Graveful Iatrogenic Tracheoesophageal Fistula Secondary to Stenting of Post Irradiated Esophageal Stricture: Case Report
- 1. Department of Otorhinolaryngology, Queen Elizabeth Hospital, Malaysia
Abstract
Objective: We report an extremely rare case of massive tracheosophageal fistula which can be a reference for physicians and surgeons in the prevention of the disease.
Method: A case report and literature review of aetiologies, clinical features, management and prevention of acquired Tracheoesophageal Fistula (TOF) secondary to oesophageal stent are presented.
Results: A young gentleman developed TOF at post oesophageal stenting day 14 for benign proximal oesophageal stricture (secondary to irradiation for Diffuse Large B cell lymphoma of mediatinum). After insertion of self-expanding oesophageal stenting, he developed severe respiratory distress and stridor where he needed a tracheostomy. Presence of tracheostomy, oesophageal stent, previous irradiation and malnutrition put him at deem high risk of TOF. He passed away due to failure of pulmonary oxygenation before surgical correction of the fistula.
Conclusion: Proper selection of candidate with least risk factors is important prior oesophageal stenting.
Keywords
Tracheoesophageal fistula; Oesophageal stent; Irradiation
Citation
Liew YT, Yong DJ, Somasundran M, Ong CA (2014) Graveful Iatrogenic Tracheoesophageal Fistula Secondary to Stenting of Post Irradiated Esophageal Stricture: Case Report. JSM Clin Case Rep 3(1): 1074.
INTRODUCTION
Tracheoesophageal Fistula (TOF) is defined as abnormal connection between esophagus and trachea. It is a life threatening surgical emergency which warrants urgent attention and treatment as the patent tract bypasses the normal protection offered by laryngeal reflexes. Pulmonary complications such as aspiration pneumonia, pneumonitis can follow. We report a case of massive acquired TOF secondary to esophageal stenting for a benign proximal esophageal stricture.
CASE PRESENTATION
A 34 year old gentleman was diagnosed to have benign proximal esophageal stricture when he presented to medical unit, with the complaint of progressive dysphagia for 5 years. Besides, he suffered hypothyroidism, anemia and cervical myelopathy as a result of radiation therapy which he received for his Diffuse Large B cell lymphoma of mediastinum 20 years ago. Total dose of 30 Gy was given. There was no previous barium swallow and stenting done before. Clinically, the patient had cervical myelopathy at the level of T4. Her upper limb was normal neurologically. Level below T4 was affected. Regarding the esophageal stricture, it was about 4 cm in length from 18cm to 22 cm from upper incisor teeth (Figure 1).
Figure 1 Oesophageal stricture pre stenting (Fluoroscopy view).
Esophageal biopsy revealed no malignancy. Following that, primary medical team inserted a self-expanding fully covered metallic stent (Hanaro 110 mm length; 20 mm central diameter) endoscopically to relieve the obstruction (Figure 2).
Figure 2 Oesophageal stricture post stenting (Fluroscopy view).
Esophageal mucosa at the site of stenting was normal except for stenosed lumen. Six hours after the stenting, he developed respiratory distress. On examination, he was malnourished. He was fully conscious but severely tachypnoeic with biphasic stridor. Besides tachycardia, blood pressure was normal and oxygen saturation was still maintained within normal range by oxygen face mask. Arterial
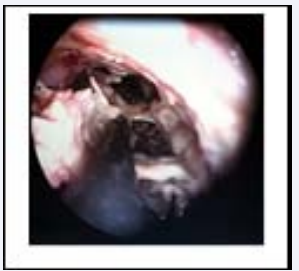
blood gas showed type 1 respiratory failure while chest X ray revealed pulmonary infiltrates at both lower lung fields. Bedside flexible nasopharyngolaryngoscopy showed normal glottic and supraglottic structures without obstructing mass. Stridor did not respond to both nebulized and intravenous steroid. He was then subjected to emergency tracheostomy in view of airway obstruction and urgent Computerized Tomography (CT) of neck and thorax showed subglottic and tracheal narrowing. Inflamed tracheal mucosa from tip of tracheostomy down to carina was noted from bronchotelescopy done at same setting. There was compression on the posterior tracheal wall as well, likely from the esophageal stent. No fistula was seen. Since then, he was mechanically ventilated for 2 days with portex tracheostomy tube in intensive care unit prior to extubation. Ballon pressure was frequently checked to ensure it was about 20mmHg. He had periodic hypotension due to sepsis but later improved with intravenous antibiotics and tracheostomy was decannulated. However, the decannulation could not last for more than a day till he developed another episode of respiratory distress with symptoms of cough during meals, and abdominal distention at day 14 post esophageal stenting. There was also leaking of fluid via tracheostoma whenever he drank. Repeated bronchotelescopy showed a massive TOF, starting 6 cm from vocal cords to the carina with esophageal stent migrated into trachea (Figure 3).
Figure 3 Bronchotelescopy view shows thick arrow as bronchus and thin arrow as oesophageal stent.
He passed away due to failure of pulmonary oxygenation before fistula could be treated effectively.
DISCUSSION
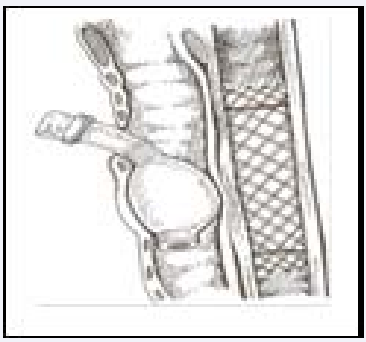
Acquired TOF is rare but serious complication of mainly malignancy and trauma. Nowadays, malignancy comprises about 50% of cases of acquired TOF whereas more than 75% of nonmalignant TOFs are due to endotracheal cuff related trauma. Of the malignant TOF, 77% are attributable to esophageal tumours while 16% are secondary to pulmonary primaries [1]. Other aetiologies include thoracic trauma, granulomatous inflammation such as tuberculosis, foreign bodies, radiotherapy, caustic ingestion, indwelling esophageal stent [1,2]. In our report, our patient was at deem high risk for developing TOF in view of his medical problems (anemia, hypothyroidism, malnutrition) and stents in situ both tracheostomy and esophageal stent. Both stents exerted pressure to the posterior wall of trachea and adjacent oesophageal wall. Pressure necrosis occurred due to local ischemia and TOF formed as showed in figure 4.
Figure 4 Cartoon diagram, arrow shows area of most compression pressure.
Other coexisting factors that could contribute to TOF formation in our patient were episodic hypotension, anemia, steroid usage which were suggested by Raman Diddee [1]. It is also worth to mention that out patient had received external beam radiotherapy for his cervical lymphoma. Radiation is known to create a hypovascular, hypoperfusion state with poor healing capacity in tissues. Stents in situ as mentioned might have added pressure on the esophagus which might have been irradiated.
Diagnosis of TOF basically based on clinical signs and symptoms, imaging studies and endoscopy. Three main signs and symptoms had been described, which are cough while taking meals, recurrent pneumonia or respiratory infection and periodic abdominal distention. Cough while taking meals is also known as Ono’s signs or swallow-cough complex [3]. For ventilated patients, signs suggestive of TOF are air leaking, failure of weaning, sudden bout of increased secretions and recurrent chest infections. As for imaging studies, barium swallow is able to detect 70% of the lesion as well [1]. CT scan is increasingly used since it helps evaluate luminal and extraluminal condition such as lymph node status, or mediastinal masses [4]. Anyhow, endoscopy (bronchoscopy and oesophagoscopy) still remains the best diagnostic method. Treatment is always challenging for both anaesthetists and surgeons. Various treatment methods have been performed such as esophageal stenting [5], endoscopic fibrin glue application [6], and open surgery [7]. As for massive TOF, open surgery is unavoidable. Benign TOFs are managed individually depending on cause, size, and location [7]. Commonly used approaches are cervical and transthoracic. A muscle flap from neck or intercostals is used to buttress the closure and to increase the success. Massive TOF may require tracheal resection [1].
CONCLUSION
Oesophageal stenting carries risk of TOF. It is even higher with counter pressure from tracheostomy. Factor such as irradiation further exacerbates the risk. Proper selection of candidate with least risk factors is important prior oesophageal stenting.
ACKNOWLEDGEMENT
The authors are thankful to Dr. Ahmad Fadhli, an medical colleague for helping in creation of the cartoon diagram of the sandwich effect between tracheostomy tube balloon cuff and the tracheoesophageal wall. This research received no specific grant from any funding agency, commercial or not-for-profit sectors.