Major Amputations due to Chronic Lower Limb Vasculopathy: A 15-Year Brazilian Analysis
- 1. Bahiana School of Medicine and Public Health, Applied Regional Anatomy Academic Monitoring, Brazil
- 2. Doctor Adjunct Professor of Escola Bahiana de Medicina e Saúde Pública, Brazil
Summary
Introduction: Major lower limb amputations are common procedures performed in elective and emergency settings, with diabetes mellitus and peripheral vascular disease as the main causes. There is a strong financial impact on the health system and a notorious psychosocial impact on patients.
Objective: To describe the statistical behavior of hospitalizations due to major lower limb amputations, as well as their distribution in Brazilian regions. Materials and Methods: A descriptive, observational, retrospective study based on secondary data extracted from the SUS Hospital Admissions System (SIH/SUS) between 2008 and 2023.
Results: 371,232 hospitalizations were recorded, with an increase in the number of hospitalizations of 67.03%. The Southeast and Northeast regions accounted for the largest absolute numbers, with 42.12% and 32.52% of hospitalizations, respectively. The Northeast had the highest average hospitalization rate (12.9). There were 47,264 deaths and an average mortality rate of 12.73 in Brazil.
Conclusion: There was a greater concentration of the number of procedures, especially in the Southeast and Northeast, reflecting regional population disparities. In addition, the relative growth rate in the number of amputations is especially noticeable in the North and Center-West, possibly related to the growth and aging of the population.
Keywords
• Amputations
• Diabetes
• Peripheral arterial disease
Citation
Mota PHC, Kuhn PLLP, Silveira JGR, de Farias IP, Lima GN, et al. (2024) Major Amputations due to Chronic Lower Limb Vasculopathy: A 15-Year Brazilian Analysis. JSM Atheroscler 5(1): 1044.
INTRODUCTION
Major lower limb amputations (LLA) are defined as those occurring above the level of the ankle, while minor amputations are defined as those occurring at the level of the foot and pododactyls [1,2]. A major procedure can also be divided into transtibial, transfemoral and thigh or knee disarticulations, these variations have different techniques and the need to preserve as much of the limb that will undergo the intervention as possible must be taken into account [2].
Many criteria and clinical signs are used to determine the level of amputation, and the professional must make the decision that represents the best prognosis for the patient [3] and take into account the perfusion status of the target limb as a determining factor as to whether or not a major amputation should be performed. AM corresponds to a surgical method of exception and last resort, whose impact on the patient’s prognosis and quality of life is growing, limiting and notorious [4].
MAs are widely recorded in the literature and include reports of procedures carried out more than 7,000 years ago [5]. However, until the 17th and 18th centuries, the prevalence of this surgery was exclusively linked to the treatment of trauma and, only since the 20th century, amputations have been performed on limbs that have suffered ischemia from other causes, such as in diabetic patients [7]. In this context, there has been an increase in the frequency of amputations due to vascular causes, especially in Brazil. According to studies, AM due to peripheral arterial disease (PAD) reaches 56.3%, while 43.7% are due to diabetes mellitus (DM). These data show an increase of 1.2% to 22.9% in AM caused by diabetes mellitus and 4% to 19.4% in cases of PAD as the cause [3].
In Brazil, there is a 65% increase in the frequency of AM between 2012 and 2022. According to the Brazilian Society of Angiology and Vascular Surgery, the Southeast is the region with the highest absolute number of AM, accounting for 118,962 amputations, 42% of the total. This was followed by the Northeast with 92,265, the South with 39,952, the North with 15,848 and the Midwest with 15,546. However, there is little literature showing their distribution by state, as well as the causes of these figures.
Traumatic and vascular causes are of significant importance to the surgical outcome of amputation. With regard to the latter, we can identify PAD, DM, hypertension, smoking, dyslipidemia renal failure and hypercoagulability as other causes integrated with vascular disorders. In addition, ischemia, immune weakness and neuropathy are factors conducive to the onset of infectious processes and loss of tissue function [7,8].
DM is an important cause of AM and vascular disorders, which can lead to the need for a certain surgical procedure. A survey has shown that more than 80% of diabetics have some form of vascular disease [9]. Another study showed that 51% of amputated patients had DM as a cause, while 31% had vascular injuries and another 17% had arterial thrombosis and atherosclerosis [10]. Another source found that around 50 to 70% of AM cases occur in diabetic patients with PAD [11,12].
Elderly patients are more likely to undergo major amputations when compared to other age groups, so that the highest average number of amputations is between 60 and 79 years of age [13]. The mortality rate associated with AM is also a predictor of epidemiological importance, so the risk of death is considerably present in patients undergoing AM. In fact, the 5-year mortality rate after any amputation was high, ranging from 53% to 100%, while in proximal amputations it ranged from 52% to 80%. PAD, kidney disease and other repercussions of diabetes increased the risk of death after AM [14,15]. Complications and post-operative repercussions have a significant impact on the patient, with problems related to the stump, quality of life, mobility and social integration being the most frequently mentioned and reported.
Still with regard to perioperative repercussions, the mortality rate of all AMs occurring during the perioperative period is considered high, reaching 22% in the first 30 days, 44% after one year and 77% at 5 years [7,16]. Another survey concludes that the death rate is around 10%, taking into account that in the first year, 30% of patients die; in the third year, the percentage is 50% and in the fifth year, it reaches 70% [17].
When comparing this same variable between groups that underwent minor amputations and those that underwent major amputations, the figure is 21% in the former compared to 38% in the latter, considering the 1-year interval [18]. On the other hand, the mortality rate at 5 years is extremely high, reaching a range of 56 to 70% [16,19-21]. There is a consensus that major amputations always have the highest perioperative mortality rate, regardless of the patient’s profile [18].
For all the above reasons, the magnitude of the various factors related to AM is still under discussion. There are gaps between the studies that report the epidemiology of amputations, the prevalence of PAD and DM and the other causes of critical ischemia in Brazil, as well as their surgical and post-operative complications [3,11,12]. This study aims to help understand the Brazilian reality in terms of the data available in its public health system, taking a regional view of the country.
MATERIALS AND METHODS
This is a descriptive, observational and retrospective study, based on secondary data extracted from the SUS Hospital Admissions System (SIH/SUS). It analyzed hospital admissions for non-traumatic AM between 2008 and 2023, by region and by place of hospitalization. The research segment involved processing the data in tables and graphs using Microsoft Excel software. All the data can be found on Data SUS, Tab Net via the link: https://datasus.saude.gov.br//.
AM-related hospitalizations are described taking into account the following variables: number of hospitalizations; coefficient of hospitalizations; hospitalization rate; number of deaths; mortality rates; total amount spent in dollars; average amount spent per hospitalization in dollars; total days of stay; average days of stay. The data was structured by Brazilian regions (North, Northeast, South, Southeast and Center-West) and by year of service from 2008 to 2023.
The hospitalization coefficient was calculated from the ratio between the number of hospitalizations due to AM and the resident population in the respective year and region. The hospitalization rate was calculated by dividing the number of admissions for AM by the total number of admissions in the respective year and region. The data on the resident population was taken from the demographic and socio-economic indicators in the “Study of Population Estimates by Municipality, Sex and Age-2000-2021”, available in the Data SUS database. All values were converted to dollars, based on the currency exchange rate on 01/23/2024 (R$: 4.95).
We excluded patients who had undergone traumatic amputations of any level or exclusively minor amputations. As it is a public health database, analysis by the Ethics Committee was not required.
RESTRICTED
Between 2008 and 2023, 371,232 hospitalizations for AM were recorded. The largest number of hospitalizations for this procedure, in absolute numbers, was concentrated in the Southeast region, with 156,375 admissions, representing 42.12%, followed by the Northeast region (32.52%), the South (14.44%), the North (5.48%) and the Midwest (5.42%) (Table 1).
Table 1: Regional distribution of the statistical behavior of hospitalizations for lower limb amputation/disarticulation between 2008 and 2023, in Brazil
|
Variables |
North |
North East |
South East |
South |
Midwest |
Total |
|
Hospitalizations |
20346 |
120742 |
156375 |
53630 |
20139 |
371232 |
|
Hospitalization Coefficient |
6,91 |
12,95 |
10,92 |
11,28 |
7,84 |
13,87 |
|
Average Stay |
9,6 |
7,9 |
9,9 |
7,9 |
9,8 |
8,9 |
|
Deaths |
2210 |
14497 |
21500 |
6398 |
2659 |
47264 |
|
Mortality Rate |
10,86 |
12,01 |
13,749 |
11,9298 |
13,2 |
12,731 |
|
Total Amount Spent |
$ 8.770.141,78 |
$ 44.264.209,86 |
$ 71.434.216,81 |
$ 22.716.039,72 |
$ 9.054.237,23 |
$ 156.238.845,40 |
|
Average Value per Hospitalization |
$ 430,67 |
$ 366,34 |
$ 456,64 |
$ 423,13 |
$ 449,29 |
$ 420,61 |
|
Profissional Services Value |
$ 1.557.811,91 |
$ 8.307.724,87 |
$ 12.663.983,86 |
$ 3.993.823,01 |
$ 1.615.317,62 |
$ 28.138.661,27 |
|
Hospital Services Value |
$ 7.145.932,57 |
$ 35.710.337,32 |
$ 58.426.200,03 |
$ 18.620.818,29 |
$ 7.439.823,99 |
$ 127.343.112,20 |
Source: SUS Hospital Information System (SIH/SUS), available in the DataSUS data base. The following variables were expressed in absolute values: Hospitalizations; Deaths; Total Amount Spent; Value Professional Services; Value Hospital Services. The other variables were expressed through the average of the values, among the years analyzed: Hospitalization Coefficient; Average Stay; Mortality rate; Average Value per Hospitalization. The Total Amount Spent; Average Value per Hospitalization; Professional Services Value and Hospital Services Value were expressed in dollars. The Hospitalization Coefficient only covers the years 2008 to 2021 and was expressed per 100,000 inhabitants
During the period analyzed, there was a clear upward trend in the annual number of hospitalizations for AM in all Brazilian regions. It rose by 67.03%, from 16,818 in 2008 to 28,092 in 2023. The North had the highest growth rate at 113%, followed by the Midwest (88.05%), the Southeast (75%), the Northeast (63.1%) and the South (35.49%) (Graph 1).
Graph 1: Hospitalizations due to lower limb amputation/ disarticulation per year, in Brazil
With regard to the hospitalization coefficient, Brazil saw an increase in this variable between 2008 and 2021, moving from a value of 8.8 (in 2008) to 13.9 (in 2021- the last year analyzed). On average, the Northeast region stood out with the highest coefficient of hospitalizations in the period, with a value of 12.9, followed by the South (11.3), Southeast (10.9), Midwest (7.8) and North (6.9) (Graph 2).
Graph 2: Hospitalizations for Lower limb Amputation/Disarticulation per 100,000 Inhabitants per Year, in Brazil
There were 47,264 deaths due to MB, with the Southeast leading the absolute numbers with 21,500 (45.49%), followed by the Northeast with 30.67%, the South with 13.53%, the Midwest with 5.62% and the North with 4.67% of total deaths. The year 2021 had the highest number of deaths in the historical series analyzed, with 3,588 deaths (Table 1).
The average mortality rate secondary to MA was 12.73 throughout Brazil. There was a clear decrease in the dispersion of annual mortality rates, so that in 2008 the calculated standard deviation was 2.33 and in 2023 it was 0.5. In 2008, the highest and lowest mortality rates were 14.87 (Southeast region) and 8.9 (North region), while in 2023, the mortality rates for all regions were concentrated between 11.42 (South region) and 9.98 (North region). (Graph 3).
Graph 3: Mortality Rate from Lower Limb Amputations/ Disarticulations per Year
When quantifying how many days on average each patient has been hospitalized for amputations, the historical average is 8.9 days in Brazil. There is a considerable downward trend in the average number of days spent in hospital in the historical series, so that in the first survey, in 2008, the figure was 9.52 days, while in the last survey, in 2023, the average was 8.57 days. The years 2020 and 2021 showed a significant reduction in the average length of stay per patient, with 7.92 and 7.88 days respectively. With regard to the regional breakdown, there were no major differences in average length of stay between the regions. The Southeast region has the highest average number of days spent in hospital (9.9), followed by the Midwest (9.8), the North (9.6), the South (7.9) and the Northeast (7.9) (Table 1; Graph 4).
Graph 4: Average Days of Stay per Limb Amputations/Disarticulation Procedure per Year, in Brazil
There has been an increase in hospital spending on MAs across the country, from 4 million dollars in 2008 to approximately 12 million dollars in 2023, with a slight reduction to 11 million in 2023. These figures delimited a growing curve with an increase of around 200% from the initial figure (2008) to the final figures (considering the year 2022).
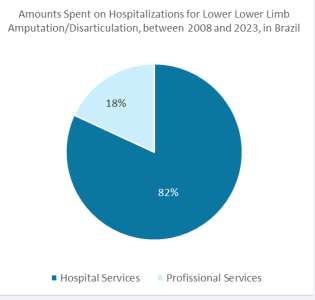
On the other hand, professional services have seen a less significant increase, from around 1 million dollars in 2008 to approximately 2.2 million dollars in 2023, marking an upward curve that has not kept pace with the increase in spending on hospital services. As a result, it was found that 82% of total spending on MS is on hospital services, while less than 20% is on professional services. In addition, the Southeast region is responsible for almost 50% of the country’s total spending. The amount spent on MS increased between 2008 and 2023, in some regions more significantly and in others less so, but it continued to increase exponentially (Table 1; Graph 5 and Graph 6).
Graph 5: Amounts Spent on Hospitalizations for Lower Limb Amputation/Disarticulation, between 2008 and 2023, in Brazil
Graph 6: Amounts Spent on Hospitalizations for Lower Limb Amputation/Disarticulation, in Dollars, per Year, in Brazil
A total of 371,232 AM procedures were recorded, followed by 367,602 finger amputation procedures and 96,753 foot and tarsal disarticulation procedures. There was also a very similar growth trend between the number of AM procedures and finger amputation/disarticulation procedures. As for foot and tarsal amputation and disarticulation, there was a less significant growth trend.
DISCUSSION
In Brazil, the Southeast leads the country in the number of hospitalizations due to AM, reflecting Brazil’s unequal population distribution, in which the largest population groups are concentrated in the Southeast, for historical, cultural and geographical reasons. It is the most industrialized region in the country, with differentiated medical care compared to other regions of the country.
In this universe, amputations at the thigh level stood out, as shown in the literature, not only because of the severity of the underlying disease, PAD or DM, but also because of the length of hospital access and stay [7]. Of the 102,056 AM performed between 2011 and 2016, 94% were performed by the Unified Health System (SUS), which corroborates the universality/ coverage of the Brazilian public health system [22].
The North was the region with the highest rate of growth in procedures, followed by the Midwest. This increase is related to the growth of the Brazilian population, around 5.34% over the same period-192.7 million Brazilians in 2008 and 203 million in 2022, the date of the last census - along with the increase in the elderly population, who are known to be more affected by AM risk factors. The literature also documents an increase of around 200% in amputations between 2012 and 2023, which corroborates our data [13].
This same upward trend can be seen in the hospitalization coefficient, which moved from a value of 8.8 (in 2008) to 13.9 (in 2021 - the last year analyzed). On average, the hospitalization coefficient over this entire time series has been close to 10 (9.96), with the Northeast region standing out (12.9), followed by the South (11.3). The data on the hospitalization coefficient is similar and in line with the figures in the literature on the worldwide incidence of amputations, which ranged from 2.8 to 43.9 per 100,000 inhabitants each year, so that in Brazil the prevalence of all amputation procedures was around 13.9, close to the average prevalence of AM of 9.96 between 2008 and 2023 [14,23].
In addition, during this same period, the average mortality rate was 12.73 in Brazil, so it is possible to see a reduction in the dispersion of mortality rates between regions, given the reduction in the standard deviation observed in the comparison between 2008 and 2023. This phenomenon can be understood as a reflection of greater, but insufficient, homogenization of regional disparities in health variables between regions, as a result of the universalization of the SUS state apparatus, in order to mitigate regional inequalities. As a result, there is less difference between the data for each region, including mortality data.
The data analyzed from 2008 to 2023 showed a total average length of stay of 8.9 days for all five Brazilian regions. The main factors influencing length of stay are: comorbidities, patients with chronic diseases such as diabetes mellitus, peripheral vascular disease or heart failure, which result in a longer length of stay. Post-operative complications such as infections, tissue necrosis and healing problems can also significantly increase the length of stay. In addition, the need for intensive rehabilitation and specialized nursing care after surgery can also influence length of stay [24,25]. In the time series analyzed, the average length of stay remained stable in all years, with the exception of 2020 and 2021, when a moderate drop in length of stay was observed, which graphically represented a depression in the curves of this section. This is justified by the pandemic period experienced (COVID-19), which peaked during 2020 and 2021, and which resulted in an overload of hospital services, possibly reducing the time of in- hospital care in the post-operative period of AM [26].
Hospitalization costs have shown an upward trend over the years, reflecting not only the increased demand for these procedures, but also the costs associated with the complexity of treatment and post-operative complications. The average costs per AM hospitalization can vary considerably, depending on various factors, such as the healthcare institution, the region of the country, the severity of the case and the presence of comorbidities. Furthermore, it is important to reflect on the economic and social impact, which, in addition to the direct costs of hospitalizations, includes the costs of rehabilitation, prostheses, long-term nursing care and loss of patient productivity. These costs, although not taken into account by Data Sus, should be considered when assessing the financial impact of these procedures.
CONCLUSION
There is a greater concentration of procedures, especially in the Southeast and Northeast, which also have more deaths, reflecting regional population disparities and requiring public policies adapted to the needs of each region. Costs tend to rise, reflecting not only growing demand, but also additional costs resulting from the complexity of treatment and post-operative complications. This highlights the need for preventive and multidisciplinary approaches to reduce not only amputation rates, but also the economic and social impact. A comprehensive, multidisciplinary approach and care can help to reduce amputation rates and improve clinical and surgical outcomes, with a knock-on effect on the financial impact on the healthcare system.
During the study, limitations were observed when using the Data SUS tool, in particular the underreporting of cases, the impossibility of investigating the epidemiological profile of patients in greater depth, in order to distinguish gender, social status, race/color and age group, as well as the lack of specification of the underlying causes of each procedure and the inflationary impact on costs.
REFERENCES
- Kolossváry E, Ferenci T, Kováts T, Kovács L, Járai Z, Menyhei G, et al. Trends in Major Lower Limb Amputation Related to Peripheral Arterial Disease in Hungary: A Nationwide Study (2004-2012). Eur J Vasc Endovasc Surg. 2015; 50: 78-85.
- de Jesus-Silva SG, de Oliveira JP, Brianezi MHC, de Moraes Silva MA, Krupa AE, Cardoso RS. Analysis of risk factors related to major and minor lower limb amputations in a tertiary hospital. J Vasc Bras. 2017; 16: 16-22.
- Seidel AC, Nagata AK, De Almeida HC, Bonomo M. Epistemology of lower limb amputations and debridements at Hospital Universitário de Maringá Epistemology of lower limb amputations and debridements at Hospital Universitário de Maringá. 2008; 7: 308- 315.
- Nugroho MB. Zollinger Atlas of Surgery. J Chem Info Mod. 2013; 53.
- Maloney TR, Dilkes-Hall IE, Vlok M, Oktaviana AA, Setiawan P, Priyatno AAD, et al. Surgical amputation of a limb 31,000 years ago in Borneo. Nature. 2022; 609: 547-551.
- Mellick SA. Rediscovering vascular surgery: Of arterial injury and amputation. Med J Aust. 1998; 168: 352-353.
- Assumpção EC, Benjamin Pitta G, Lisboa De Macedo AC, Borges De Mendonça G, Christyne L, De Albuquerque A, et al. Comparison of risk factors for major and minor amputation in diabetic patients included in a Family Health Program. J Vasc Bras. 2009; 8.
- Donohue SJ. Lower limb amputation 1: indications and treatment.
- Silva Carvalho F, Clarice Kunz V, Zafanelli Depieri T, Cervelini R. PREVALENCE OF VASCULAR INFERIOR MEMBER AMPUTATION: ANALYSIS OF REPORTS. Arq. Ciênc. Saúde Unipar. 2005; 9.
- Boulton AJM. Diabetic foot - what can we learn from leprosy? Legacy of Dr. Paul W. Brand. Diabetes Metab Res Rev. 2012; 28: 3-7.
- Helm P, Engel T, Holm A, Kristiansen VB, Rosendahl S. Function after lower limb amputation. Acta Orthop. 1986; 57: 154-157.
- de Souza YP, Dos Santos ACO, de Albuquerque LC. Characterization of amputees at a large hospital in Recife, PE, Brazil. J Vasc Bras. 2019; 18.
- Ambler GK, Brookes-Howell L, Jones JAR, Verma N, Bosanquet DC, Thomas-Jones E, et al. Development of Core Outcome Sets for People Undergoing Major Lower Limb Amputation for Complications of Peripheral Vascular Disease. Eur J Vasc Endovasc Surg. 2020; 60: 730-738.
- Thorud JC, Plemmons B, Buckley CJ, Shibuya N, Jupiter DC. Mortality After Nontraumatic Major Amputation Among Patients With Diabetes and Peripheral Vascular Disease: A Systematic Review. J Foot and Ankle Surg. 2016; 55: 591-59.
- Fortington LV, Geertzen JHB, Van Netten JJ, Postema K, Rommers GM, Dijkstra PU. Short and long term mortality rates after a lower limb amputation. Eur J Vasc Endovasc Surg. 2013; 46: 124-131.
- Cardoso NA, Cisneros L de L, Machado CJ, Procópio RJ, Navarro TP. Risk factors for mortality among patients undergoing major amputations due to infected diabetic feet. J Vasc Bras. 2018; 17: 296- 302.
Rolim D, Sampaio S, Gonçalves-Dias P, Almeida P, Almeida-Lopes J, Teixeira JF. Mortality after amputation. Angiologia e Cirurgia Vascu. 2015; 11: 166-170.- Cruz CP, Eidt JF, Capps C, Kirtley L, Moursi MM. Major lower extremity amputations at a Veterans Affairs hospital. Am J Surg. 2003; 186: 449-454.
- Aulivola B, Hile CN, Hamdan AD, Sheahan MG, Veraldi JR, Skillman JJ, et al. Major Lower Extremity Amputation Outcome of a Modern Series Hypothesis. Arch Surg. 2004; 139: 395-399.
- Mayfield JA, Reiber GE, Maynard C, Czerniecki JM, Caps MT, Sangeorzan BJ. Survival following lower-limb amputation in a veteran population. J Rehabil Res Dev. 2001; 38: 341-355.
- dos Santos KPB, da Luz SCT, Mochizuki L, d’Orsi E. Burden of disease for lower limb amputations attributable to diabetes mellitus in the State of Santa Catarina, Brazil, 2008-2013. Cad Saude Publica. 2018; 34.
- Chamlian TR, Varanda R dos R, Pereira CL, Resende JM de, Faria CC de. Epidemiological profile of lower limb amputees patients assisted at the Lar Escola São Francisco between 2006 and 2012. Acta Fisiátrica. 2013; 20: 219-223.
- Ferreira GP, Gonçalves JV, Branco Liposcki D. Epidemiological profile of amputee patients treated at a public rehabilitation center. Fisioterapia Brasil. 2022; 23: 798-812.
- Guarinello GG, D’Amico RC, Miranda ANM, Novack J, Coral FE. Impact of COVID-19 on the surgical profile of vascular surgery patients at a referral service in Curitiba. J Vasc Bras. 2022; 21.