Injections of Leukocyte-Reduced Platelet-Rich Plasma in Partial Tears of the Achilles Tendinopathy: A Report of Six Cases
- 1. Department of Orthopaedic Surgery, The Jikei University School of Medicine, Japan
Abstract
A conservative repair for a partial tear conformed in the tendinopathy-affected tendon is difficult, however, in 6 patients with Achilles tendinopathy the partial tears could be repaired by injections of an autologous leukocyte-reduced platelet-rich plasma (PRP). There were 4 men and 2 women with mean age of 64 years and mean disease duration of 7.3 months. High intensity areas in the Achilles tendons were observed in both short tau inversion recovery (STIR) images and T2* images of a magnetic resonance (MR) analysis. The PRP injections were performed for 1 to 3 times during 3 weeks depending on clinical recovery. All cases returned to sport activities at a previous level as without symptoms and the high intensity areas in MR images disappeared at 3 or 4 months after the PRP therapy. The outcomes indicated that PRP injections led to successful repair of partial tears conformed in the Achilles tendinopathy
Keywords
• Platelet-rich plasma (PRP)
• Tendinopathy
• Partial tear
• Achilles tendon
Citation
Yoshida M, Marumo K (2017) Injections of Leukocyte-Reduced Platelet-Rich Plasma in Partial Tears of the Achilles Tendinopathy: A Report of Six Cases. JSM Arthritis 2(1): 1021.
INTRODUCTION
Partial tears are sometimes observed in tendons affected with tendinopathy, in which complicating tendon tissue degeneration interferes with conservative repair, successful otherwise after acute fresh injuries. Micro-degenerative damages developed due to tendinopathy might produce a pathologic condition that impedes with the normal reparative reaction within the tendon tissue [1].
In the current decade, a therapy of autologous platelet-rich plasma (PRP) injections has been clinically applied in treatment of Achilles tendinopathy and significant therapeutic effects were showed compared to the conventional therapies [2-6]. We attempted to use PRP injections to conservatively repair partial tears observed as high intensity areas (HIA) in magnetic resonance (MR) images in 6 cases for the Achilles tendinopathy [7,8].
PATIENTS AND METHODS
All 6 patients were diagnosed with Achilles tendinopathy by the criteria applied to the previous study [1-6]. They had not recently had any acute injuries. There were 4 men and 2 women with a mean age of 64 years (43 – 95 years). The mean period from the diagnosis to the commencement of PRP therapy was 7.3 (4 - 12) months (Table 1).
|
Table 1: Profiles and clinical data of 6 cases. |
||||||
|
Case(Years Old) |
Gender |
Age |
PeriodaSports |
Vascularity Tear Size |
(width × depth × length) |
Number of injections |
|
1 |
M |
43 |
12marathon |
III4.5 × 2.1×17.8 |
2 |
|
|
2 |
M |
53 |
5 football |
III5.1 × 2.8 × 10.2 |
2 |
|
|
3 |
M |
63 |
7 tennis |
IV4.6× 8.8× 25.1 |
2 |
|
|
4 |
M |
63 |
4 marathon |
IV3.5× 2.3 × 9.2 |
3 |
|
|
5 |
F |
67 |
12 dance |
III3.8× 4.7 × 16.7 |
1 |
|
|
6 |
F |
95 |
5 bowling |
III8.0× 2.1 ×27.4 |
1 |
|
|
a Period from the diagnosis to the first injection of PRP |
||||||
All patients resisted against any conventional therapies including an eccentric stretching or the injection of a corticosteroid for more than 4 months before decision to receive the PRP treatment.
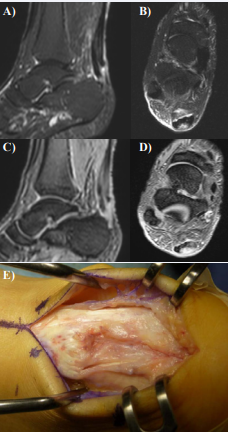
Power-Doppler analyses were performed for all Achilles tendons. In each tendon, a grade of vascularization was evaluated according to the vascularization grading system determined by Del Buono (Table 1) [9]. Magnetic resonance examinations were performed with short tau inversion recovery (STIR) or T2* images and sagittal or transverse sections were constructed for all Achilles tendons. In all cases, the HIAs were observed in both STIR images and T2* images. A HIA in a STIR image indicated a fluid accumulation or inflammation, and a HIA in T2* image indicated a tendon degeneration or fluid accumulation. The borders of HIAs were easily determined in all cases. In our previous studies we have confirmed that HIAs in both STIR images and T2* images reflect partial tears associated with degeneration by comparison of those MR findings with directly inspected tendons during surgery for tendon repairs (Figure 1).
Figure 1 MR images and a photo of the Achilles tendon in a case, in which partial tear was surgically repaired. A. A sagittal section, STIR image; B. A transverse section, STIR image; C. A sagittal section, T2* image; D. A transverse section, T2* image; E. A photo of the Achilles tendon at surgery. A partial tear associated with degenerative tissue was observed at the posterior side of the tendon
Therefore, the HIAs in 6 patients from the present study were considered partial tears associated with tendon degeneration. However, detection of partial tears by ultrasonography was rather difficult. Each tear sizes (width, depth or length) were measured in sagittal or transverse sections on STIR images. The mean volume of tears was calculated as 360.5 (74.1 - 1016.1) mm³ .
A 3.0 mL of an autologous leukocyte-reduced PRP was obtained from 20 mL of the whole blood by using the preparation kit (MyCells, Kaylight, Tel Aviv, Israel), accordingly with the manufacturer’s instructions. We obtained an autologous PRP at the mean platelets concentration of 8.8×105 / μL containing leukocytes at the mean concentration of 3.1×103 cells / μL and no erythrocytes. An obtained PRP sample was classified as type 3 according to the Mishra’s classification and as pure PRP in PAW classification since we did not activate PRP before injection.
A point of tenderness at the Achilles tendon was determined and marked. Then, the surface of the skin at the marked region was sterilized with a 10 % povidone-iodine solution and a PRP was slowly and gently injected into or around the tendon by using a 30 G needle via the peppering technique with the patient in prone position without previous anesthesia. An ankle was immobilized with the cast under non-weight bearing conditions for one week. After the cast was removed, ROM exercises were started and a weight bearing was gradually introduced. At 3 weeks after the injections, a total weight bearing was permitted and an efficacy of the PRP therapy was evaluated by clinical examinations. A grade of a pain was recorded with using the visual analog scale (VAS). When the observed effect was not satisfactory, second PRP injections was carried out in the same manner followed by bandaging or brace treatment under total weight bearing conditions. After three weeks, a clinical examination was carried out and the treatment efficacy was evaluated. If the progress in pain reduction stopped and plateaued, an another injection of PRP was administered in the same manner. The mean number of the injections was 1.8. Following the last injection, clinical follow-up was carried out for 12 - 24 months in all cases.
RESULTS
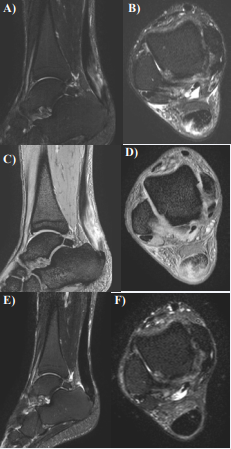
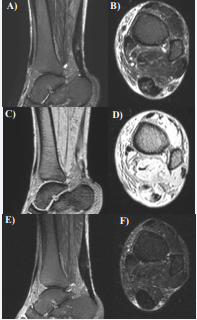
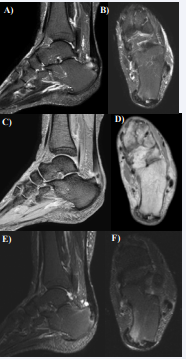
A pain was almost disappeared in all six cases and the final mean value of the VAS was 0.25 (0.0~0.5). All six patients returned to their sport activities as during previous levels with no symptoms. The vascularity grade declined to grade I or grade II. Magnetic resonance images showed that the initially observed HIAs disappeared on STIR images in all cases. The MR images of cases 3 - 5 are shown in (Figures 2- 4).
Figure 2 MR images of Case 3. A. A sagittal section, STIR image; B. A transverse section, STIR image; C. A sagittal section, T2* image; D. A transverse section, T2* image. The high intensity area observed in the Achilles tendon; E. A sagittal section, STIR image after PRP therapy; F. A transverse section, STIR image after PRP therapy. The high intensity area on STIR images disappeared after PRP therapy.
Figure 3 MR images of Case 4. A. A sagittal section, STIR image; B. A transverse section, STIR image; C. A sagittal section, T2* image; D. A transverse section, T2* image. The high intensity area observed in the Achilles tendon; E. A sagittal section, STIR image after PRP therapy; F. A transverse section, STIR image after PRP therapy. The high intensity area on STIR images disappeared after PRP therapy. A
Figure 4 MR images of Case 5. A. A sagittal section, STIR image; B. A transverse section, STIR image; C. A sagittal section, T2* image; D. A transverse section, T2* image. The high intensity area observed in the Achilles tendon; E. A sagittal section, STIR image after PRP therapy; F. A transverse section, STIR image after PRP therapy. The high intensity area on STIR images disappeared after PRP therapy
DISCUSSION
It has been challenging to conservatively repair partial tears in tendinopathy-affected tendons comparing to those following acute fresh injuries. Hence, partial tears have generally been repaired surgically: the degenerative tissue was resected and the partial tear sutured [1]. There were few reports that partial tears caused by tendinopathy might be conservatively repaired with PRP therapy, although most orthopedic surgeons have considered the PRP therapy efficient in treatment of tendinopathy [2-6]. In the present study, we report that high intensity areas observed in STIR MR images disappeared after application of the PRP therapy, indicating that PRP injections facilitated conservative repair of partial tears conformed in tendinopathy-affected Achilles tendons. However, we still do not know how large a partial tear could be to allow for successful repair with the PRP therapy. In our series, we demonstrated that the repair was possible with a tear having maximum volume of approximately 1000 mm3 . When the width of the tear was 5 mm and the depth 4 mm (approximate mean sizes of the tears in the present study), the length would be 50 mm with the volume of 1000 mm3 . Further investigations are necessary to elucidate the effects of partial tear volume or size on limitations of the PRP therapy.