Poor Level of Physical Activity in Patients with Fibromyalgia Compared to European and French General Populations
- 1. Clermont Université, Laboratoire de Pharmacologie, Faculté de médecine F-63001 Clermont-Ferrand, France
- 2. Inserm, CIC 1405, UMR Neurodol 1107, F-63003 Clermont-Ferrand, France
- 3. Centre d’Evaluation et de Traitement de la Douleur, CHU Amiens, France
- 4. Centre d’Evaluation et de Traitement de la Douleur, CHU Clermont-Ferrand, France
- 5. Centre d’Evaluation et de Traitement de la Douleur, Hôpital Jean Minjoz, CHRU Besançon, France
- 6. Service de Rhumatologie et Algologie, Hôpital Sainte Musse, CHI Toulon, France 7
- 7. CHU Clermont-Ferrand, Centre de Pharmacologie Clinique, F-63003 ClermontFerrand, France
- 8. Service de Neurologie, CH Lyon-Sud, France
- 9. Centre d’Evaluation et de Traitement de la Douleur, CH Bayeux, France
- 10. Centre d’Evaluation et de Traitement de la Douleur, CH Bayonne, France
- 11. CHU Clermont-Ferrand, Délégation Recherche Clinique & Innovation - Villa annexe
Abstract
Background: Patients suffering from fibromyalgia reported to have a lower level of physical activity than the general population. The aim of this study was to assess physical activity in patients with fibromyalgia referred to French Pain Clinics and to compare it with data obtained from a large European survey, the “Eurobarometer 64.3” (EB 64.3).
Methods: This observational study was conducted in seven French Pain Clinics and included 76 patients with fibromyalgia. Daily physical activity was assessed by patients at their first Pain Clinic visit using the International Physical Activity Questionnaire (IPAQ). According to IPAQ items, the number of days per week spent “walking”, in “moderate physical activity”, “vigorous physical activity” and “sitting” was recorded and compared (significance<0.05) with French and European data obtained from the EB 64.3 according to age and gender categories using Student t-test or Welch’s test (significance<0.05).
Results: Compared to general French (Fr) and European (Eu) populations, 76 patients with fibromyalgia (FM) reported significantly lesser physical activity (days/week) in moderate physical activity (FM: 1.8 ± 1.1; Fr: 2.0; P=0.12; Eu: 2.5; P<0.001), vigorous physical activity (FM: 0.6 ± 0.9; Fr: 1.6; Eu: 1.7; P<0.001) and walking (FM: 1.8 ± 1.4; Fr: 4.5; Eu: 4.6; P<0.001). Time spent in moderate physical activity during leisure time (28.5 mins/week) was well below international recommendations (150 mins/week).
Conclusions: This study demonstrates for the first time that patients with fibromyalgia are significantly much less active than general French and European populations and their daily physical activity are below international recommendations. In fibromyalgia, factors of this deconditioning such as pain, kinesiophobia or mitochondrial dysfunction need to be further investigated in order to improve fibromyalgia therapeutic strategies. Adaptation and individualization of physical rehabilitation programs for fibromyalgia patients are recommended to improve the clinical symptoms, but the long-term benefits of tailored exercise in fibromyalgia remain to be assessed.
Keywords
• Eurobarometer 64.3
• International physical activity questionnaire
• Fibromyalgia
• Physical activity
Citation
Martin E, Serra E, Delage N, Tiberghien F, Mechtouf K, et al. (2016) Poor Level of Physical Activity in Patients with Fibromyalgia Compared to European and French General Populations. JSM Arthritis 1(3): 1017.
ABBREVIATIONS
ACR: American College of Rheumatology; APS: American Pain Society; AWMF: Association of the Scientific Medical Societies in Germany; EB: Eurobarometer; Eu: European; EULAR: European League against Rheumatism; FM: Fibromyalgia; Fr: French; IPAQ: International Physical Activity Questionnaire; PA: Physical activity; WHO: World Health Organization
INTRODUCTION
According to a survey conducted in five European countries [1], 2.9% of adults in Europe and 1.6% in the French general population are diagnosed with fibromyalgia (FM) [2], predominantly women. FM is a chronic rheumatic disorder characterized by pain described by patients as muscular and/ or skeletal, diffuse and chronic, exacerbated by pressure on tendon insertion points, associated with sleep disturbances and long-term fatigue [2]. FM is defined by clinical criteria that were established by the American College of Rheumatology (ACR) in 1990 as widespread pain (defined as axial pain, left- and right-sided pain, and upper and lower segment pain) for more than three months in combination with tenderness at 11 or more of 18 defined point sites. A redefinition was proposed in 2010 as FM is accompanied by a combination of additional symptoms such as cognitive impairment, unrefreshed sleep, fatigue and somatic symptoms that have also to be taken into account. The 2010 ACR criteria were aimed at simplifying the diagnosis of FM without requiring a tender point examination [3].
FM impacts on every aspect of daily life, and all dimensions of health-related quality of life are affected. Physical as well as psychological functioning with symptoms of depression and anxiety are reported [4]. In addition, fear of pain and of exercise contribute to impair physical functioning [5]. However, strong evidence supports the importance of an active life-style to better manage FM symptoms, and aerobic exercise has been shown to be beneficial to patients with FM [6]. The European League Against Rheumatism (EULAR), the American Pain Society (APS), and the Association of the Scientific Medical Societies in Germany (AWMF) have published guidelines for the treatment of patients with FM. APS and AWMF recommendations for “first line” therapy include aerobic exercise, cognitive-behavioral therapy, amitriptyline (a tricyclic antidepressant) and multicomponent therapy (combination of exercise therapy with at least one psychological therapy). These recommendations contrast with EULAR guidelines which place a greater emphasis on medications, recommending pharmacological treatments such as amitriptyline, tramadol, fluoxetine, duloxetine, milnacipran, moclobemide, pirlindole, tropisetron, pramipexole and pregabalin. A systematic review of these guidelines has concluded to a global high strength of recommendation for aerobic exercise [7].
The World Health Organization (WHO) defines physical activity (PA) as any bodily movement produced by skeletal muscles, including activities undertaken while working, playing, carrying out household chores, travelling, and engaging in recreational pursuits. From a public health perspective, WHO guidelines on PA have been developed for the general population in order to promote health-related PA [8]. Surveys such as the “Eurobarometer” have been conducted in Europe on behalf of the European Commission. They provide regular monitoring of social and political attitudes in the European public. These European surveys have assessed PA in the Member States using the “International Physical Activity Questionnaire” (IPAQ), a questionnaire that has been validated in 2003 allowing a cross-cultural comparison of PA parameters.
Although patients with FM are considered to be less physically active than patients without FM, only three controlled trials studied this issue, using IPAQ in women with FM compared to healthy women [9-11]. In order to assess the intuitively described low level of PA in patients with FM, our study aims to compare PA data obtained in French patients with the general French and European population data extracted from the Eurobarometer 64.3 (EB 64.3).
MATERIALS AND METHODS
Study design and subjects
This observational study was conducted in seven French Pain Clinics spread over the whole of France and included 100 patients with FM. They filled out the IPAQ (long form) in the course of their first visit to the Pain Clinic. The IPAQ questionnaire is part of a battery of tests systematically done at the first Pain Clinic visit for all fibromyalgia patients presenting at a Pain Clinic. Patients were invited to participate to the study after clinical examination by the rheumatologist or pain specialist if they were ≥ 18 years and diagnosed with FM according to the ACR criteria [3]. Between November 2013 and August 2014, 76 questionnaires were returned to the Clinical Investigation Center and analyzed. Data were anonymized in order to protect the privacy of the subjects and the confidentiality of their personal information.
Assessment
Concerning the general European population, data were drawn from the EB 64.3. The Eurobarometer survey series, running since 1970, is the product of a unique program of cross-national and cross-temporal social science research, designed to compare and gauge trends within Europe. Surveys on health status and health behavior of the general European population aged 15 years and over have also been conducted (i.e. the Special Eurobarometer Wave 64.3 in Autumn 2005 [12]). The EB 64.3 conducted in 32 European countries between November and December 2005 was commissioned by the Directorate General Health and Consumer Protection and carried out by TNS Opinion & Social, a consortium formed by TNS and EOS Gallup Europe. The methodology was that of the standard Eurobarometer surveys of the Directorate General Press and Communication (“Opinion Polls, Press Reviews, Europe Direct” unit). The aim of this survey was to study several areas having an impact on the health of European citizens (for further information see http:// www.icpsr.umich.edu/icpsrweb/ ICPSR/studies/4590). The total sample included 29,193 respondents with 24,682 in the 25 European Union member countries and 1,012 in France [12]. Data from the Special Eurobarometer survey series are publicly accessed and reproduction is authorized, except for commercial purposes.
The IPAQ has been developed to assess health-related PA and consists in two questionnaires: a short form (9items) and a long form (31 items) [13]. Validity and reliability correlations of the long form used in this study are respectively 0.30 and 0.80 supporting the acceptability of the psychometric performance of IPAQ. The self-administered IPAQ is used to obtain internationally comparable data on health-related PA and is designed to assess the frequency, duration, and intensity of PA across all domains of work, transportation, housework/gardening tasks, leisure-time activity and time spent sitting for seven days. The IPAQ questionnaire is available in Additional Figure (1)
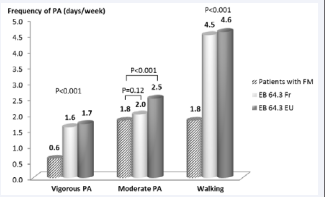
Figure 1 Mean frequency of physical activity of patients with fibromyalgia compared to general populations data (EB64.3). The Patients with FM reported significantly less PA than general Eu and Fr populations (P<0.001). EB 64.3 Fr, general French population data drawn from the Eurobarometer 64.3; EB 64.3 EU, general European population data drawn from the Eurobarometer 64.3; FM, fibromyalgia; PA, physical activity
and IPAQ scoring protocol was based on instructions available at www. ipaq.ki.se.
Outcome measures were: (1) number of days reported in vigorous intensity activity, moderate intensity and walk per week (at work, during transportation, housework/gardening tasks and leisure-time activity); (2) time (mins) reported in vigorous- and moderate-intensity activity and walk per day (at work, during transportation, housework/gardening tasks and leisure-time activity) and (3) mins spent sitting per day.
In order to examine whether frequency and duration of PA varied across sociodemographic factors, PA data (vigorous, moderate and walking) and sitting time were compared across gender and age in four categories (15-24, 25-39, 40-54 and 55 years and older). Days per week spent in each intensity level of PA (vigorous PA, moderate PA and walking) were calculated by averaging days per week spent in PA at work, during housework/ gardening tasks (for vigorous PA and moderate PA) or during transportation (for walking) and during leisure-time activity (for vigorous PA, moderate PA and walking). This calculation is similar for the average mins per day spent in each intensity level of PA. Daily sitting time was calculated by averaging responses of the last items of the IPAQ (“time spent sitting on a weekday” and “time spent sitting on a weekend day”). Finally, patients with FM data were compared to French and European population data extracted from the EB 64.3 and according to gender (women and men) and age categories (15-24, 25-39, 40-54 and 55 years and older) established by the EB 64.3.
Statistical analysis
Statistical analysis was performed using Stata 13 software (StataCorp LP, College Station, TX, US). The tests were two-sided, with a Type I error set at α = 0.05. Quantitative data were presented as mean ( ± standard-deviation) and categorical parameters as the number of patients and associated percentages. Comparisons between independent groups (general French and European populations) were performed using 1) test of proportions for categorical variables (chi-squared test or Fisher’s exact test when appropriate) and 2) Student t-test or Welch’s test for quantitative parameters (homoscedasticity studied using Fisher-Snedecor test). As proposed by some statisticians, we chose to report all the individual p-values without doing any mathematical correction for distinct tests comparing general French and European populations [14].
RESULTS
In the 7 pain clinics, 100 patients with FM were pre-screened and 76 patients responded to the questionnaire (response rate 76.0%); 67 women and nine men with a mean age of 47.5 ± 10.3 years and a female to male ratio of 7:1. Unemployment amounted to 63.2% of patients with FM and 36.8% had a part-time or full-time job. The mean time interval between the time of FM diagnosis and the time of administration of the IPAQ questionnaire was 3.8 ± 4.4 (range: 0.1 – 21.6) years. Characteristics of the 76 participants are summarized in Table 1.
| Table 1: Demographic characteristics in patients with fibromyalgia. | ||
|
|
|
Patients with FM (n = 76) |
|
Gender, n (%) |
|
|
|
|
Female |
67 (88.2) |
|
|
Male |
9 (11.8) |
|
Age (year), mean ± SD |
47.5 ± 10.3 |
|
|
|
Female |
47.8 ± 10.6 |
|
|
Male |
45.8 ± 8.2 |
|
Age (year), n (%) |
|
|
|
|
15-24 |
2 (2.6) |
|
|
25-39 |
12 (15.8) |
|
|
40-54 |
44 (57.9) |
|
|
55 + |
18 (23.7) |
|
Age (year), range |
20 - 73 |
|
|
Employment status, n (%) |
|
|
|
|
Employed |
28 (36.8) |
|
|
Unemployed |
48 (63.2) |
|
Time interval between time of FM diagnosis and time of questionnaire administration (year), mean ± SD [range] |
3.8 ± 4.4 [0.1 – 21.6] |
|
|
Abbreviations: FM: Fibromyalgia; SD: Standard deviation. |
||
| Abbreviations: FM: Fibromyalgia; SD: Standard deviation | ||
Patients with FM reported 0.6 ± 0.9 days/week and 26.5 ± 50.4 mins/day (22.9 ± 79.6 mins/week) spent in vigorous PA, 1.8 ± 1.1 days spent and 35.9 ± 32.5 mins/day (28.5 ± 94.7 mins/ week) in moderate PA and spent 1.8 ± 1.4 days and 30.4 ± 39.5 mins/day walking (Figures 1 and 2). Women and men reported no significant difference in frequency (days/week) and duration (mins/day) of vigorous PA and walking, in duration of moderate PA and in time spent sitting. Women reported significantly higher frequency of moderate PA than men (women: 1.9 ± 1.1 days/ week; men: 0.6 ± 0.6 day/week; P<0.001) (Additional Table 1).
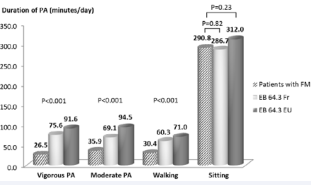
Compared to general European (Eu) and French (Fr) populations, patients with FM reported significantly less days/ week in: vigorous PA (FM: 0.6; Eu: 1.7; Fr: 1.6; P< 0.001), moderate PA (FM: 1.8; Eu: 2.5; P< 0,001) and walking (FM: 1.8; Eu: 4.6; Fr: 4.5; P< 0.001) (Figure 1 and Additional Table 1). Patients with FM reported significantly lower duration of PA measured in mins/ day compared to general Eu and Fr populations in: vigorous PA (FM: 26.5; Eu: 91.6; Fr: 75.6; P< 0.001), moderate PA (FM: 35.9; Eu: 94.5; Fr: 69.1; P< 0.001) and walking (FM: 30.4; Eu: 71.0; Fr: 60.3; P< 0.001). No significantly group difference was found for time spent sitting (mins/day) (P=0.82) between groups (Figure 2 and Additional Table 1).
Figure 2 Mean duration of physical activity of patients with fibromyalgia compared to general populations data (EB64.3). The Patients with FM reported significantly lower duration of PA compared to general Eu and Fr populations (p<0.001). No group difference was found for time spent sitting. EB 64.3 Fr, general French population data drawn from the Eurobarometer 64.3; EB 64.3 EU, general European population data drawn from the Eurobarometer 64.3; FM, fibromyalgia; PA, physical activity
Considering leisure time, patients with FM reported to spend 28.5 ± 94.7 mins/week in moderate PA (such as cycling, swimming at a regular space and tennis) and 22.9 ± 79.6 mins/ week in vigorous PA (such as aerobics, running, fast bicycling or fast swimming). Specific data concerning moderate and vigorous PA during leisure time were not available for Eu and Fr populations.
DISCUSSION
This study demonstrates that patients with FM have a very low level of PA compared to a large general population. The frequency and duration of vigorous PA, moderate PA and walking reported by French patients with FM are significantly lower than in the general European and French populations (P<0.001). Our findings, with a female to male ratio of 7:1 similar to published data [15], confirm intuitive and pragmatic results reported by clinicians concerning the low level of PA in FM. Patients with FM are also below WHO recommendations when considering current global recommendations on PA for health (World Health Organization, 2010), leisure time PA and sport. Moderate and vigorous PA during leisure time in patients with FM are respectively 28.5 ± 94.7 mins/week and 22.9 ± 79.6 mins/week whereas according to WHO recommendations, adults aged 18-64 years should have at least 150 mins of moderate-intensity aerobic PA throughout the week (or at least 75 mins of vigorous-intensity aerobic PA throughout the week, or an equivalent combination of moderate- and vigorous-intensity activity [8]). Our study shows that only 9.0% of women and 11.1% of men do meet the WHO recommendations for moderate to vigorous PA (moderate PA: ≥ 150 mins/week or vigorous PA: ≥ 75 mins/week). Reversely, Natvig et al. [16], observed that women with FM reported higher PA during their leisure time than a control female population. This unexpected result was explained by the observation that patients with FM with reduced employment activity have more leisure time to spend on PA
Poor level of PA in patients with FM has also been observed in previous studies assessing physical performance abilities and functional limitation in performing daily activities by self-report instruments (IPAQ and the COOP-WONCA Chart “Physical fitness”) [9,10,16] and objective measurements (accelerometer, 6-minute walk test and muscle function tests) [9,10,17].
This dramatic low level of PA has been suggested as a cause and also as a consequence of FM. Pain, central mechanisms, kinesiophobia (fear of movement), biochemical and endocrine dysfunction all interact in this syndrome whose primary manifestation is muscle and skeletal pain (5,18–21). Moreover, four meta-analyses have suggested that exercise training interventions of multiple kinds such as aerobic / mixed, aquatic and resistance exercises have significant and positive effects for pain reduction (6,22–24).
Patients with FM often develop fear of movement. This concept, also known as kinesiophobia, (Vlaeyen et al. [19]), may contribute to functional limitation and amplified pain perception. A behavioral pattern of brief alternating periods of vigorous PA or a sudden increase in PA followed by prolonged periods of inactivity trigger worsening symptoms and are often observed in patients with FM [20]. Approximately 40% of patients with FM may display high levels of fear of movement and avoidance behavior towards PA [5,21]. However, Russek et al. [22], have recently showed a lack of correlation between kinesiophobia and moderate or vigorous PA and suggested to conduct further studies in order to investigate whether kinesiophobia mediates the relationship between pain and physical function in patients with FM.
For several years numerous clinical trials assessing the effect of specific exercise (e.g. aerobic, strengthening, stretching) in patients with FM have found a beneficial effect on pain and depression, on physical function and global health (6). In FM, successive guidelines published since 2005 assigned the highest level of recommendation to aerobic exercise [23]. Newer studies also indicate that physical activity may enhance cognitive performance and decrease psychological symptoms (e.g. anxiety and depression) reinforcing the importance of exercise program in patients with FM [24, 25].
However, a poor compliance and a high dropout rate are frequent in exercise programs and there is today little information on the long-term benefit of exercise in FM [26]. Drop-out rates often exceed 30% [27, 28] suggesting the importance to develop exercise interventions that can be sustained. Information and education of patients on the benefits of PA in FM, adaptation and individualisation of exercise programs centered on symptom severity, tolerance to exercise-induced pain and reduction of fear of movement are the goals of clinicians to overcome the deleterious effects of physical deconditioning [29]. In order to find ways to promote PA in persons with FM that can be sustained over time, a study has shown that promoting increased PA by asking patients with FM to accumulate short bouts of activity throughout the day can markedly increase PA and reduce perceived functional deficits and pain [30]. Exercise enjoyment appears to be important for the long-term effectiveness of exercise programs and need to be maximized in future interventions to promote PA in persons with FM [31]. Regular PA measurement in everyday life with a combination of subjective (self-report questionnaires) and objective (i.e. accelerometry) measures may help to better understand the deconditioning pattern observed in FM.
CONCLUSION
This study compares for the first time French FM patients to large population samples from France and Europe and shows that patients with FM have a much lower level of PA than the general French and European populations. In this complex pathology, causes of such a deconditioning are intertwined and need to be explored further in order to give therapeutic options to patients with FM. Individualized exercise programs are highly recommended to improve well-being, quality of life and physical function, but the long-term benefits of tailored exercise in FM remain to be evaluated.
ACKNOWLEDGEMENTS
We thank clinical staff of the Pain Clinics involved in the study for the collaboration in data collection. We are very grateful to all patients who kindly completed the questionnaires.
Authors’ contributions
EM had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: GP and EM. Acquisition, analysis, or interpretation of data: All authors. Drafting of the manuscript: GP and EM. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: BP. Administrative, technical, or material support: EM. Study supervision: GP and EM.