Do Scapular Kinematics Alter during the Performance of the Scapular Assistance Test and Scapular Retraction Test: A Pilot Study
- 1. Shoulder Center of Kentucky, Lexington Clinic Orthopedics, USA
- 2. Department of Rehabilitation, University of Kentucky, USA
Abstract
Objective: To describe to what degree and in what plane biomechanical alterations occur during the performance of the Scapular Retraction test (SRT) and Scapular Assistance Test (SAT).
Design: Laboratory Pilot Study
Participants: Eight symptomatic and 7 asymptomatic subjects were instrumented with electromagnetic sensors. Main Outcome Measures: The SRT and SAT were performed with the scapula stabilized and unstabilized. The scapular kinematic variables of posterior tilt, internal rotation, upward rotation, protraction, and elevation were measured during both tests.
Results: Descriptive analysis of scapular kinematics suggested that posterior tilt was primarily increased during both clinical tests in both groups. Both groups decreased in scapular elevation, indicating that the scapula was being depressed during the SRT. There was no meaningful change in force during the SRT.
Conclusion: These findings indicate that both the SRT and SAT appear to alter scapular motion in both groups. The interpretations of these results are limited due to the small sample size and large confidence intervals, but suggest that these tests change specific positions of the scapula. Further research into these tests is needed to confirm these biomechanical alterations, and to determine the value of these tests when developing rehabilitation protocols in patients with shoulder pain.
Keywords
Physical examination; Biomechanics; Scapular dyskinesis
Citation
Ben KW, Cunningham TJ, Myers NL, Uhl TL (2016) Do Scapular Kinematics Alter during the Performance of the Scapular Assistance Test and Scapular Retraction Test: A Pilot Study. JSM Anat Physiol 1(1): 1005.
Abbreviations
SRT: Scapular Retraction Test; SAT: Scapular Assistance Test; ISB: International Society of Biomechanics’; UR: Upward Rotation; PT: Posterior Tilt; IR: Internal Rotation; Nm: Newton Meters
Introduction
Multiple tests are administered by physicians and clinicians to diagnose and assess shoulder dysfunction. Two particular tests that have been described to evaluate scapular dysfunction are the scapular retraction test (SRT) and the scapular assistance test (SAT) in patients with shoulder pain [1-3]. The most commonly described scapular dysfunction is scapular dyskinesis which is an alteration in the normal position or motion of the scapula during coupled scapulohumeral movements [4]. Scapular dyskinesis has been reported to be present in approximately 70% of shoulder injuries, [4] and is thought to be caused by multiple factors, one of which is muscular inhibition involving the muscles surrounding the scapula and shoulder joint [5]. Scapular dyskinesis appears to be a nonspecific response to shoulder dysfunction because no specific pattern of dyskinesis is associated with a specific shoulder diagnosis [2,6,7]. Clinical experience of the authors using the SRT and SAT as part of the clinical exam has indicated that the application of these corrective maneuvers assists in manually improving control of the scapula which seems to increase shoulder strength, decrease shoulder pain, and improve function, and may assist clinicians in the selection of therapeutic interventions designed to target scapular mobility and neuromuscular control.
The SRT has been thought to improve isometric shoulder strength as this clinical maneuver ensures that the scapula is acting as a stable base for the rotator cuff muscles by promoting scapular retraction [1]. This concept can be further supported as relationships between shoulder strength and scapular motion have been previously investigated, revealing that scapular protraction is correlated with decreases in shoulder rotation strength [8]. Furthermore, previous research has demonstrated significant isometric strength outputs while utilizing scapular retraction during manual muscle testing of the arm [1,9]. However, no study has previously quantified scapular kinematics during the SRT test. The SAT has been theorized to improve scapular motion by assisting the scapula into upward rotation; thus, optimizing the force-couple relationship between the serratus anterior and lower trapezius [5]. Previous biomechanical studies have demonstrated increased scapular upward rotation and posterior tilt in healthy and pathological patients suffering from subacromial impingement syndrome and/or scapular dyskinesis [9,10]. Both of these studies assessed the SAT statically at varying degrees of humeral elevation. However, the SAT is a dynamic test, and to date, has not been investigated as originally described [2].
Both of these clinical tests require the clinician to apply mechanical forces to the scapula while the patient reports change in symptoms. However, the plane of motion and degree of scapular kinematic alterations is currently unknown for the SRT and SAT when performed dynamically. Therefore, this pilot study will record scapular motion in both symptomatic and asymptomatic subjects. Scapular motion was recorded three-dimensionally in order to determine the amounts of change occurring during the performance of these clinical tests and to what plane scapular kinematics is most altered.
Materials and Methods
Subjects
Participants in this study included symptomatic and asymptomatic participants. Symptomatic participants were recruited from a sample of convenience and symptomatic subjects were enlisted from one orthopedic surgeon’s practice in Lexington, KY. The participant population consisted of 8 symptomatic shoulders (age=25 ± 8yrs) and 7 asymptomatic shoulders (age=34±14yrs). Subjects were included in the symptomatic group if the orthopedic surgeon determined scapular dyskinesis was present, a qualifying diagnosis was present, and at least 120° of shoulder elevation could be performed. Scapular dyskinesis was described as the presence or absence of dysfunctional movement by using a yes/no classification system [7,10]. Five of the symptomatic subjects were diagnosed as having rotator cuff tendinitis. To have rotator cuff tendonitis subjects had to have three of the following tests positive: Neer impingement sign, Hawkins-Kennedy test, a painful arc, pain with weakness during resisted abduction, or pain with weakness during resisted external rotation [11]. Combining 3 or more of the above tests has been shown to be useful in confirming subacromial impingement [11]. Three of the symptomatic subjects were diagnosed as having superior labral pathology. To have superior labral pathology at least two of the following were present: popping or clicking in the shoulder, positive active compression test, anterior slide, or modified dynamic labral shear test [12]. Individuals in the asymptomatic group were included if there was no current shoulder pain or limited range of motion at the shoulder. Exclusion criteria for both the symptomatic and asymptomatic groups consisted of a history of central nervous system disorder, peripheral neuropathy, previous history of traumatic shoulder injury or surgery, or allergies to adhesive products. All subjects read and signed informed consent approved by the University of Kentucky Institutional Review Board prior to participation.
Set-up
The subjects were instrumented with receivers from a 3D electromagnetic tracking device, the Flock of Birds (Ascension Technologies, Burlington, VT) in a clinical laboratory. Motion Monitor software (Innovative Sports Programs, Chicago, IL) recorded 3D position and orientation of each subjects’ thorax, scapulae, and humerus at 100Hz. Three receivers were applied with two-sided adhesive tape and secured with CoverRoll (Beiersdorf, Norwalk, CT), one to the sternum, just inferior to the jugular notch, one to the involved scapula (dominant scapula for healthy subjects), and one attached to ipsilateral humerus using a custom made thermoplastic cuff (Orthoplast, Johnson & Johnson, New Brunswick, NJ). The scapular receiver was placed on the flattest portion of the posterior acromion to reduce skin movement artifact [13]. Placement of the scapular sensor on the posterior acromion location has been validated with bone pin studies [14,15].
Global coordinate system was established with an extended range transmitter (Ascension Technologies, Burlington, VT) on a wooden base 60 inches above the ground. The transmitter was aligned with the cardinal planes of the body. The subjects stood with their arms relaxed by their sides while the bony landmarks on the thorax (jugular notch, xiphoid process, C7, T8, T12), scapula (inferior angle, root of scapular spine, posterior acromial angle), and humerus (medial epicondyle, lateral epicondyle, and center of humeral head) were digitized to record motions of the upper extremity. The center of the humeral head was determined using the sphere-fitting protocol provided within the Motion Monitor software [16]. We followed The International Society of Biomechanics’ (ISB) standardized protocol defining coordinate systems and Euler rotation sequences for upper extremity motion [17]. This procedure has produced reliable measures, with intraclass correlation coefficient (2,1) values ranging between .77-.90 with a standard error of measure of less than 2° [18]. Assessment of skin movement error was carried out in pilot testing as the two scapular tests require manipulation of the scapula, which may alter scapular kinematic measures. Seven subjects underwent pilot testing to address this potential error prior to starting the study. Instrumentation of the subjects was the same as described above. A recording was made with the arm at 90° . The examiner then placed his hand and forearm on the subject as would be performed during SRT test, and the kinematic data was recorded again. The difference between the two measures for the five scapular kinematic dependent measures was determined for each subject and averaged across all seven subjects. The same procedure was carried out for the SAT with the arm at rest using the two hand position: one on the inferior angle the other over the upper trapezius of the instrumented shoulder as previously reported [2]. The mean amount of skin movement due to hand placement for each scapular motion did not exceed 1.6(Table 1).
Table 1: Skin movement artifact due to hand placed on the scapula during each test is reported with respective mean (standard deviation). These data are reported as the change score by placing the hand on the scapula to perform the test.
| Internal Rotation | Upward Rotation | Posterior Tilt | Protraction | Elevation | |
| Scapular Assistance Test | -0.005 (1.5°) | 0.36 (1.7°) | 0.02 (1.7°) | -0.3 (1.4°) | -0.6 (1.0°) |
| Scapular Retraction Test | -0.42 (1.9°) | 1.3 (2.4°) | 1.05 (2.4°) | -1.4 (2.4°) | -1.6 (1.4°) |
The subjects’ resting kinematic data were recorded for 5 seconds and served as a reference for scapular kinematics recorded during dynamic motion. All data were recorded as a change score from this reference position. All subjects’ were asked to stand in their normal resting posture with their arms at their side, thumbs pointing forward. The dependent measure of scapular internal rotation (IR), posterior tilt (PT), upward rotation (UR), protraction, and elevation were calculated for all testing as previously described by Myers et al [19].
Scapular Retraction Test
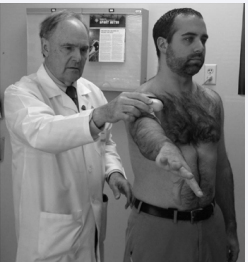
The Scapular Retraction Test was performed as previously described in the literature in two steps [1,2] The subjects were asked to elevate their arm to 90° in the scapular plane with their arm internally rotated such that their thumb was pointing downward toward the floor. Subjects’ were asked to maximally push up against resistance for 3 seconds. Resistance was applied just above the elbow with a hand held dynamometer (J Tech Medical, Salt Lake City, UT) as previously described (Figure 1) [1].
Figure 1: Scapular Retraction Test. The examiner manual muscle tests the arm in a position of forward flexion.
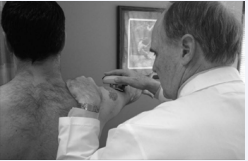
This procedure occurred twice and the average scapular kinematic data were recorded as a change from resting reference values. The scapular angular motions were measured during the test and were named “unstabilized scapula”. The second step was for an examiner to manually stabilize the scapula in a position of retraction (Figure 2).
Figure 2: The same scapula test is performed with the medial border of the scapula stabilized.
Care was taken to keep the examiner’s arm as far away from the scapular receiver as possible to minimize movement artifact without disrupting the hand placement of the test as originally described [2]. This position attempts to stabilize the scapula and therefore was named “stabilized scapula”. Subjects were instructed to maximally elevate their arm against static resistance for 3 seconds. This was repeated twice and the average scapular kinematic data were recorded as a change from resting reference values. Average torque values in both conditions were recorded for later analysis.
Scapular Assistance Test
The Scapular Assistance Test was performed as previously described in the literature [2]. The subjects were asked to elevate the instrumented arm overhead as far as possible in the scapular plane. A guide was used to keep the arm at 45° relative to the frontal plane. Arm elevation of all subjects was performed with no assistance and repeated twice. Data was extracted for all scapular dependent measures (UR, PT, IR, clavicular protraction, and clavicular elevation) at 30°, 60°, 90°, and 120°. The average of the two trials was used and this condition was named unstabilized scapula.”Next, subjects repeated the arm elevation motion while the scapular assistance test was performed. Scapular assistance was provided by manually applying an anterior and lateral force to the scapula with the examiner’s thumb on the inferior angle of the scapula as the arm was elevated. The examiner’s opposite hand was placed over the upper trapezius as previously described [2]. Data was extracted for all scapular dependent measures at 30°, 60°, 90°, and 120°. The average of the two trials was used and this condition was named “stabilized scapula.”
Data Reduction
The standing resting position was used as the scapular kinematic reference value to determine changes between the two conditions (unstabilized and stabilized) during both the SRT and SAT. The scapular kinematic change values (reference value – unstabilized condition value) and (reference value – stabilized condition value) were used for descriptive analysis to account for the variances in resting scapular position. We chose to use this approach because previous research has shown large variations in resting scapular position during humeral elevation for all 5 dependent measures in this study [20,21]. We compared the resting scapular kinematic values between groups using the Mann-Whitney Test, to confirm that our correction was not biased. The analysis revealed no differences in resting scapular kinematic values between symptomatic from asymptomatic shoulders (Table 2).
Table 2: This table provides descriptive analysis of scapular kinematics at rest during the SRT with mean and 95% confidence intervals (lower boundary, upper boundary). The P-Value represents the probability from the Mann-Whitney Test that compared the two groups.
| Asymptomatic | Symptomatic | P-Value | |
| Resting/Reference Position | |||
| Internal Rotation (°) | 25 (13.7, 35.5) | 19 (2.1, 36.8) | 0.91 |
| Posterior Tilt (°) | −13 (-18.7, -7.1) | −11 (-13.3, -9.3) | 1.00 |
| Upward Rotation (°) | −2 (-9.3, 4.8) | 0.15 (-6.3, 6.7) | 1.00 |
| Protraction (°) | −25 (-36.3, -14.1) | −37 (-56.0, -17.2) | 0.30 |
| Elevation (°) | 7 (-4.8, 19.6) | 0.38 (-27.1, 27.9) | 0.49 |
Data Analysis Descriptive statistics were generated in order to investigate the change in scapular kinematics between the unstabilized and stabilized scapular condition for both tests. The average relative change values and 95% confidence intervals were used due to the nature of this being a pilot study, and the fact that we have a low number of subjects. The goal of this study was to determine if scapular kinematic alterations were occurring and in which direction during the performance of the SRT and SAT in both symptomatic and asymptomatic subjects. The confidence intervals provide an estimate of the probability that the actual scapular kinematic changes for each measure will fall within this limit, even if a larger sample size was recruited. For the purpose of this study, if dependent measures confidence intervals had overlapping boundaries between unstabilized and stabilized condition we would interpret that there is likely no change in scapular kinematics for a particular plane for that dependent measure. Further, if the dependent measures’ confidence boundaries do not overlap, we would interpret that there is likely a meaningful change occurring. Descriptive strength measures (means and 95% confidence intervals) for both groups of subjects were generated with the scapula unstabilized and then stabilized during the SRT applying the same interpretation.
Results
Stabilizing the scapula during the scapular retraction test increases posterior tilt in both the asymptomatic and symptomatic group by 11° and 9° , respectively. The distinct separation between the upper and lower boundaries of the 95% confidence intervals is likely the result of meaningful increases to posterior tilt. Meaningful decreases on average of 10° were present in elevation in both groups during the SRT despite the minimal overlap in the confidence boundaries of the asymptomatic group (Table 3).
Table 3: This table provides the relative mean change from resting scapular position during the performance of the Scapular Retraction Test with 95% confidence intervals (lower boundary, upper boundary) representing the variability of change scores for both groups. The SRT is performed with the arm abducted to 90° in the scapular plane with the arm internally rotated.
|
Asymptomatic |
Unstabilized Scapula |
Stabilized Scapula |
|
Internal Rotation (°) |
6 (-1.8, 14.2) |
-2 (-11.0, 6.6) |
|
Posterior Tilt (°) |
4.8 (1.3, 8.4) |
16.7 (9.5, 23.8) |
|
Upward Rotation (°) |
13.1 (6.9, 19.4) |
16.8(6.2, 27.3) |
|
Protraction (°) |
-0.7 (-7.5, 6.1) |
-6.2 (-14, 1.5) |
|
Elevation (°) |
8.4 (5.1, 11.8) |
-0.3 (-7.6, 7.0) |
|
Symptomatic |
|
|
|
Internal Rotation (°) |
8.8 (0.1, 16.6) |
1.7 (-7.4, 10.1) |
|
Posterior Tilt (°) |
6.1(1.4, 10.8) |
15.4 (10.2, 20.6) |
|
Upward Rotation (°) |
18.4(13.6, 23.2) |
13.9 (7.7, 20.2) |
|
Protraction (°) |
4.3 (-6.0, 14.6) |
0.5 (-10.1, 11.1) |
|
Elevation (°) |
13.8 (8.4, 19.2) |
1.5 (-5.1, 8.2) |
There were overlaps in confidence boundaries for the stabilized and unstabilized conditions for all other dependent measures.
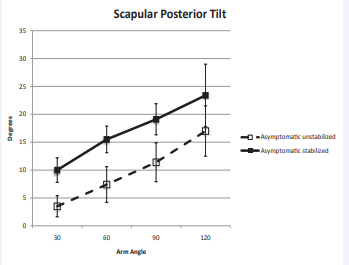
The SRT did not generate meaningful changes in torque in either of the groups when examining the boundary limits of the 95% confidence intervals. The asymptomatic group demonstrated meaningful improvements in posterior tilt between the two scapular conditions at 30° , 60° , and 90° of humeral elevation as confirmed by separated confidence boundaries (Figure 3).
Figure 3: Represents scapular posterior tilt in asymptomatic participants with the scapula unstabilized and stabilized during the SAT across arm angles. These data are represented by the mean and 95% confidence interval (lower boundary, upper boundary). No overlap in confidence intervals indicates meaningful changes in scapular motion.
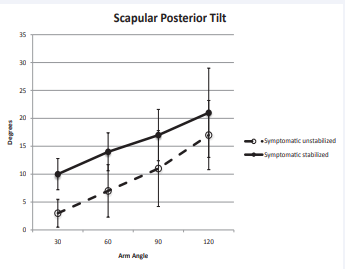
The symptomatic group displayed greater variability in posterior tilt as demonstrate in Figure (4).
Figure 4: Represents scapular posterior tilt in symptomatic subjects with the scapula unstabilized and stabilized during the SAT across arm angles. These data are represented by the mean and 95% confidence interval (lower boundary, upper boundary). No overlap in confidence intervals indicates meaningful changes in scapular motion.
Table 4: This table provides torque data represented in Newton Meters (Nm) as means with 95% confidence intervals (lower boundary, upper boundary) in both asymptomatic and symptomatic groups with the scapula unstabilized and again with the scapula stabilized during the SRT.
|
|
Unstabilized Scapula |
Stabilized Scapula |
Change in Torque |
|
Asymptomatic |
47.1 (27.5-66.7) |
48.5 (30.1-66.8) |
1.4 (-4.5-7.4) |
|
Symptomatic |
29.5 (15.2-43.8) |
29.9 (16.1-43.6) |
0.4 (-3.5-4.3) |
There was an average change between the unstabilized to stabilized scapula during the SAT of 7° between each arm angle in both groups (Table 5).
Table 5: This table provides the relative mean change from resting scapular position during the performance of the Scapular Assistance Test (SAT) with 95% confidence intervals (lower boundary, upper boundary) representing the variability of change scores for both groups. The SAT is performed with the subject actively elevating their arm in the scapular plane up to 120° of elevation.
|
|
Unstabilized Scapula |
Stabilized Scapula |
||||||
|
Asymptomatic |
30° |
60° |
90° |
120° |
30° |
60° |
90° |
120° |
|
Internal Rotation (°) |
-0.8 (-5.6, 4.0) |
1.4 (-4.4, 7.1) |
3.9 (-2.6, 10.4) |
5.2 (-2.5, 13.1) |
-0.5 (-7.5, 6.4) |
2.8 (-4.9, 10.4) |
5.1 (-2.4, 12.7) |
6.1 (-3.1, 15.3) |
|
Posterior Tilt (°) |
3.5 (1.6, 5.4) |
7.4 (4.2, 10.6) |
11.4 (7.9, 15.0) |
17.0 (12.3, 21.5) |
10.1 (7.9, 12.2) |
15.5 (13.2, 17.9) |
19.1 (16.1, 22.0) |
23.4 (17.8, 29.0) |
|
Upward Rotation (°) |
5.0 (0.4, 9.6) |
11.3 (5.6, 19.9) |
18.5 (11.5, 25.5) |
24.1 (14.6, 33.7) |
5.4 (-0.4, 11.1) |
11.1 (4.7, 17.4) |
16.1 (8.8, 23.5) |
20.2 (10.6, 29.8) |
|
Protraction (°) |
-1.1 (-5.1, 2.8) |
-1.1 (-6.1, 3.9) |
-1.5 (-7.6, 4.6) |
-2.8 (-9.7, 4.2) |
-0.5 (-6.8, 5.9) |
0.4 (-6.2, 7.1) |
0.8 (-6.0, 7.7) |
-0.5 (-7.3, 6.2) |
|
Elevation (°) |
1.3 (-2.1, 4.7) |
3.4 (-0.6, 7.4) |
7.0 (2.8, 11.2) |
9.0 (5.0, 13.1) |
-0.9 (-4.3, 2.3) |
-0.1 (-3.6, 3.4) |
1.3 (-3.0, 5.7) |
3.4 (-1.2, 8.0) |
|
Symptomatic |
|
|
|
|
|
|
|
|
|
Internal Rotation (°) |
0.3 (-2.5, 3.1) |
2.5 (-0.9, 6.0) |
5.0 (-0.2, 12.2) |
8.6 (0.4, 16.8) |
0.1 (-3.1, 3.3) |
2.4 (-1.0, 5.8) |
5.6 (0.5, 10.7) |
8.4 (-0.7, 17.4) |
|
Posterior Tilt (°) |
3.0 (1.6, 5.5) |
7.1 (2.5, 11.7) |
11.4 (5.0, 17.8) |
16.5 (9.8, 23.2) |
9.7 (6.5, 12.8) |
14.2 (11.0, 17.4) |
17.4 (13.2, 21.6) |
21.3 (13.5, 29.0) |
|
Upward Rotation (°) |
2.7 (0.2, 5.2) |
9.9 (6.4, 13.4) |
18.6 (13.3, 24.1) |
27.0 (19.9, 34.1) |
4.5 (-1.1, 10.1) |
11.0 (4.6, 17.5) |
18.1 (11.3, 24.8) |
25.6 (17.1, 34.1) |
|
Protraction (°) |
-0.4 (-5.1, 4.4) |
0.5 (-5.7, 6.8) |
1.8 (-7.2, 10.8) |
3.1 (9.2, 15.4) |
-0.7 (-8.7, 7.2) |
2.8 (-6.7, 12.3) |
5.6 (-5.4, 16.6) |
5.7 (-7.0, 18.4) |
|
Elevation (°) |
3.1 (-4.4, 10.5) |
6.1 (-1.1, 13.3) |
10.5 (2.0, 19.0) |
13.8 (5.8, 21.8) |
-13.0 (-27.9, 1.9) |
-11.0 (-25.3, 3.2) |
-7.2 (-21.3, 6.8) |
-1.2 (-15.7, 13.5) |
There were overlaps in confidence boundaries for the stabilized and unstabilized conditions for all other dependent measures.
Discussion
Three-dimensional kinematic analysis quantified scapular changes to identify which planes of motion were most altered and to what degree during the SRT and SAT. We observed that during the SRT that posterior tilt was increased by approximately 9° and scapular elevation was reduced by approximately 10° in both symptomatic and asymptomatic groups. Posterior tilt was primarily affected during the SAT as there was an increase in posterior tilt throughout the arc of motion of approximately 7° in both groups. These findings support the goal of this study to determine what planes of scapular motion are most influenced by these clinical tests and to what degree. The fact that we have a small sample size and large confidence intervals must temper our interpretation of these findings. It is apparent from the large variability observed in the confidence intervals ranging from 5-30° in some cases that the amount of scapula kinematic change varies tremendously between individuals. However, the limited overlap between the confidence boundaries of posterior tilt in both clinical tests and scapular elevation in the SRT support that these tests may consistently alter scapular kinematics and thereby help clinicians determine the role of these scapular motions in altering patient symptoms.
Scapular dyskinesis is an alteration in the normal position or motion of the scapula during coupled scapulohumeral movements [4,6,22]. Scapular dyskinesis has been associated with several pathologies including but not limited to subacromial impingement, shoulder instabilities, rotator cuff tendinopathy, and adhesive capsulitis [4,23]. Scapular dyskinesis is not diagnostic of the presence of pathology but has been suggested to be an indication of impairment [7,24,25]. The utilization of the SRT and SAT are to determine if the pain or force impairment is altered, indicating that aberrant scapular motion may in part contribute to a patient’s symptoms or dysfunction [2]. These results suggest that posterior tilt is the plane of motion most affected during these tests which is reasonable as the force applied during these maneuvers is directed along the medial border and inferior angle which would mostly affect posterior tilt.
The increase in posterior tilt seen in our study agrees with previous static assessment of the SAT that identified an increase on average of 5° of posterior tilt in individuals with and without shoulder pathology [26]. There was no alteration in upward rotation during the SAT in the current study which is not consistent with previous research that identified approximately 5° increase in upward rotation during the static application of the scapular assistance test across three elevation angles (0, 45, and 90° ) [27]. The most likely explanation for the differences was that in the current study the examiner applied the force to the inferior angle by their thumb primarily in an anterior and slightly lateral direction during dynamic motion as the original SAT was described [2]. Seitz et al., employed the modified SAT described by Rabin et al., [3] which incorporated the entire hand applying pressure to the inferior medial border of the scapula which appears to alter the plane of motion affected during the SAT. It appears the two techniques yield slightly different results. The previous study was on a larger population of individuals with and without sub-acromial impingement symptoms while this study is on a much smaller population of varied diagnoses, which may also account for the lack of change in upward rotation.
Scapular retraction and elevation movement patterns are present during humeral elevation [28,29]. However, this is the first study to evaluate scapular protraction and elevation during the SRT and SAT. The stabilization of the scapula during SRT suggests approximately a 10° change in scapular elevation in both groups. We believe this to be potentially meaningful decrease due to only a 2° overlap in the asymptomatic subjects and no overlap in the symptomatic subjects when examining the confidence intervals of the relative change from resting (Table 3). The forearm position during the SRT applies pressure along the medial border creating the posterior tilt but the hand of the arm is placed over the superior border of the scapula and is likely to be pulling the scapula downward [2] This fact combined with the instruction of the patients to volitionally retract the scapula prior to elevating the arm contributes to this finding. Further biomechanical investigation of this finding is warranted. Nonetheless the large variability may explain in part why there are inconsistent findings in the force alterations during SRT testing. A trend of decreased elevation was observed during SAT but the very wide confidence intervals likely due to our small sample size in the symptomatic group preclude us from suggesting a true effect is occurring.
Previous research has reported conflicting information on the effect of strength during the performance of the SRT [1,9]. Earlier research has identified that performing the SRT may create a better environment for increasing shoulder strength in the empty can position [1]. Force has been shown to increase by 13% in healthy subjects and 24% in injured participants [1]. The current study did not produce similar strength gains, which could be due to methodological changes. However, a study comparing forty-four healthy overhead athletes to ninety-eight overhead athletes with impingement [9] had similar results to this study. Approximately 20% of these athletes had an increase in strength based off a minimal detectable change score of 9.3N [9]. Authors also discovered significant increases in normalized torque within both groups. The current study found similar results as less than a 1Nm of change in strength was identified between an unstabilized and stabilized scapula. Significant torque changes during the reposition test [9] could be multifactorial: patient population, average age of 21±3 years, large sample size, and consistent resistant patterns through the use of a mounted dynamometer. Lastly, the symptomatic subjects’ pain perception in our study with an unstabilized to a stabilized scapula did not change. This finding is in agreement with previous research that found pain is minimally influenced as isometric strength increases during the stabilized portion of the scapular retraction or reposition test [1,9]. Despite conflicting research on strength increases it is important to understand that this test does alter scapular kinematics and may increase strength depending on the level of shoulder dysfunction and the target population.
There are limitations to this study. Primarily, the sample size is small which limits interpretation of the data. We have limited the analysis of data to descriptive statistics and have used confidence intervals to interpret our findings. Certainly future research on a larger number of subjects is needed to confirm these findings. A power analysis run on data from this study to compare within group changes between unstabilized and stabilized scapula during the SRT suggest that approximately 20- 40 people would need to be examined to confirm if observed difference for scapular upward rotation and internal rotation are significantly different. The symptomatic patients presented with several diagnoses comprising a heterogeneous sample. Furthermore, a single diagnosis would yield more consistent findings as was the case in Seitz previous research [26,27]. The use of the SRT and SAT is applied to patients with several different diagnoses which is why we included more than a single diagnosis. Additionally, muscle activity was not assessed to establish muscle pattern alterations during the application of the SRT and SAT, which may help explain observed kinematic alterations. In the current study, the SAT was performed during dynamic humeral elevation; however, participants self-reported level of disability was not captured. Therefore future research should be done on both tests with patients with moderate and severe disability in their shoulder to examine the effects of these tests on a more disabled patient population.
Conclusion
The SRT and SAT as performed by a single examiner and as described by Kibler appear to have the primary effect on posterior tilt and to a less degree on scapular elevation in both symptomatic and asymptomatic subjects. This pilot study provides the first examination of scapular kinematics during the performance of the SRT. It also builds on the previous static findings that the SAT increases posterior tilt and appears to demonstrate that posterior tilt is increased during the dynamic performance of the SAT. These clinical tests that alter patients reported symptoms and appear to alter scapular kinematic provide support that patients presenting with shoulder pain may need to have interventions that are targeting scapular control and mobility.
Acknowledgements
The authors would like to thank Dustin Golebieski and Stephanie Moore-Reed for their support and assistance during data collection and analysis.