Anthroponotic Cutaneous Leishmaniasis (ACL) in Children
- 1. Department of dermatology, Kerman University of Medical Sciences, Iran
- 2. Department of pathology and stem cell research, Kerman University of Medical Sciences, Iran
Abstract
Cutaneous leishmaniasis is the most common type of old world leishmaniasis which is caused by leishmaniatropica (ACL) and leishmania major (ZCL). Pediatric livings in endemic areas of leishmaniasis are most vulnerable to the infection because of absence of immunity against the parasite and early exposure to the infection. Previous studies have been demonstrated that 60-70% of CL cases have age of under 19 years old. Lesions in pediatric are mostly located in head and neck area and can be misdiagnosed as bite reaction, impetigo and foreign body granuloma. The most common diagnostic method for leishmaniasis in children is slit skin smear. Pathological features of leishmaniasis is depends on parasite species, load of inoculation, duration of the lesion and host immune response. In acute CL diffuse infiltration of histocytes and lymphocytes with few plasma cells is seen. In chronic CL granulomatous infiltration of epithelioid histocytes with lymphocytes and plasma cells is observed in superficial and deep dermis. In pediatric, first-line of treatment is intralesional pentavalent antimonial. Nowadays, oral and topical formulations such as niosomal topical zinc sulphate, topical paromomycin, oral terbinafin is prescribed increasingly, because of absence of pain and acceptable efficacy.
Keywords
- Leishmaniasis
- Children
- Epithelioid histocytes
- Host immune response
Citation
Meymandi SS, Aflatoonian M, Khalili M, Dabiri S (2018) Anthroponotic Cutaneous Leishmaniasis (ACL) in Children. Arch Paediatr Dev Pathol 2(1): 1020.
INTRODUCTION
Leishmaniasis is a protozoan parasitic infection which is caused by genus of leishmania with nearly 20 different species. Infection is transmitted by bite of infected female sand fly, phelebotumous and reservoirs of the infection are humans, rats and dogs [1,2]. Leishmaniasis is classified to cutaneous, mucocutaneous, localized lymphadenitis and visceral types depend on species. Cutaneous form is the most common type, represent 50%- 75% of new cases. Less common types of leishmaniasis are diffuse, disseminated, lupoid (recidivans), post -kala-azar dermal leishmaniasis .world health organization (WHO) classify Leishmaniasis to old world and new world. The most common types of cutaneous leishmaniasis in new world is caused by Leishmaniamexicana and in old world by leishmania tropica (L. tropica) and leishmania major (L. major) [1,3]. Cutaneous leishmaniasis is seen in all age group but children are at greater risk due to lower immunity [4].
Nearly 350 million people in 98 countries are at the risk of infection and 12 million people are affected by leishmaniasis worldwide. Based on WHO 2 million people are infected per year [1,2,4]. Infection is seen in both old world (southern Europe, Africa, and Asia) and new world (Latin America). Approximately, 90% of CL is located in Afghanistan, Iran, Pakistan, Syria, Saudi Arabia, Algeria, Colombia, morocco, Peru, Tunisia and turkey [5,6].
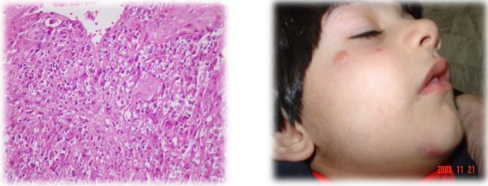
Iran is an endemic area for CL .Incidence rate of leishmaniasis in Iran is 30.9 per 100,000 people, annually. Most of the infection is located in central part of country and maximum incidence is in autumn season (35.14%) [7,8].The most common leishmania species in Iran is L. major (50.2%) and the most common type of CL is wet type (43.3%). Sporotrichoid and lupoid forms have the least prevalence (0.1 %, 0.2%, respectively). Leishmaniasis is seen most frequently in 0-4 years old (35.8 per 100,000 people) and 5-9 years old (32.5 per 100,000 people) [9]. In our area, Kerman, in south east of Iran, the most common type is Dry type cutaneous Leishmaniasis or urban type or anthroponotic cutaneous leishmania (ACL) has varied clinical features based on parasite load and host immune system [5,10]. After incubation period of 2 weeks to several months, a popular lesion is developed in the place of bite. Figure 1, and then gradually enlarged until a plaque or nodule developed Figure 2. Duration of ACL type is usually longer and can be healed after 1- 2 years ending in disfiguring scarFig6 or persisted for more than 1-2 years as chronic lupoid and chronic nonlupoid form [1].
Figure 1 Acute Leishmaniasis as papule and nodular lesions with diffuse lymphohistiocytic infiltration with many Leishman body.
Figure 2 Acute Leishmaniasis as papule and nodular lesions with diffuse lymphohistiocytic infiltration with many Leishman body.
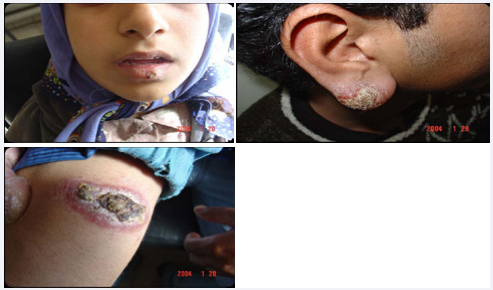
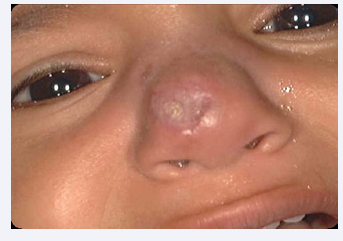
Development of red-brown or yellowish-brown papule or nodule in periphery of previous scar of leishmaniasis is called chronic lupoid (recidivans) (Figure 3) form that is usually caused by L. tropica and is refractory to treatment [3]. Chronic nonlupoid which is very rare in children is defined as persistent of acute type after 2 years as ulcer, erysepeloid, indurated plaque, psoriasiform and other various forms. Diffuse (anergy) form of leishmaniasis is presented as multiple non-ulcerated papules and nodules. This rarely form of leishmaniasis is caused by L. aethiopica and L. tropica and most frequently is seen in immunosuppressive patients. There is no visceral involvement in this type and it is associated with recurrent relapse and poor response to treatment [3,11]. Disseminated form of leishmaniasis is presented as generalized distribution of ulcerated papules, plaques and nodules in immunosuppressive patients. This form is associated with involvement of visceral organs and has poor prognosis with high mortality rate [3,12]. Sporotrichoid form is characterized with development of multiple nodules along the lymphatic. Atypical presentations of ACL including eczematoid, psoriasiform, hyperkeratotic (Figure 4), verrusiform, zosteriform, cheilitis (Figure 5), perleche, furunculoid, chancriform and erysipeloid forms that has been reported as case reports [3,13].
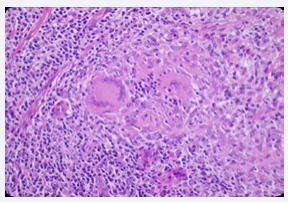
Figure 3 Chronic lupoid leishmaniasis with histological changes as non necrotizing granulomatous reaction.
Figure 5 It shows the scar of Acute Leishmaniasis.
Pediatric livings in endemic areas of leishmaniasis are most vulnerable to the infection because of absence of immunity against the parasite and early exposure to the infection. Previous studies have been demonstrated that 60-70% of ACL cases have age of under 19 years old [2,5]. Furthermore, children less than 5 years old have infection with longer duration and higher percentage of chronic lupoid form because of immaturity of immune system. In most of the studies, male have higher prevalence of infection. Lesions in pediatric are mostly located in head and neck area and they are ulcerated in 50%-60% of the cases. With increased in age in pediatric, lesions were located most frequently in trunk and limbs .Multiple lesions has been reported in 8.4% to 48.7% of the cases. Most common type of ACL in childhood was acute CL. Sporotrichoid and lupoid types have lower frequency in children [14-17]. Differential diagnosis in acute ACL mostly misdiagnosed as insect bite, furunculosis, ecthyma, pyoderma, impetigo and foreign body granuloma. Chronic ACL can misdiagnose as atypical mycobacteria, tuberculosis cutis, deep fungal infection, sarcoidosis, keloid and lupus vulgaris. Diffuse type can be misdiagnosed as lepromatous leprosy [4,12].
The most common diagnostic method for leishmaniasis is slit skin smear from the active border of the lesion that is a simple and rapid method for detection of leishmania parasite (Figure 6). This method is painless, so especially suitable for children. Smear is usually positive in 50%-80% of cases. Lesions with short period of development are more likely have positive result [3,18]. Skin biopsy is another method for diagnosis of leishmaniasis that is diagnostic nearly in 50%-70% of cases. In ACL numerous leishman body can be detected in macrophage and extra-cellular areas, but in chronic lupoid and chronic nonlupoid forms usually have scarce number or no leishman body. So, histopathology in ACL is more confirmatory. Wright-Gimsa stain can be used for better detection of leishman bodies that is stains cytoplasm and nucleus of amastigote blue and red, respectively. Culture of parasite in (NNN) media has sensitivity of 85% that should be read after 4 weeks. Because, this method requires long period of time to confirm the diagnosis, it is not suitable for diagnostic method. Polymerase chain reaction (PCR) is a highly specific (100%) and sensitivity (90. %) method, but is expensive. The major advantage of PCR is rapid result in 24 hours [3,19].
Figure 6 It shows the Slit skin smear of Leshmaniasis.
Fine needle aspiration (FNA) is suitable in children because of less aggressiveness of procedure and relative lack of pain. Sensitivity of this method is varied depend on expertise of laboratory personnel. Extracted sample can be send for culture or PCR examination [3,18,19].
Montenegro skin test is done by intra-dermal injection of killed promastigote. Test is positive if induration more than 5 mm after 72 hours in the site of injection. Test is usually positive in ACL after 3months of inoculation but negative in diffuse type. Furthermore, test has less validity in endemic areas, because it can not differentiate between acute ACL and previous exposure to leishmaniasis [3,18,19].
Balance between T-helper1 T H1 and TH2 response in immune system has essential role in resolution or progression of leishmaniasis lesions. Increased level of cytokines associated to TH1 including interleukin IL1, IL-2, IL-12, IL-18, IL-23, tumor necrotizing factor-α (TNF-α) and interferon (IFN) Gama lead to resolution of lesions. In diffuse and lupoid types of CL marked level of cytokines related to TH2 (IL-4, IL-5, IL-10, IL-13) and transforming growth factor (TGF)-β are reported .Cytokines related to TH1 leads to activation of natural killer(NK)cells and macrophages that results to production of nitric oxide and other free radicals and killing of intra-cellular parasite. Moreover, production of IL12 by antigen presenting cells and increase TH1 lead to increased level of TNF-α and more activation of macrophages. On the other hand, increased level of cytokines related to TH2 in non-healed types of CL lead to increase antibody production against parasite and inactivation of macrophages [19,20].
The histological spectrum of ACL classify to 4 groups (Azadeh histopathologic classification) as I- Anergicmacrophagic reaction heavily parasitized II- Focalized histiocytic reaction variable parasitized III- Diffuse necrotizing reaction variable parasitized IV- Diffuse lymphoyjygiygiyiiiuuihistiocytic reaction variable parasitizedV- Lupoid granulomatous reaction no parasitized [20]. Clinically it does not constitute a clinico-pathological correlation and is simply a stage in the chronological development of DCL lesions. Chronic lupoid leishmaniasis (CLL) resembles lupus vulgaris. The lesions are characterized by non-caseating epithelioid granulomata and organisms are absent or extremely scanty [21].
In one study in Iran on L. tropica granulomatous infiltration is seen most frequently in chronic lupoid and chronic nonlupoid form of CL than acute CL (38.6% of acute CL, 55.6% of chronic NLCL and 66.7% of chronic LCL). Al l of the granulomatous infiltration in this study was without necrosis. Furthermore, acanthosis, Psudoepitheliomatosis hyperplasia, multinucleated giant cell giant cells and fibrosis were observed most frequently in chronic form of CL. CD4 and CD8 T lymphocytes were infiltrated in both acute and chronic form [22].
In another study in turkey histological features of CL were evaluated. In this study, the most common epidermal findings were liquefaction degeneration of the basal cell layer (69.6%). Pseudoepitheliomatous hyperplasia, epidermal atrophy and acanthosis were seen in 24.2%, 27.2% and 18.1% of the cases. Ulceration and crust formation were observed in 33.3% and 18.1% of the cases. Moreover, histiocytes and lymphocytes were observed in 100% of the cases. Plasma cells, eosinophils and Langhan’s type giant cells were seen in 84.8%, 42.4% and 27.2%23.In acute CL parallel increase in CD68 macrophage cells and CD1a+ epidermal dendritic cells (DC) is seen. In lupoid type parallel increase in CD1a+ epidermal DC and CD1a+ dermal DC were observed [24].
Management of ACL depends on clinical features of the disease. If the number of the lesions become more than 4, location of the lesion be on face, fingers, toes, joints, genitalia with failure of local therapy, lupoid, diffuse or disseminated forms and in immunocompromised host, systemic therapy including pentavalent antimonial, amphotericin B, pentamidine, azoles, miltefosine are recommended . Simple type of leishmaniasis can be treated with local therapy including intralesional injection of pentavalent antimony, cryotherapy, heat therapy, topical paromomycin, and photodynamic therapy. Combination therapy is more effective than single therapy. In pediatric, first-line of treatment is combination of intralesional pentavalent antimonial with cryotherapy. Nowadays, oral and topical formulations such as niosomal topical zinc sulphate, topical paromomycin, oral terbinafin are reported to be effective with the advantage of absence of the pain [3,25-28].