Importance of Transesophageal Echocardiography for Stroke Prevention in Patients Undergoing Coronary Artery Bypass Graft Surgery - Case Report
- 1. Department of Anesthesia, Indiana University School of Medicine, United States of America
Abstract
Transesophageal echocardiography (TEE) has become routine during cardiovascular and thoracic anesthesia. It plays a key role in surgical planning and provides vital hemodynamic information intraoperatively. A 61-year-old female undergoing coronary artery bypass graft surgery, in which an intraoperative TEE was performed. Subsequently, a left atrial appendage thrombus was discovered. The case was postponed allowing for adequate anticoagulation. Successful CABG was performed after outpatient TEE determined the resolution of the left atrial appendage thrombus. The use of TEE intraoperatively stresses the importance of stroke prevention in patients undergoing high-risk surgeries.
Keywords
• Transesophageal echocardiography; Left atrial appendage; Atrial fibrillation; Stroke; coronary artery bypass graft; Spontaneous echo contrast
CITATION
Raniwsky A, Moseman A, Carmony M (2022) Importance of Transesophageal Echocardiography for Stroke Prevention in Patients Undergoing Coronary Artery Bypass Graft Surgery - Case Report. Int J Clin Anesthesiol 10(1): 1114.
ABBREVIATIONS
TEE: Transesophageal echo; CABG: Coronary Artery Bypass Graft; LAA: Left Atrial Appendage; SEC: Spontaneous Echo Contrast
INTRODUCTION
Perioperative stroke is amongst the most unwanted outcomes for patients and physicians. In high-risk cardiac surgeries, the use of TEE can recognize a thromboembolic source which ultimately can decrease patient morbidity and mortality
CASE PRESENTATION
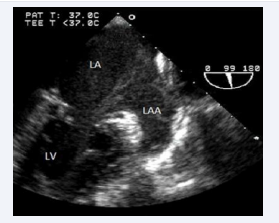
A 61-year-old female with a past medical history of hyperlipidemia and multivessel coronary artery disease presented for elective Coronary Artery Bypass Grafting (CABG) surgery. The patient had a strong family history of coronary artery disease and her father had atrial fibrillation however, the patient herself had no such diagnosis. The patient was brought to the operating room where an awake right radial artery arterial line was placed, and eventually underwent induction with propofol and rocuronium. Her airway was secured with an endotracheal tube, large-bore intravenous access was obtained, and a triple lumen central venous catheter was placed in the right internal jugular vein. A transesophageal echo (TEE) was performed. While obtaining imaging during the mid-esophageal two-chamber view, a thrombus in the patient’s left atrial appendage (LAA) was noted (Figure 1).
Figure 1: Mid esophageal two-chamber view on TEE, left atrial appendage (LAA) thrombus (Arrow). Left Atrium (LA), Left Ventricle (LV), Mitral Valve (MV).
The case was subsequently canceled, and the patient was discharged home on daily apixaban. After six weeks of anticoagulation, the patient underwent outpatient TEE that revealed resolution of the LAA thrombus. The patient proceeded with elective CABG and was discharged home with an uneventful postoperative course.
DISCUSSION
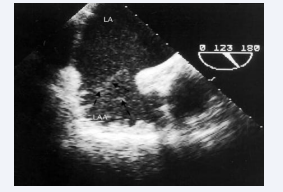
Stroke is one of the most unwanted outcomes of cardiac surgery both for patients and physicians alike. The risk of perioperative stroke has been reported up to 10% in patients undergoing high-risk brain surgery or cardiac surgery, such as CABG [1]. Perioperative stroke can lead to decreased quality of life as well as increased mortality. In addition to increased mortality and morbidity, perioperative complications of CABG have been estimated to cost over $2 billion annually worldwide [2]. Stroke prevention should be at the forefront of a practitioner’s mind when undergoing high-risk surgeries. One of the biggest risk factors for stroke is atrial fibrillation [3]. Postoperative atrial fibrillation occurs in up to 30% of CABG patients and is associated with an increased risk of stroke [4]. The LAA is a small, pyramidal structure, which is situated on the lateral aspect of the left atrium (LA), extending between the pulmonary artery above and the left ventricle (LV) below (Figure 2) [5].
Figure 2: Mid esophageal two-chamber view on TEE, left atrial appendage (LAA), Left Atrium (LA), Left Ventricle (LV).
This is the most prominent site of thrombus formation, with more than 90% of thrombi generated within this anatomical structure [6]. Identification of individuals at risk of perioperative stroke is increasingly important to assess the risk and benefit of CABG and to develop strategies to mitigate the risk of stroke whenever possible. One strategy to mitigate risk is the use of perioperative TEE [7]. To examine the LAA with TEE, two standard mid-esophageal views are acquired during a study. These views are the short axis aortic valve (30-60 degrees), and the two-chamber (80-100 degrees) view (Figure 2) [8]. TEE is also helpful in the detection of LAA spontaneous echo contrast (SEC). SEC is a smoke-like swirling pattern seen on two-dimensional imaging and is thought to reflect rouleaux formation resulting from the stasis of the blood. Understandably, SEC is the harbinger of thrombus formation and therefore, a predictor of thromboembolic risk [9] (Figure 3).
Figure 3: left atrial appendage (LAA), Left Atrium (LA), Spontaneous Echo Contrast (Arrows)
The presence of spontaneous echo contrast in the left atrium and left atrial appendage has been associated with a higher risk of thromboembolism and cerebrovascular accident [10]. Current guidelines recommend TEE be used for all open heart and thoracic aortic procedures and its use should be considered in CABG [10]. TEE serves as a crucial tool in the monitoring, diagnosis, and management of patients undergoing CABG (or other high-risk surgeries). TEE can be utilized to assess cardiac sources of emboli, assess for valvular dysfunction, and visualize the LAA for possible thrombus [10].
CONCLUSION
Identification of pathology on TEE can change operative planning and decrease adverse patient outcomes, including stroke. Applications for TEE in perioperative settings are expanding and more research is needed to fully understand the value of TEE in perioperative stroke prevention.
ACKNOWLEDGEMENTS
The Authors thank the Indiana University School of Medicine.