Chagas Cardiac Disease, a Disease that must be kept in Mind
- 1. Department of Internal Medicine, Hospital São Francisco Xavier, Portugal
- 2. Department of Intensive Care Unit, Hospital Beatriz Angelo, Portugal
- 3. Department of Intensive Care Unit, Hospital da Luz, Portugal
- 4. Cardiology Department, Hospital da Luz, Portugal
Abstract
A 34-year-old woman, from Argentina, with history of positive serology for Trypanosoma cruzi (T. cruzi) is referred to cardiology consultation for symptoms of palpitations. Cardiovascular assessment with chest x-ray, electrocardiogram (ECG) and 24-hour Holter monitoring was normal. Attending to theepidemiologic context of an immigrant patient from an endemic area for Chagas’ disease echocardiographic evaluation was performed and documented left ventricle cavity at the upper limit for normal and inferolateral hypokinesia with decreased regional longitudinal strain. Cardiac magnetic resonance imaging
(MRI) detected dilated left ventricle (LV) with segmental alterations (lower wall and apex), dilated right ventricle (RV) and increased T1 and T2 native left ventricle. These findings were suggestive of chronic Chagas’ myocardiopathy, an early form (indeterminate phase).
New imagining modalities, like strain echochardiography and MRI, helped this patient to start pharmacological treatment earlier and is now a good way to improve clinical care and follow-up of a “forgotten disease”.
Keywords
Chagas Disease; Chagas’ myocardiopathy; Cardiac magnetic resonance imaging; Echocardiographic strain imaging
Citation
Verdasca I, Ferreira M, Mota P, Cardim N (2020) Chagas Cardiac Disease, a Disease that must be kept in Mind. JSM Clin Case Rep 8(1): 1172.
ABBREVIATIONS
ECG: Electrocardiogram; MRI: Magnetic Resonance Imaging; LV: Left Ventricle; RV: Right Ventricle
INTRODUCTION
Chagas’ disease, resulting from infection by the protozoan T. cruzi, is an important cause of heart failure [1,2]. It is a heterogeneous condition with a wide variation in prognosis and in its clinical course through acute and chronic phases.
Assessment of cardiac disease in patients with confirmed infection by Trypanosoma cruzi is crucial to detect early cardiac impairment and risk stratification before symptoms develop[2].
Characterization of the indeterminate phase has been challenging and it is imperfect because early manifestations can be subtle, however new technology, such as Strain Echocardiography and MRI, have been proved, to help the clinician make a more efficient and accurate diagnosis and understand when to start treatment in the early stages of the disease.
CASE PRESENTATION
A 34-year-old woman, from Argentina, living in Portugal for nine years, with history of positive serology for T. cruzi, acquired by congenital transmission, is referred to cardiology consultation for symptoms of palpitations felt as tachycardia for two weeks. There was no history of dyspnea, orthopnea, chest pain, fever or other symptoms. Family and social history was irrelevant besides Chagas’ disease. On exam her blood pressure was 120/75mmHg, pulse was 62 beats/min and regular. Her oxygen saturation by pulse oximetry was 97% on room air. No jugular venous distension was observed and the breathing sounds were normal. The cardiac examination revealed rhythmic sounds S1, S2 without additional heart sounds or heart murmur. Soft abdomen insensitive to palpation. No pitting edema was observed, with warm skin with good pulse. The weight was 80kg with a body mass index of 30.9 Kg/m?.
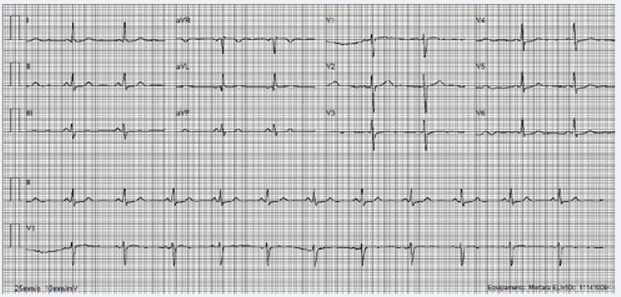
Laboratory evaluation confirmed positive serology for Chagas’ disease by IgG test for T. cruzi; the remaining laboratory evaluation as cardiac markers, thyroid function, inflammatory parameters were normal. Initial cardiovascular assessment was normal- electrocardiogram (Figure 1), 24-hour Holter monitoring and cardiac event recorder showed no arrhythmia or no relationship between symptoms and changes in heart rate or rhythm.
Figure 1 Electrocardiogram. Sinus rhythm, 73 bpm, non-specific ST-T wave changes.
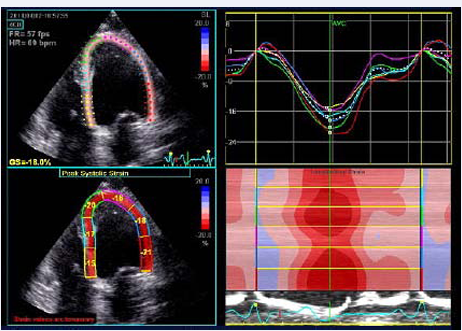
Chest-x ray showed no abnormalities. Further cardiovascular assessment by transthoracic echocardiogram (Figure 2) documented left ventricle cavity at the upper limit of normal with non-hypertrophied walls, with normal ejection fraction and global longitudinal strain, but with inferolateral hypokinesia and decreased regional longitudinal strain in this wall (Figure 3).
Figure 2 Transthoracic echocardiogram. Left ventricle cavity at the upper limit of normal with non-hypertrophied walls (Images acquired in GE ViVid E90).
Figure 3 Strain and Speckle-Tracking Echocardiography (TT). Normal global longitudinal strain but inferolateral hypokinesia and decreased regional longitudinal strain in this wall (Images acquired in GE ViVid E90).
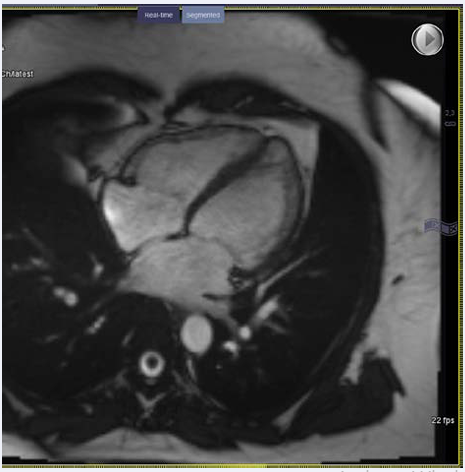
Although only minor changes were detected first, attending to the strong epidemiologic context of a Latin American immigrant from an endemic area for Chagas’ disease, further assessment was necessary for an accurate evaluation of myocardial involvement. Cardiac MRI detected dilated left ventricle with segmental alterations (lower wall and apex) with preserved global systolic function; dilated right ventricle without evident changes in regional kinetics and increased T1 and T2 native left ventricle, although there was no late enhancement (possible fibrosis and diffuse inflammation) – (Figure 4).
Figure 4 Cardiac magnetic resonance imaging (MRI). Dilated left ventricle with segmental alterations (lower wall and apex) with preserved global systolic function and dilated right ventricle without evident changes in regional kinetics and increased T1 and T2 native left ventricle.
These findings were suggestive of chronic Chagas’ myocardiopathy, an early form (indeterminate phase).
Diagnosis during the chronic phase of infection relies on serologic assays. Patients with chronic disease but without signs or symptoms of Chagas’ disease are considered to have the indeterminate phase of the infection. It is estimated that 20 to 30% of people who initially have the indeterminate phase of Chagas’ disease have progression over a period of years or decades to clinically evident cardiac disease, gastrointestinal disease, or both[1].
DISCUSSION
The term Chagas’ disease is used for the general disease caused by T. cruzi, a protozoan parasite. Chagas’ disease is a significant public health problem in most Latin American countries. In recent decades it has spread to cities and to no endemic countries, mostly as a result of immigration and travellers. The disease is a heterogeneous condition with a wide variation in clinical course and prognosis. Its natural history is generally divided into acute and chronic phases. In the chronic phase, two well-defined forms of disease are distinguished: indeterminate (latent, pre-clinical) and cardiac, digestive and cardio digestive forms [1]. Although the majorities (60%–70%) of infected individuals remain asymptomatic throughout life, some develop only conduction defects and mild segmental wall motion abnormalities; others develop severe symptoms of heart failure, thromboembolic phenomena, and life-threatening ventricular arrhythmias [2]. To note, sudden cardiac death is frequent and manifests often in the absence of previous significant symptoms or signs of advanced chronic Chagas’ cardiomyopathy [3]. The pathophysiology of myocardial damage in chronic Chagas is complex and multifactorial, but it has always three pathologic processes: inflammation, cell death and fibrosis.
Our case regards to a subtle clinical presentation of a young woman, natural from Argentina, with history of congenital transmitted Chagas’ disease who begun with symptoms of palpitations but without other symptoms or signs of disease at physical examination. The investigation was carried out by complementary tests with positive abnormal findings on serologic tests, echocardiography and cardiac MRI suggestive of indeterminate phase of Chagas’ disease.
The indeterminate phase of the disease is classically defined as the clinical situation of an individual with parasitological and/ or serological evidence of chronic T. cruzi infection, but without symptoms or physical signs of the disease, with normal ECG and chest X-ray and without digestive tract (esophagus and colon) impairment seen in radiological exams [3]. However, more accurate complementary exams (as echocardiography, nuclear angiocardiography, hemodynamic study) may demonstrate - usually subtle and of no prognostic relevance - cardiac alterations in this group of patients classified as indeterminate by classical criteria [2,4,5] .
Until new data there is no evidence to support formal guidelines in relation to the conduction of exams for early detection of left ventricular dysfunction in patients with the indeterminate phase of Chagas’ disease [3-5]. On the other hand, there are no identifiable factors in this phase that can distinguish the individuals who will develop the clinical cardiopathy from those who will remain asymptomatic during their whole lives, just keeping the serological positivity. It is suggested that complementary exams as echocardiography, ECG and x-ray should be repeated every 3-5years [1]. Our patient besides initiating pharmacological treatment must continue follow-up complemented by cardiovascular assessment and monitoring
REFERENCES
1. Simões M, Romano M, Schmidt A, Macedo M, José Antonio M. Chagas Disease Cardiomyopathy. Int J Cardiovasc Sci. 2018; 31: 173-189.
3. Rassi A Jr, Rassi A, Marin-Neto JA. Chagas heart disease: pathophysiologic mechanisms, prognostic factors and risk stratification. Mem Inst Oswaldo Cruz. 2009; 104: 152-158.