Post-Traumatic Tsteomyelitis of the Cierny-Mader IV Femur Treated with an External Fixation Stent Combined with Loaded Calcium Sulfate
- 1. Department of Orthopedics, Hospital of Xinjiang Medical University, China
- 2. Department of Microrepair and Reconstructive Surgery, Hospital of Xinjiang Medical University, Chinaa
Abstract
Background: Good results have been achieved by using external fixation stents combined with drug-loaded calcium sulfate in the treatment of Cierny-Mader type IV post- traumatic osteomyelitis of the femur, but fewer clinical studies have been reported.
Methods” The purpose of this study is to investigate the application of this method for the treatment of Cierny-Mader type IV post-traumatic osteomyelitis of the femur to control infection, repair bone defects, use an use an external fixation bracket to provide stable bone support and protection, reduce interfracture mobility, promote repair and regeneration of bone tissue, improve the rate of healing of osteomyelitis, and explore the clinical efficacy and advantages of this method.
Results: Twelve patients were treated with loaded calcium sulfate, and the antibiotics chosen were vancomycin in 11 cases and vancomycin combined with gentamicin in one case, with a follow-up period of 31-49 months and a mean follow-up period of 39.17 months. The results of serological examination showed that WBC, CRP, and ESR were lower at 1 month postoperatively than preoperatively, and the difference was statistically significant (P<0.05). PCT and IL-6 were lower at 1 month postoperatively than preoperatively, but the difference was not statistically significant (P > 0.05). Twelve cases of osteomyelitis were cured without recurrence, and according to the Paley scoring system, 5 cases were excellent, 5 cases were good, and 2 cases were poor, with an excellent rate of 83.33%. According to the LEFS grading criteria, 6 cases were excellent, 4 cases were good, and 2 cases were poor, with an excellent rate of 83.33%. According to the Likert satisfaction scale, 9 cases were very satisfied, 2 cases were satisfied, and 1 case was fair, with an excellent satisfaction rate of 91.67%. After treatment with the external fixation stent combined with drug-carrying calcium sulphate, all patients achieved more satisfactory clinical efficacy.
Conclusion: For the treatment of Cierny-Mader type IV post-traumatic osteomyelitis of the femur, external fixation stents in combination with drug-loaded calcium sulphate are a better option because they are dependable, have fewer surgical complications, and have a lower recurrence rate.
KEYWORDS
- Post-traumatic osteomyelitis of the femur
- External fixation bracket
- Loaded with calcium sulphate
- Vancomycin
CITATION
Li L, Yusufu A, Liu D, Zhang Q, He X, et al. (2024) Post-Traumatic Tsteomyelitis of the Cierny-Mader IV Femur Treated with an External Fixa- tion Stent Combined with Loaded Calcium Sulfate. JSM Bone and Joint Dis 4(1): 1016.
BACKGROUND
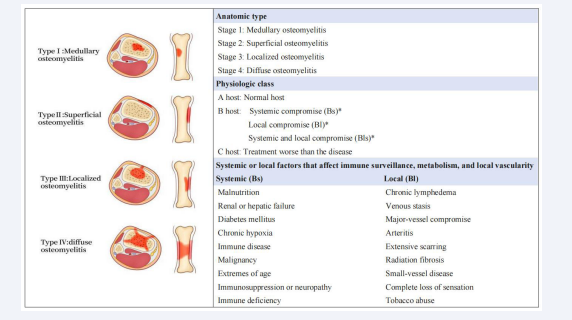
Traumatic femur fracture is a common clinical fracture, mostly caused by high-energy injuries, and its preferred treatment is intramedullary nailing with internal fixation [1]. Intramedullary infection is one of the most common and serious complications after intramedullary nailing, and untimely treatment will develop into chronic traumatic osteomyelitis [2]. Cierny-Mader typing is the classification of osteomyelitis into four anatomical stages, and Cierny-Mader type IV, also known as diffuse osteomyelitis, is the most severe and difficult to treat type, mainly due to the bone structure and its instability [3]. Its high recurrence and disability rates impose a huge economic burden on patient care [4]. Cierny-Mader typing includes anatomical typing and host typing Figure 1, and when clinically selecting a treatment strategy,
Figure 1: Cierny–Mader staging system
it is necessary to combine the 2 aspects of patient anatomical typing and host typing for comprehensive consideration [5]. In some cases, the infected foci are located within the femoral bone tissue and the lesion is large, making it difficult to completely remove the infected foci and achieve a stable repair with conventional surgery, which may result in dead space [6], and the problem of drug resistance may be faced during the use of antibiotics, leading to ineffective treatment [7,8]. In recent years, external fixation stent combined with drug-carrying calcium sulfate has been applied to treat Cierny-Mader type IV post-traumatic osteomyelitis of the femur, but the method and effectiveness of treatment are not very clear, and at present, there are fewer domestic and foreign studies on the external fixation stent combined with drug-carrying calcium sulfate for the treatment of Cierny-Mader type IV post-traumatic osteomyelitis of the femur. We treated Cierny-Mader type IV post-traumatic osteomyelitis of the femur with an external fixation stent combined with drug- carrying calcium sulfate to control the infection and repair the bone defect. The external fixation stent provides stable bone support and protection, reduces interfracture mobility, promotes the repair and regeneration of bone tissues, and improves the healing rate of osteomyelitis. We discuss the clinical efficacy and advantages of it and evaluate its therapeutic efficacy and prognosis.
METHOD
Study design and setting
Patients with osteomyelitis of the femur treated in our unit from January 2018 to June 2022 were retrospectively analyzed. Eighteen cases were retrieved on the case system based on keywords, and 12 eligible patients were screened according to the inclusion and exclusion criteria; one was amputated, two were not treated with an external fixation frame combined with drug-carrying calcium sulfate, and the remaining three were lost to follow-up. Inclusion criteria: 1) patients were ≤70 years old; 2) osteomyelitis after femoral trauma; 3) osteomyelitis was graded as IV type according to the Cierny-Mader grading system; 4) patients had intact function of the contralateral lower limb; 5) they could tolerate the surgery and did not suffer from severe underlying diseases; and 6) follow-up time was ≥12 months. Exclusion criteria: 1) combined severe osteoporosis; 2) combined severe organ injury; 3) amputee; 4) patients with allergy to calcium sulfate; 5) patients who could not cooperate with the treatment or lost the visit; Clinical data collected included age, gender, clinical history, preoperative assessment data, serum inflammatory indexes (White Blood Cell Count (WBC), Erythrocyte Sedimentation Rate (ESR), and C Reactive Protein (CRP) levels, procalcitonin (PCT), interleukin 6 (IL6)), bacterial culture results, etiology, imaging data, location of osteomyelitis (left/right), number of surgeries, type of calcium sulfate-loaded antibiotics, number of days in the hospital, and follow-up time. Studies involving human participants were reviewed and approved by the Fourth Affiliated Hospital of Xinjiang Medical University, and participants or legal guardians/next of kin of the participants provided written informed consent to participate in this study.
Surgical methods
Preoperative: After the patients were admitted to the hospital, we fully understood the patients’ medical history, the number of previous surgeries and medications, and whether they had a history of diabetes mellitus, hypertension, and coronary artery disease. We actively improved the preoperative examinations and clarified the site and extent of the infection through imaging examinations (X-ray, CT, or MRI) and laboratory examinations (blood routine, coagulation four, biochemical complete set, ESR, CRP, PCT, IL6, blood group identification, etc.) to rule out contraindications. Bacterial culture and drug susceptibility testing were performed on secretions or necrotic tissue from the lesion area to determine the type of antibiotic to be used with drug-loaded calcium sulfate and the choice of anti- infective drugs.
During the operation: Silent suction combined general anaesthesia and lumbar epidural anaesthesia were performed. After the anaesthesia took effect, the patient was placed supine with a pillow placed under the buttocks. A tourniquet was used for control, and the affected limb was routinely disinfected and covered with a sterile towel. Based on preoperative imaging, the site and extent of infection were clarified. First, the internal fixation device was removed, and then a surgical plan was developed for radical debridement. The skin was incised layer by layer from shallow to deep, and the necrotic sclerotic bone,
inflammatory granulation tissue, and infected necrotic tissue at the trauma site were thoroughly excised down to the normal tissue layer. The depth of the cavity is probed with a probe, and a window is opened along the cavity with a bone cutter. The area is then scraped with a curette layer by layer until normal cortical bone is scraped. The medullary cavity is thoroughly removed until spotting of bleeding occurs on the surface of the cortical bone (known as the pepper sign, which has an indistinct border and can be determined by using rapid intraoperative freezing to determine if the bone tissue has been adequately removed). Samples of deep tissue and scraped dead bone are taken for bacterial culture, drug sensitivity testing, and pathological examination, followed by rinsing with copious amounts of saline. Under C-arm fluoroscopy, the metaphysis on the side opposite to the bone defect was selected, which had good soft tissue coverage and high osteogenic potential. Based on the location of the bone defect and the length of the distal and proximal bone segments, a plan for assembling the external fixation bracket was designed. The distal and proximal femurs are drilled according to the surgical plan, and four to six 6-mm-diameter external fixation screws are placed from the lateral aspect of the femur, penetrating the cortex of the opposite side of the bone. The remaining external fixation screws have been installed, and the drilling process has been conducted in a manner that avoids damage to the neurovascular system. It is essential that the external fixation screws are positioned perpendicular to the longitudinal axis of the femur, parallel to one another, and in the same plane. The Orthofix reconstructive external fixation bracket should be assembled with due attention paid to ensuring the length of the affected limb and the line of force are accurate, so that the two articular surfaces of the broken end are parallel. The lengthening knob should be set in the position of the pre-truncated bone, while the pressurising knob should be set on the broken end of the bone defect. The choice of antibiotics was made on the basis of the size of the bone defect and the results of bacterial culture and drug susceptibility testing. Drug-carrying calcium sulfate (Stimulan®, Biocomposites Ltd., Keele, England) was implanted into the femoral bone defect after proper contouring. Once the implant had solidified, the wound was flushed again, and the drainage tube was left in the medullary cavity. The wound was then closed by layer-by-layer suture.
Postoperative: Intravenous antibiotics were administered to all patients following surgical procedures as a standard protocol. The duration of antibiotic administration was determined according to the patient’s temperature, C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), white blood cell (WBC) count, procalcitonin (PCT), interleukin-6 (IL6) levels, and the results of other tests. The dressing was changed, and the drainage tube was removed 24 to 48 hours after surgery, contingent on the condition of the wound. On a daily basis, 75% alcohol or povidone-iodine should be used to disinfect Kirschner’s needles or external fixation screws, with particular attention paid to the areas that come into contact with the skin. Additionally, sterile gauze is employed to fill and wrap the traction needles, thereby preventing needle tract infection. Two days following the surgical procedure, patients were encouraged to commence rehabilitation exercises to facilitate flexion and extension of the knee joint. This was undertaken to prevent joint contracture and reduce the swelling and pain of the affected limb. The control of postoperative infection was determined by the results of X-rays and laboratory tests. Following the initial postoperative period, X-ray films were reviewed at one-week, one-month, two-month, three-month, and six-month intervals. During these reviews, patients were instructed to maintain the operative area and pin tract in a clean and dry state. They were also advised to attend the hospital at the specified time, monitor the warmth of the affected limbs, and perform the recommended functional exercises. The X-ray film demonstrated that the newborn bone scab was solid and well ossified, that the fracture had healed, that the external fixation frame had been removed at the appropriate time, and that the patient had been instructed to commence rehabilitation and functional training in the subsequent stage of their treatment.
Evaluation criteria
- The efficacy of the treatment was evaluated using the Paley scoring system, which is based on several criteria, including knee mobility, lengthening length, gait, force line offset, pain, and daily work-life ability. The scores were classified as excellent (95-100 points), good (75-94 points), intermediate (40-74 points), or poor (<40 points).
- Lower Extremities Functional Scale [10] (LEFS), with a score of 80 points, 0-4 points for each item, 0 points for extreme difficulty or inability to perform the activity, 1 point for great difficulty, 2 points for moderate difficulty, 3 points for a little difficulty, and 4 points for no difficulty, with the following criteria for evaluation: 70-80 points for excellent, 60-69 points for good, 50-59 points for good, 40-74 points for poor, and <40 points for poor. 50-59 points; poor <50 points.
- Likert satisfaction scale was used to evaluate patients’ satisfaction, which was categorized as very satisfied, satisfied, average, dissatisfied, and very dissatisfied.
Statistical analysis
All data were statistically analyzed using SPSS 25.0 software. Measurement data were expressed as mean ± standard deviation (-x±s). Data before and after treatment were analyzed using paired-samples t-test or Wilcoxon signed rank test, and differences were considered statistically significant at P<0.05.
RESULTS
A total of 12 patients with post-traumatic osteomyelitis of the femur were identified as Cierny-Mader type IV, comprising 8 males and 4 females with a mean age of consultation of 40.08 years (ranging from 14 to 69 years). Four patients (33.33%) had additional medical conditions, including hypertension, type 2 diabetes mellitus, gentamicin allergy, penicillin allergy, and the location of the injury. Ten cases were located on the left side, and two were located on the right side. The causes of injury are as follows: Five cases were attributed to traffic accidents, four to falls from height, two to horseback riding, and one to being struck by a tree. The symptoms of morbidity were predominantly characterised by redness, swelling, pain, skin breakdown, and the formation of sinus tracts. In a few cases, these symptoms were accompanied by fever. Two cases manifested the symptoms of morbidity as vague pain and pain, respectively. The location of occurrence was the proximal one-third of the femur in three cases, the middle one-third of the femur in six cases, and the middle-distal one-third in two cases. In two cases, the proximal one-third of the femur was affected, while in one case, the distal one-third was affected. The majority of the abnormal serological indexes were CRP, ESR, WBC, and IL6. The 11 cases were treated with vancomycin-loaded calcium sulfate, while one case opted for vancomycin combined with gentamicin-loaded calcium sulfate implantation. Bacterial cultures of all 1 patient were diagnosed with methicillin-resistant Staphylococcus aureus (MRSA) infections. In one case, vancomycin was used to treat the infection, while cefazolin sodium was employed in three cases and cefuroxime sodium in six cases. Clindamycin was used in one patient who was allergic to cefazolin sodium and cefuroxime sodium, as well as in one instance of penicillin sodium for anti- infection purposes. The follow-up period spanned a duration of 31 to 49 months, with a mean follow-up time of 39.17 months. At the six-month postoperative follow-up, X-rays demonstrated a gradual resorption of the drug-carrying calcium sulfate, osteogenesis induced by the drug-carrying calcium sulfate in the area of the fracture and bone defects, localized scab formation, and gradual The restoration of bone continuity was evident at the final follow-up, as demonstrated by the X-ray, which showed blurred boundaries of the plastinated loaded calcium sulfate, mature osteoinduction and bone remodeling, restoration of both osteocortical continuity, and a patent medullary cavity. Typical case pictures are shown in Figure 2.
Figure 2: Patient, male, 58 years old, presented with osteomyelitis of the left femur after a traffic accident. a-b Pre-operative X-rays showed that the left femur was internally fixed and infected. c-e Intra-operative removal of the internal fixation and removal of the dead bone. f-g X-rays one day after implantation of external fixation bracket combined with drug-carrying calcium sulphate showed that the drug-carrying calcium sulphate was anastomosed with the bone defect site. h-k, i-m X-rays at 6 months after surgery showed that the drug-carrying calcium sulphate was gradually absorbed and the external fixation bracket was stabilised. X-rays at 6 months after h-k and i-m showed that the drug-loaded calcium sulphate in the bone defect was gradually absorbed and the external fixation bracket was stable; n-p X-rays at 10 months after the operation showed that the bone defect had healed well and it was proposed to remove the external fixation bracket. q-v X-rays at 24 months after the operation showed that the bone defect had healed well, and the affected limb was fully loaded and could maintain basic daily life, even though there was stiffness in the joints.
Of the 12 cases of osteomyelitis, 12 were successfully treated, with no recurrence observed. According to the Paley scoring system, 5 cases were classified as excellent, 5 as good, and 2 as poor, resulting in an overall excellent rate of 83.33%. In accordance with the LEFS evaluation criteria, six cases were classified as excellent, four as good, and two as poor, resulting in an overall excellent rate of 83.33%. According to the Likert satisfaction scale, nine cases were classified as ‘very satisfied’, two as ‘satisfied’, and one as ‘fair’. This yielded an overall excellent satisfaction rate of 91.67%. Following treatment with an external fixation stent in conjunction with drug-carrying calcium sulfate, all patients exhibited enhanced clinical outcomes (Table 1).
Table 1: Patient Data
|
Patient number |
Age |
sex |
Side |
Disease time |
Symptoms |
co- morbidity |
cause of disease |
Causative agent |
Anti- infection drugs |
Drug calcium sulfate species |
Abnormal Serological Indicators |
Time of onset (months) |
Paley Rating |
The LEFS Scale |
Likert Satisfaction Scale |
|
1 |
58 |
M |
L |
In June, 2018 |
Redness, pain, swelling, broken skin |
hypertensive disease |
traffic accidents |
MRSA |
Cephazolin sodium |
vancomycin |
CRP,ESR,IL6 |
48 |
excellent |
excellent |
very satisfied |
|
2 |
16 |
F |
L |
In August, 2019 |
Redness, pain, |
None |
Falling from heights |
MRSA |
Cephazolin sodium |
vancomycin |
WBC,CRP,ESR,PCT,IL6 |
43 |
excellent |
excellent |
very satisfied |
|
3 |
14 |
M |
L |
In July, 2019 |
hidden anguish |
penicillin allergy |
traffic accidents |
MRSA |
clindamycin |
Vancomycin was combined with gentamicin |
CRP,ESR,IL6 |
36 |
good |
good |
very satisfied |
|
4 |
28 |
F |
L |
In April, 2018 |
Redness, pain, swelling, sinuses, broken skin |
Gentamicin allergy |
traffic accidents |
MRSA |
cefuroxime sodium |
vancomycin |
WBC,CRP,ESR,IL6 |
38 |
good |
good |
pleased |
|
5 |
69 |
M |
L |
In September, 2019 |
Redness, swelling, pain, fever, broken skin |
None |
traffic accidents |
MRSA |
cefuroxime sodium |
vancomycin |
WBC,ESR,PCT |
34 |
good |
good |
very satisfied |
|
6 |
29 |
F |
L |
In May, 2021 |
Pain |
None |
Falling from heights |
MRSA |
cefuroxime sodium |
vancomycin |
WBC,CRP,ESR,IL6 |
35 |
excellent |
excellent |
very satisfied |
|
7 |
59 |
M |
R |
In August, 2021 |
Redness, pain, swelling, sinuses, broken skin |
Type 2 diabetes |
Falling from heights |
MRSA |
cefuroxime sodium |
vancomycin |
WBC,CRP,ESR |
32 |
difference |
difference |
general |
|
8 |
62 |
M |
L |
In September, 2021 |
Redness, pain, swelling, sinuses, broken skin |
None |
Injured by a tree |
MRSA |
penicillin sodium |
vancomycin |
WBC,CRP,ESR,IL6 |
31 |
excellent |
excellent |
very satisfied |
|
9 |
15 |
M |
L |
In August, 2019 |
Redness, pain, swelling, fever, broken skin |
None |
Injury from horseback riding |
MRSA |
vancomycin |
vancomycin |
WBC,CRP,ESR,IL6 |
34 |
good |
excellent |
very satisfied |
|
10 |
42 |
M |
L |
In February, 2018 |
Redness, swelling, pain, fever, broken skin |
None |
traffic accidents |
MRSA |
cefuroxime sodium |
vancomycin |
WBC,CRP,ESR,PCT,IL6 |
49 |
good |
good |
very satisfied |
|
11 |
55 |
F |
L |
In January, 2019 |
Redness, swelling, pain, fever, broken skin |
None |
Injury from horseback riding |
MRSA |
cefuroxime sodium |
vancomycin |
WBC,CRP,ESR,IL6 |
42 |
excellent |
excellent |
very satisfied |
|
12 |
34 |
M |
R |
In August, 2019 |
Redness, pain, swelling, sinus tracts, broken skin |
None |
Falling from heights |
MRSA |
Cephazolin sodium |
vancomycin |
WBC,CRP,ESR,PCT,IL6 |
48 |
difference |
difference |
pleased |
|
Abbreviation: White Blood Cell Count (WBC ), Erythrocyte Sedimentation Rate (ESR), and C Reactive Protein (CRP) levels, procalcitonin (PCT), interleukin 6 (IL6),Methicillin-resistant Staphylococcus aureus (MRSA) |
|||||||||||||||
The results demonstrated a statistically significant reduction in WBC, CRP, and ESR one month following the operation when compared to the preoperative levels (P < 0.05). Conversely, while PCT and IL-6 exhibited a decline at the one-month postoperative period, this did not reach statistical significance (P > 0.05) [Table 2].
Table 2: Preoperative and postoperative analysis of serum inflammatory indicators
|
Serological indicators |
Preoperative |
1 month postoperative |
t/Z |
P value |
|
WBC(109/L) |
8.93±4.61 |
6.07±1.52 |
2.919 |
0.004 |
|
CRP(mg/L) |
58.22±59.04 |
17.15±19.78 |
3.296 |
0.001 |
|
ESR(mm/h) |
64.57±38.22 |
43.57±38.22 |
3.210 |
0.001 |
|
PCT(109/L) |
0.20±0.35 |
0.11±0.14 |
0.316 |
0.752 |
|
IL-6(ng/L) |
16.74±13.84 |
15.72±12.75 |
-0.282 |
0.778 |
|
Serum inflammation index: white blood cell count (WBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), procalcitonin (PCT), Interleukin 6 (IL6) level. |
||||
DISCUSSION
The treatment strategies for Cierny-Mader type IV post- traumatic osteomyelitis of the femur have undergone significant developments over the past few decades [11]. The current standard of care for this condition includes antibiotic therapy, debridement, elimination of dead space, soft tissue coverage, maintenance of stabilization, and reconstruction [12]. The treatment of post-traumatic osteomyelitis in Cierny-Mader type IV femur is particularly challenging, as it requires the filling of the residual cavity, repair of the bone defect, control of the infection, and stabilisation of the affected area. The objective is to promote fracture healing at the broken end. The selection of antibiotics with the appropriate sensitivity profile, based on the characteristics of bacterial resistance, has become a crucial aspect of the anti- infective treatment of Cierny-Mader type IV post-traumatic osteomyelitis of the femur. Patzakis et al. have demonstrated that 65% to 70% of cases of traumatic osteomyelitis are caused by S. aureus [13]. The selection of appropriate antibiotics, according to the infecting species and the results of drug sensitivity tests, and the administration of early, adequate doses of antibiotics for an adequate course in an effective manner represent the most important aspects of the treatment of this condition [14]. The selection of antibiotics should satisfy a number of criteria, including a broad antimicrobial spectrum, safety, heat stability, water solubility, and hypoallergenicity [15]. However, it is notable that no single antibiotic currently available has demonstrated satisfactory results in all of these areas. Aminoglycoside antibiotics, such as gentamicin, and glycopeptide antibiotics, such as vancomycin, are the most commonly employed in the treatment of post-traumatic osteomyelitis. Aminoglycoside antibiotics offer a broad antimicrobial spectrum, good thermal stability, and good absorption. However, the current clinical resistance situation is more serious, and the application of single aminoglycoside antibiotics is generally effective [16]. In light of the current rise in antibiotic-resistant bacterial strains, it is imperative to develop tailored and efficacious anti-infective treatment regimens for patients based on the results of their bacterial cultures and drug sensitivity tests. In certain cases, the use of multiple antibiotics in combination may be necessary.
Cierny-Mader type IV post-traumatic osteomyelitis of the femur is characterised by a wide range of infected foci and extensive necrotic tissue. In order to control the infection, radical destruction is required. A comprehensive assessment of the patient’s condition should be conducted prior to performing debridement in order to ascertain the extent of the lesion and infection and to prevent inadvertent debridement [17]. Murphy et al., have stated that for chronic osteomyelitis, debridement should be comprehensive, removing all periwound fibrotic and ischemic bone and soft tissues that impede antibiotic penetration [18]. Radical debridement is an effective method for removing necrotic bone and inflammatory foci around the lesion. It has been demonstrated to be more effective in reducing the risk of infection recurrence, which is an inevitable consequence of incomplete debridement [19,20].
In clinical practice, the surgical protocols most commonly employed for the treatment of Cierny-Mader type IV post- traumatic osteomyelitis of the femur include the Masquelet technique, the Ilizarov technique, free fibula grafting (autologous free fibula grafting with or without accompanying blood vessels), and allograft bone grafting. Each of these surgical protocols possesses distinct advantages and disadvantages [21]. The Masquelet technique is currently regarded as a significant treatment option for all types of bone defects resulting from debridement. The technique comprises two principal phases: the initial phase, which involves the treatment of radical debridement and the filling of the bone defect with polymethyl methacrylate (PMMA) to induce membrane formation; and the subsequent phase, which encompasses spacer removal and grafting of autogenous cancellous bone. The technique has been widely employed in the treatment of chronic osteomyelitis. Noam Bor and colleagues treated 15 patients with chronic osteomyelitis of Cierny-Mader types I-III and one patient with chronic osteomyelitis of Cierny-Mader type IV with radical debridement in combination. The use of PMMA in the treatment of all patients resulted in the successful control of infection and the absence of recurrence during the late follow-up period. However, this approach is not recommended for patients with Cierny-Mader type IV due to the necessity for extensive bone segment removal in a one-stage procedure, which would require significant reconstruction in a two-stage surgery [22]. Marianne Cuvillier et al., employed the Masquelet technique in conjunction with Reamer Irrigation Aspiration (RIA) and intramedullary nailing (MaRIAN) in the treatment of 12 cases of chronic osteomyelitis of the lower extremities. However, two intramedullary nails fractured and one femoral fracture occurred during the postoperative follow- up period [23]. In a series of 21 patients with Cierny-Mader type III and IV chronic haematogenous osteomyelitis in children, Shi et al. employed the early debridement and Masquelet technique. During the postoperative follow-up, one case underwent a secondary operation to replace the plate with a new one due to an accidental fall, resulting in plate fracture. Additionally, one case developed arthritis. The authors also report one case of a patient who fell one month after the removal of the PMMA, resulting in a bone re-fracture at the defect. Secondary surgery was performed to address this complication [24]. While PMMA has the potential to form an induced membrane, providing a favourable environment for second-stage bone grafting, it is non-degradable, requires a second surgery to remove it after implantation in the human body, and may potentially Secondary damage and the induction of secondary infections are potential complications. The anti-infective function of PMMA reaches its peak 48-72 hours postoperatively; however, the concentration of local antibiotics will decrease dramatically after 72 hours. Furthermore, PMMA carriers may induce bacterial colonization when the concentration of antibiotics is below the threshold required for efficacy. Low concentrations of antibiotics may also promote bacterial resistance, leading to recurrence of infection [22].
Cierny-Mader type IV post-traumatic osteomyelitis of the femur is characterised by a relatively large bone defect following debridement, which can also be accompanied by unstable bone segments. This can result in bone deformity. In response to this condition, the application of the Ilizarov bone handling technique has been proposed for clinical use in the treatment of the aforementioned condition. The Ilizarov technique produces the desired correction during treatment, thus allowing for limb weight-bearing and maintaining joint motion [25]. Peng et al., concluded from a pooled analysis of 590 patients from 24 studies that the Ilizarov technique is an effective treatment for infected nonunion of the tibia and femur [26]. In a systematic evaluation of 37 publications on the clinical outcomes of the Ilizarov method for the treatment of long bone defects of the lower extremity, Pak Kostidis and colleagues demonstrated that the Ilizarov technique significantly reduced the risk of deep infection of infected bone lesions in the segmental defects of the lower extremity that were included in the treatment. However, the incidence of re-fracture was 5%, and the incidence of neurovascular complications was 2%. The amputation rate was 2.9% [27]. Konchada Srikant et al. used the Ilizarov technique in 14 patients with femoral stem fracture. All 14 patients were able to walk with full weight bearing postoperatively. Six patients experienced claudication, 13 had limb shortening of less than 4 centimetres, and one had limb shortening of 5 centimetres [28]. Souvik Paul et al., conducted a comparative analysis of patients with segmental long bone defects of the lower extremity across five studies. In this study, 96 patients underwent treatment using the Illizarov technique, while 72 patients were treated with the autologous free fibula grafting technique with vascularisation. The findings of the study indicated that there was no notable discrepancy between the two treatment modalities with respect to bony and functional outcomes. However, the mean healing time of the autologous free fibular graft with vascularisation was 9.3 months earlier than that of the Illizarov technique. Furthermore, the overall incidence of complications was 68% higher in patients undergoing the Ilizarov technique, and there was no significant difference in the non- healing rate between the two groups [29]. The Ilizarov technique for Cierny-Mader type IV post-traumatic osteomyelitis of the femur Mader type IV post-traumatic osteomyelitis of the femur continues to present a significant challenge, with a high incidence of bone non-union and re-infection, as well as complications such as limb shortening, incorrect alignment of forces, and prolonged treatment duration.
Furthermore, autologous free fibular bone graft without vascularisation represents an additional treatment option for post-traumatic osteomyelitis of the femur in Cierny-Mader type IV. Ali Bas and colleagues conducted a retrospective evaluation of seven patients from 2003 to 2020, utilising autologous free fibular bone graft without vascularisation. During the follow- up period, effective bone regeneration and good healing were confirmed in all cases. However, two patients developed pin- trajectory infection and one patient developed joint contracture [30]. Autologous bone grafting has the advantages of convenience, low cost, and no rejection reaction. However, its disadvantages include limited sources and the necessity of surgery in the donor for allogeneic bone grafting. The area may also be susceptible to local infections. Artificial implants are allogeneic bone, which has a high resorption rate. Long-term implantation is prone to foreign body reaction and rejection. Furthermore, artificial implants are prone to bone disjunctions due to long-term implantation. This necessitates additional surgery to remove the implant, which increases the patient’s pain and financial burden. The use of artificial implants may result in bone dislocation due to the prolonged implantation period, necessitating further surgical intervention to remove the implant. This can lead to increased patient discomfort and economic burden.
While these surgical techniques have yielded favourable outcomes in numerous instances, there are nevertheless some constraints associated with the management of Cierny-Mader type IV post-traumatic osteomyelitis of the femur. In this case, an external fixation stent was employed in conjunction with a drug- loaded calcium sulfate for the treatment of Cierny-Mader IV type post-traumatic femoral osteomyelitis. Radical debridement was performed until the appearance of punctate haemorrhage from the Harvard tube on the surface of the cortical bone (red pepper sign). In cases where lesion boundaries are unclear, intraoperative rapid freezing can be employed to ascertain whether the bone tissue has been completely debrided. A complete debridement is essential, and it is crucial to preserve as much cortical bone as possible to allow for the preservation of the bone wall cavities [32]. Cierny-Mader type IV is the most severe and challenging subtype to treat, characterised by an extremely unstable bone structure. In previous treatments, radical debridement is often employed in phase I as a means of temporarily maintaining stability. This is achieved by filling the dead space with PMMA bone cement, if necessary, and by administering individualised antibiotic therapy following phase I surgery. The bone defect is then reconstructed in phase II [33]. Consequently, the treatment of Cierny-Mader type IV osteomyelitis frequently entails the implantation of drug-carrying calcium sulfate, which is combined with iliac bone grafts to fill bone defects and control infection, and with the combination of external fixation brackets to stabilize bone structure and maintain a favorable biomechanical environment. Cierny-Mader type IV osteomyelitis is typically accompanied by a substantial segmental bone defect, and the utilization of conventional internal fixation surgery is associated with a considerable risk of complications. Cierny- Mader IV osteomyelitis is typically associated with significant bone defects. The external fixation stent can mitigate the risk of delayed healing and pseudoarthrosis by connecting the healthy bone segments and providing stabilising support, thereby reducing the stress burden on the damaged bone segments. Furthermore, the brace can also facilitate some degree of motion, which is conducive to the functional recovery of the affected limb. Furthermore, the external fixation brace offers the additional benefits of a shortened treatment period, minimal damage, and a reduced number of surgical procedures. This approach can help to alleviate pain and accelerate recovery, while also controlling infection and maintaining limb length [34]. In some cases, traditional microbial culture methods may not yield sufficient results in terms of detecting pathogenic microorganisms. In such instances, the use of alternative techniques, such as macrogenomic second-generation sequencing (mNGS) and bacterial whole-genome testing, can enhance the detection rate of pathogenic microorganisms, thereby facilitating more accurate guidance in the treatment of infections [35]. The selection of the calcium sulfate-carrying antibiotic is contingent upon the availability of precise bacterial data, epidemiologic data at the patient’s location, and advancements in clinical research. The most common complication of Cierny-Mader IV post-traumatic osteomyelitis of the femur is knee stiffness or loss of function. According to the Paley scoring system, five cases were classified as excellent, five as good, and two as poor, resulting in an excellent rate of 83.33%. In accordance with the LEFS evaluation criteria, six cases were classified as excellent, four as good, and two as poor, resulting in an overall excellent rate of 83.33%. According to the Likert satisfaction scale, nine cases were classified as ‘very satisfied’, two cases were classified as ‘satisfied’, and one case was classified as ‘fair’. This yields an overall excellent satisfaction rate of 91.67%. Following treatment with an external fixation stent in conjunction with drug-carrying calcium sulfate, all patients exhibited clearance of their infected lesions and demonstrated enhanced clinical efficacy. During the follow-up period, one patient experienced a recurrence of infection in the affected limb following an inadvertent fall 10 months after the initial operation. A second surgical procedure was performed, and during the subsequent follow-up, the patient was able to walk with weight bearing, although they experienced severe claudication, which significantly impacted their daily life. The remaining patients were able to walk with weight bearing, three of whom experienced claudication, while the remainder exhibited a largely normal gait. Nine cases exhibited limb shortening of less than 3 cm, two cases exhibited limb shortening of 4 cm, and one case exhibited limb shortening of 5 cm. The limb shortening was 5 cm in one case, 4 cm in two cases, and 5 cm in one case. Despite three patients presenting with knee joint stiffness, infection control was achieved, and patients were able to bear weight on the ground and maintain basic daily life activities.
In the management of bone defects following debridement, the current clinical application of drug-carrying calcium sulfate has demonstrated the following characteristics: degradability, good biocompatibility, and the gradual and stable release of loaded antibiotics. Additionally, the antibiotic elution rate of calcium sulfate is higher than that of PMMA, obviating the need for a second surgical procedure [36]. Furthermore, calcium sulfate has a composition similar to that of human autologous bone and generates a local space through the degradation of calcium sulfate. In vivo, calcium sulfate does not affect the migration and colonization of autologous bone cells, which has an osteogenic induction effect. Additionally, calcium sulfate does not dissipate heat in vivo, which allows for the use of a wider range of antibiotics [37]. Veenesh Selvaratnam et al., treated 13 patients with Cierny-Mader type IV and 21 patients with Cierny- Mader type I chronic osteomyelitis using gentamicin-loaded calcium sulfate. Only one patient with Cierny-Mader type IV and one patient with Cierny-Mader type I experienced recurrence [38]. Zhou et al. used vancomycin-loaded calcium sulfate implantation in 64 patients with traumatic osteomyelitis of the limb caused by MRSA infection. Only one patient relapsed in the fifth postoperative year after surgery due to new injury at the surgical site during follow-up, with satisfactory results [39]. In a study conducted by Andrea Sambri and colleagues, 93 patients with chronic osteomyelitis were treated with loaded calcium sulfate. Of these patients, 21 experienced recurrence of infection, which may be related to incomplete surgical debridement and a relatively high incidence of aseptic exudate [40]. This highlights a clinical problem that requires further investigation: how to prevent sterile exudation after implantation of drug-carrying calcium sulfate. The majority of aseptic exudation is attributed to the interaction of calcium ions present in the drug-carrying calcium sulfate with soft tissues. Accordingly, the author preserves the bone cortex covered by the periosteum while meticulously excising the wound, and subsequently administers the drug-carrying calcium sulfate into the relatively airtight bone cavity. This approach reduces the contact between the drug- carrying calcium sulfate and the soft tissues, thereby effectively mitigating the incidence of aseptic exudation in the postoperative period. In the treatment of post-traumatic osteomyelitis, the results of bacterial culture and drug sensitivity tests should be used to rationalise the use of sensitive antibiotics. Vancomycin is the preferred antibiotic for patients with gram-positive bacterial infections, whereas tylenol is recommended for gram- negative bacterial infections. Additionally, attention should be paid to the concentration of the antibiotic in bone tissue, and anaerobic bacteria should also be considered when treating conventional bacterial infections [41]. Vancomycin represents the optimal treatment option for MRSA-induced post-traumatic osteomyelitis. The bacterial cultures of 12 patients in this study were all MRSA infections, of which 11 cases were implanted with vancomycin-loaded calcium sulfate. One case was selected for implantation with vancomycin in combination with gentamicin- loaded calcium sulfate. This approach not only achieves a local anti-infective effect but also promotes the generation of new bone and effectively controls systemic infections. The results were satisfactory.
In the treatment of bone defects resulting from debridement procedures, the use of drug-loaded calcium sulfate is a viable option. It is our contention that drug-loaded calcium sulfate offers a number of significant advantages. Firstly, it is capable of delivering a high concentration of antibiotics to the infected lesion in a precise and targeted manner, prolonging the release time of the drug and providing a long-lasting effect. Secondly, it is structurally stable, biocompatible and safe, thereby reducing the risk of adverse events. Thirdly, it is capable of filling bone defects and does not dissipate heat within the body, thus obviating the necessity for a second surgical procedure to remove it. Fourthly, calcium sulfate is compositionally analogous to human autologous bone, and exhibits a degree of induced osteogenesis and vascularized membrane formation, thereby providing a protective barrier of an abundant blood supply to the bone graft area. Additionally, this approach can reduce the overall treatment period, decrease associated costs, and limit the adverse effects of bone grafting. The combination of an external fixation stent and drug-loaded calcium sulfate represents a promising strategy for addressing Cierny-Mader type IV post-traumatic osteomyelitis of the femur.
It should be noted that this study is not without limitations. Firstly, the study was designed as a single-centre retrospective study, which may have introduced selection and indication bias. Secondly, the study was conducted with a relatively small sample size, comprising only 12 patients.
REFERENCES
- Lu V, Zhang J, Zhou A, Matija Krkovic. Management of post- traumatic femoral defects with a monorail external fixator over an intramedullary nail. Eur J Orthop Surg Traumatol. 2022; 32: 1119- 1126.
- Rodham P, Panteli M, Vun J, Paul Harwood, Peter V Giannoudis. Lower limb post-traumatic osteomyelitis: a systematic review of clinical outcomes. Eur J Orthop Surg Traumatol. 2023; 33: 1863-1873.
- Tan Y, Li H, Pan Z, Qiang Zheng. Modified algorithm for managing postoperative osteomyelitis following fracture fixation with Cierny- Mader type. J Orthop Surg Res. 2020; 15:212.
- Peng P, Dong Z G, Liu L, et al. An Effective Technique for Managing the Calcaneus Osteomyelitis Combined with Soft-Tissue Defect. Int J Low Extrem Wounds. 2023; 22: 393-400.
- Cierny G 3rd, Mader JT, Penninck JJ. A clinical staging system for adult osteomyelitis. Clin Orthop Relat Res. 2003; 414: 7-24.
- Arshad Z, Aslam A, Lau E, Thahir A, Krkovic M. Management of Polymicrobial Cierny-Mader Grade 3 and 4 Chronic Osteomyelitis of the Femur. Cureus. 2021; 13: 12818.
- Cortés-Penfield NW, Kulkarni PA. The History of Antibiotic Treatment of Osteomyelitis. Open Forum Infect Dis. 2019; 6: 181.
- Kavanagh N, Ryan EJ, Widaa A, Sexton G, Fennell J, Kerrigan SW, et al. Staphylococcal Osteomyelitis: Disease Progression, Treatment Challenges, and Future Directions. Clin Microbiol Rev. 2018; 31: 84- 17.
- Marwan Y, Cohen D, Alotaibi M, et al. Cosmetic stature lengthening: systematic review of outcomes and complica?tions. Bone Joint Res. 2020; 9: 341-350.
- Mehta SP, Fulton A, Quach C, Thistle M, Toledo C, Evans NA. Measurement Properties of the Lower Extremity Functional Scale: A Systematic Review. J Orthop Sports Phys Ther. 2016; 46: 200-16.
- Ilizarov GA. The tension-stress effect on the genesis and growth of tissues. Part I. The influence of stability of fixation and soft-tissue preservation. Clin Orthop Relat Res. 1989; 238: 249-81.
- Lazzarini L, Mader JT, Calhoun JH. Osteomyelitis in long bones. J Bone Joint Surg Am. 2004; 86:2305-18.
- Patzakis MJ, Wilkins J, Kumar J, Holtom P, Greenbaum B, Ressler R. Comparison of the results of bacterial cultures from multiple sites in chronic osteomyelitis of long bones. A prospective study. J Bone Joint Surg Am. 1994; 76: 664-666.
- Yang J, Yao JL, Wu ZQ, et al. Current opinions on the mechanism, classification, imaging diagnosis and treatment of post-traumatic osteomyelitis. Chin J Traumatol. 2021; 24: 320-327.
- 15. Subramanyam KN, Mundargi AV, Prabhu MV, et al. Surgical management of chronic osteomyelitis: Organisms, recurrence and treatment outcome. Chin J Traumatol. 2023; 26: 228-235.
- Hriouech S, Akhmouch AA, Mzabi A, et al. The Antistaphylococcal Activity of Amoxicillin/Clavulanic Acid, Gentamicin, and 1,8-Cineole Alone or in Combination and Their Efficacy through a Rabbit Model of Methicillin-Resistant Staphylococcus aureus Osteomyelitis. Evid Based Complement Alternat Med. 2020; 2020: 4271017.
- Zhang Xinling,Chen Yujie,Xiao Xiaodi,Wang Zheng,Yang Xin, et al. Application of VSD technique in adults with chronic osteomyelitis of the extremities combined with soft tissue defects. Int wound J. 2022; 20.
- Murphy C, Atkin L, Vega D C M, et al. Embedding Wound Hygiene into a proactive wound healing strategy. J Wound Care. 2022; 31: S1-S19.
- Subramanyam K N, Mundargi A V, Prabhu M V, et al. Surgical management of chronic osteomyelitis: Organisms, recurrence and treatment outcome. Chin J Traumatol. 2023; 26: 228-235.
- Cobb L H, McCabe E M, Priddy L B. Therapeutics and delivery vehicles for local treatment of osteomyelitis. J Orthop Res. 2020; 38: 2091- 2103.
- Hulsen DJW, Mitea C, Arts JJ, Loeffen D, Geurts J. Diagnostic value of hybrid FDG-PET/MR imaging of chronic osteomyelitis. Eur J Hybrid Imaging. 2022; 6: 15.
- Bor N, Dujovny E, Rinat B, Rozen N, Rubin G. Treatment of chronic osteomyelitis with antibiotic-impregnated polymethyl methacrylate (PMMA)-the Cierny approach: is the second stage necessary?. BMC Musculoskelet Disord. 2022; 23: 38.
- Cuvillier M, Meucci JF, Cazorla C, Carricajo A, Neri T, Boyer B. Masquelet’s induced membrane technique associated with Reamer Irrigation Aspiration grafting and intramedullary Nailing (MaRIAN) for chronic diaphyseal osteomyelitis of the lower limb. Orthop Traumatol Surg Res. 2022; 108: 103395.
- Shi J, Yang X, Song M, Zhang X, Xu Y. Clinical effects of early debridement, internal fixation, and Masquelet technique for childhood chronic haematogenous osteomyelitis of long bones. J Orthop Surg Res. 2023; 18: 11.
- Yang H Q, Qu L. [Ilizarov bone transport technique]. Zhongguo Gu Shang. 2022; 35: 903-907.
- Yin P, Ji Q, Li T, Li J, Li Z, Liu J, et al. A Systematic Review and Meta- Analysis of Ilizarov Methods in the Treatment of Infected Nonunion of Tibia and Femur. PLoS One. 2015; 10: e141973.
- Papakostidis C, Bhandari M, Giannoudis PV. Distraction osteogenesis in the treatment of long bone defects of the lower limbs: effectiveness, complications and clinical results; a systematic review and meta- analysis. Bone Joint J. 2013; 95-B: 1673-1680.
- Srikant K, Soni A, Pradhan S, Gulia A, Sandeep B, Kafley R, et al. Ilizarov Fixator-Assisted Management of Neglected Femur Fractures by Open Intramedullary Nailing: A Case Series. Cureus. 2023; 15: e50864.
- Paul S, Vathulya M, Kandwal P, Jagtap M, Behl R. Comparative analysis of free vascularized fibula grafting and Ilizarov bone transport in management of segmental long bone defect of the lower limb: A systematic review and meta-analysis. J Orthop. 2023; 50: 84-91.
- Bas A, Balci HI, Kocaoglu M, Demirel M, Kochai A. Augmentation with a non-vascularized autologous fibular graft for the management of Cierny-Mader type IV chronic femoral osteomyelitis: a salvage procedure. Int Orthop. 2024; 48: 439-447.
- Yi M, Nie Y, Zhang C, Shen B. Application of Mesoporous Silica Nanoparticle-Chitosan-Loaded BMP-2 in the Repair of Bone Defect in Chronic Osteomyelitis. J Immunol Res. 2022; 2022: 4450196.
- Metsemakers WJ, Kuehl R, Moriarty TF, Richards RG, Verhofstad MHJ, Borens O, et al. Infection after fracture fixation: Current surgical and microbiological concepts. Injury. 2018; 49: 511-522.
- Piccato A, Crosio A, Antonini A, Battiston B, Titolo P, Tos P, et al. Single-stage versus two-stage bone flap reconstruction in chronic osteomyelitis: Multicenter outcomes comparison. Microsurgery. 2024; 44: e31139.
- Bible JE, Mir HR. External Fixation: Principles and Applications. J Am Acad Orthop Surg. 2015; 23: 683-690.
- Gao Q, Liu Q, Zhang G, Lu Y , Li Y, Tang M, et al. Identification of pathogen composition in a Chinese population with iatrogenic and native vertebral osteomyelitis by using mNGS. Ann Med. 2024; 56: 2337738.
- Xu L, Song H, Ren Y, Fang J, Zhou C, Zhang H, et al. Antibiotic- Impregnated Calcium Sulfate vs. Wound Irrigation-Suction to Treat Chronic Calcaneal Osteomyelitis. Foot Ankle Int. 2022; 43: 331-342.
- Shi X, Wu Y, Ni H, Li M, Zhang C, Qi B, et al. Antibiotic-loaded calcium sulfate in clinical treatment of chronic osteomyelitis: a systematic review and meta-analysis. J Orthop Surg Res. 2022; 17: 104.
- Selvaratnam V, Roche A, Narayan B, Giotakis N, Mukhopadhaya S, Aniq H, et al. Effectiveness of an Antibiotic-impregnated Bioabsorbable Carrier for the Treatment of Chronic Intramedullary and Diffuse Osteomyelitis. Strategies Trauma Limb Reconstr. 2023; 18: 148-154.
- Zhou R, Huang K, Guo Q, Lin B, Ren H, Liu Y, et al. Comparative Study of Linezolid and Vancomycin Regimens in One-Stage Surgery for Treating Limb Traumatic Osteomyelitis Caused by Methicillin- Resistant Staphylococcus aureus. Pol J Microbiol. 2023; 72: 239-246.
- Sambri A, Cevolani L, Passarino V, Bortoli M, Parisi SC, Fiore M, et al. Mid-Term Results of Single-Stage Surgery for Patients with Chronic Osteomyelitis Using Antibiotic-Loaded Resorbable PerOssal Beads. Microorganisms. 2023; 11: 1623.
- Tang B, Zhu W. Progress in diagnosis and treatment of post-traumatic osteomyelitis. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2021; 46: 1290- 1297.