Neurofibromatosis with Atypical Phenotypic and Imaging Features
- 1. AIIMS, Raipur, Chhattisgarh, India
Citation
Singh P, Sharma R, Nehete L (2020) Neurofibromatosis with Atypical Phenotypic and Imaging Features. JSM Brain Sci 4(1): 1021.
CLINICAL IMAGE
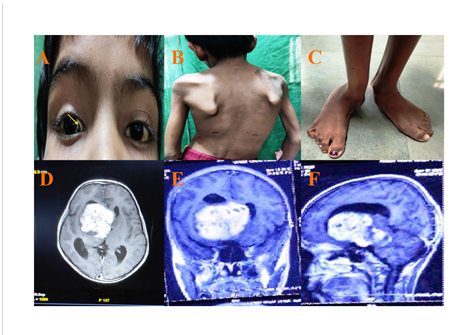
An 8-year-old boy presented with a history of progressive left hemiparesis for 3 weeks associated with mild headache but with normal vision and have no familial history of neurofibromatosis. Multiple cafe au lait spots were seen with a large patch over the left scapular region (Image 1, Panel B). He had scoliosis (Image 1, Panel B) and progressive bilateral foot deformity (Image 1, Panel C) since infancy. Ophthalmological evaluation revealed a blackish triangular patch in the medial aspect of the sclera (Image 1, Panel A), thus making it a unique finding in our case. On imaging, he was diagnosed with an atypical hypothalamic-optochiasmatic lesion (OPHG) (Figure 1, Panel D-F)
Figure 1: Image 1- Panel (A) -shows triangular patch in medial aspect of sclera suggestive of any atypical angiomatous lesion. Panel (B) - shows multiple café au lait spots with largest one over left scapular region. Panel (C) shows right ankle joint subluxation with equino-valgus deformity. Panel (D-F)- shows large suprasellar lesion, extending superiorly to shift the flood of the third ventricle with retrochiasmatic extension, causing midbrain compression and have T1 hypo, T2 and FLAIR hyperintense with homogenous contrast enhancement, suggestive of atypical hypothalamic optochiasmatic lesion. The optic nerve seems free in the imaging.
and was confirmed as low-grade glioma with an open biopsy, followed by chemotherapy. Based on the NIH criteria, he was diagnosed with neurofibromatosis-1. Skeletal abnormalities and long done dysplasia (especially tibia) is very common but foot deformity is very rarely reported in the literature [1]. The hypothesis behind the skeletal deformities suggests neurofibromin insufficiency causes premature apoptosis of the osteoblasts and changes in the osteoprogenitors cells differentiation [2]. OPHG lesion usually presents with visual deficits and behavioral changes which was not case in our patients as main bulk of the tumor is in the hypothalamus, which was unique in our case. Recent recommendations for the OPHG include ophthalmological and MRI studies four times a year for the first year, which is followed by gradual lengthening of test intervals over the next 2-3 years [3]. A two-line decrease in visual acuity on snellen chart needs referral to a pediatric neuro-oncologist for management. At present, there is very less role of the surgery and recommendation is for the chemotherapy, based on vincristine and carboplatin. Adjuvant radiotherapy is not recommended in NF-1 cases because of risk of secondary malignancies. An annual ophthalmological and spinal examination should be done below the age of 13 years in neurofibromatosis patients [2,3].
REFERENCES
- Savar A, Cestari DM. Neurofibromatosis Type I: Genetics and Clinical Manifestations. Seminars in Ophthalmology. 2008; 23: 45-51.
- Corsello G, Antona V, Serra G, Zara F, Giambrone C, Lagalla L. Clinical and molecular characterization of 112 single-center patients with Neurofibromatosis type 1. Ital J Pediatr. 2018; 44: 45.
- Hirbe AC, Gutmann DH. Neurofibromatosis type 1: a multidisciplinary approach to care. The Lancet Neurology. 2014; 13: 834-843.