Mixed Medullary-Papillary Carcinoma of the Thyroid
- 1. Department of Pathology, American University of the Caribbean, USA
Abstract
Collision tumor consisting of medullary thyroid carcinoma and papillary thyroid carcinoma is an extremely rare occurrence 3. We report a case of an 89 year old female diagnosed with uncommon collision tumor of the thyroid based on cytological evaluation of a fine needle aspiration specimen.
Keywords
Immunohistochemistry, Thyroid, Carcinoma; Mixed medullary-papillary
Citation
Fonseca C, Mohamad A (2018) Mixed Medullary-Papillary Carcinoma of the Thyroid. JSM Clin Case Rep 6(1): 1143.
ABBREVIATION
PTC: Papillary Thyroid Carcinoma; FTC: Follicular Thyroid Carcinoma; ATC: Anaplastic Thyroid Carcinoma; MTC: Medullary Thyroid Carcinoma; MMPC: Mixed Medullary-Papillary Thyroid Carcinoma
INTRODUCTION
Over the last ten years, we have seen an increase in the rate of thyroid cancer by approximately 3.8% [1]. Most thyroid cancers originate from follicular cells and are classified as papillary thyroid carcinoma (PTC), follicular thyroid carcinoma (FTC) and anaplastic thyroid carcinoma (ATC). Only medullary thyroid carcinoma (MTC) arises from parafollicular cells [2].
Thyroid cancers are usually differentiated histologically and with the aid of immunohistochemistry. Approximately 80% of diagnosed thyroid carcinomas are PTCs, and only 5-10% is MTCs. PTCs produce thyroid hormones and thyroglobulin. Patients diagnosed with this cancer have excellent long term prognosis. MTCs produce calcitonin and other peptide products, and this is a more aggressive type of thyroid cancer, it is associated with higher rates of relapse and mortality [2,3].
Presentation of mixed medullary and papillary carcinoma is rare (<1%), and very few cases have been reported in the literature [4,2,3,5]. After conducting a review of the English medical literature, we found that 34 cases have been published. Most cases were female patients, and the ages ranged from 27 to 84 [5]. Mixed medullary-papillary thyroid carcinoma (MMPC) is a variant of MTC. The World Health organization (WHO) describes it as a tumor presenting morphological characteristics of medullary carcinoma with immunoreactivity for calcitonin in addition to presenting follicular or papillary carcinoma with immunoreactivity for thyroglobulin. Among MMPCs, mixed medullary and follicular is more prevalent than mixed medullary and papillary [6,7].
Although the pathogenesis of this mixed tumor is not known, many hypotheses have been proposed [3]. Some believe that the cancerous cells have one common progenitor cell while others believe that this mixed cancer is a result of simultaneous changes in follicular and parafollicular cells [8]. Regardless of the pathogenesis, physicians need to be aware of the potential coexistence since an accurate diagnosis of mixed thyroid carcinoma is important for prognosis, appropriate treatment and screening [8,3]
CASE PRESENTATION
We report a case of an 89 year old female with diagnosis of MMPC based on cytological evaluation of a fine needle aspiration specimen. The tumor cells of this rare carcinoma display morphological and immunological characteristics of medullary and papillary carcinoma within a single lesion.
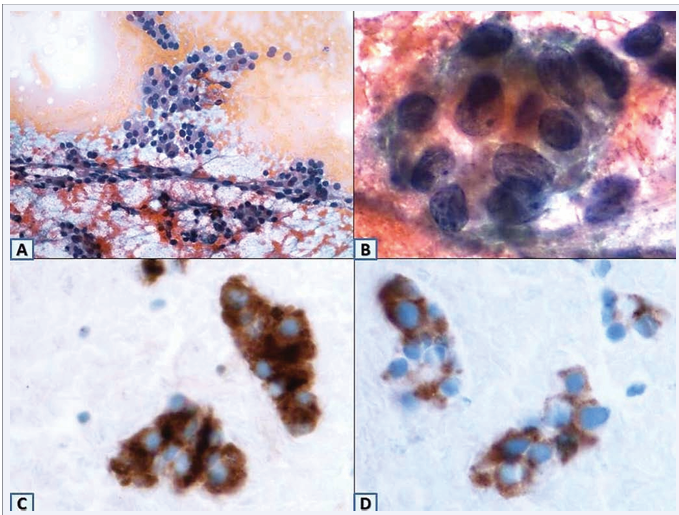
The patient presented with a 2.7 cm suspicious thyroid nodule. Fine needle aspiration of a nodule of the thyroid showed mixed features of medullary carcinoma (Figure A) as well as few nuclear features of papillary carcinoma (Figure B).
Figure 1 Fine needle aspiration of the 2.7 cm suspicious thyroid nodule showing mixed features of medullary carcinoma (Figure, A) as well as few nuclear features of papillary carcinoma (Figure, B). After total thyroidectomy, histopathological analysis of the surgical specimen revealed a carcinoma with histomorphologic features of both MC and PC. Immunohistochemistry studies were confirmatory with positivity for thyroglobulin (Figure, C) and calcitonin (Figure, D).
Considering these findings, the patient underwent a total thyroidectomy. Histopathological analysis of the surgical specimen revealed a carcinoma with histomorphologic features of both MTC and PTC. Immunohistochemistry studies were confirmatory with positivity for thyroglobulin (Figure C) and calcitonin (Figure D).
DISCUSSION
The case presented here highlights the importance of awareness of MMPC and the importance of utilizing immunohistochemical markers to make correct diagnoses of thyroid carcinomas. MMPCs are rare variants of MTCs, but this simple technique can help physicians rule out similar tumors. By obtaining differential diagnosis with immunohistochemistry, patients will get a more accurate prognosis [6].
According to WHO, prognosis of MMPC (follicular or papillary) depends upon the medullary component [7]. The presence of MTC worsens the prognosis when compared to PTC alone. The cellular origin of MMPC has not been established. The simultaneous existence of MTC and PTC has been shown to occur as a mixed tumor presenting dual differentiation and as a collision tumor, where the same mass has separate and different components [2]. The case being reported here exemplifies a collision tumor of the thyroid. Similar cases have been presented by Gajare and Joshi [2], Albores-Saavedra et al.[9], Narayanankutty and Devadas [3], Rossi et al. [10], and Gero et al. [11].
Based on available data, MMPCs seem to occur more often in women over the age of fifty and are presented as palpable neck swellings. Most cases were treated surgically. Of interest, review of the literature suggests that the incidence of hypothyroidism following total thyroidectomy is higher than following hemi thyroidectomy. In addition, morbidity rate is lower with hemi thyroidectomy [12]. Metastasis was detected in few patients, including metastasis to lung, liver, mediastinum or bone [2,3]. An accurate diagnosis of these uncommon mixed thyroid carcinomas is essential for optimal treatment and genetic screening in order to exclude familial medullary thyroid carcinoma (FMTC) and Multiple Endocrine Neoplasia 2 (MEN2) syndrome [2]. In order to increase accuracy of diagnosis and prognosis, immunohistochemical markers should be utilized when identifying thyroid cancer.