Non-Compaction of the Left Ventricle with Multiple Left Intraventricular Thrombi Complicated By Left Hemispheric Ischemic Stroke: A Case Report
- 1. Department of Cardiology, Bogodogo University Hospital, Burkina Faso
- 2. Department of Cardiology, Yalgado OUEDRAOGO University Hospital, Burkina Faso
Abstract
Introduction: Non-compaction of the left ventricle (NCVG) is an under-diagnosed cardiac pathology with major complications. We describe a case of LVNC complicated by intraventricular thrombi followed by hemispheric ischaemic stroke.
Clinical presentation: The patient was 24 years old, primigravida and primiparous, with no previous pathological history, and was admitted for dyspnoea. Physical examination revealed general condition stage III (WHO performance status), paleness of conjunctivae and mucous membranes, blood pressure 130/88 mmHg, congestive heart failure syndrome, mitral insufficiency murmur intensity 3/6. Echocardiography showed hypertrabeculation inside the left ventricle, which was very vascular on colour Doppler, with three trombi in the left ventricle. The patient was treated with furosemide 80 mg daily, enalapril, Aldactone for heart failure and curative enoxaparin. The 48-hour course was marked by the sudden onset of total right hemiplegia with Brocca aphasia. A subsequent CT scan revealed a left hemispheric ischaemic stroke. The patient died 24 hours after her neurological event due to respiratory distress.
Conclusion: This case highlights the diagnostic and therapeutic issues associated with non-compaction cardiomyopathy. It is a condition that is still poorly understood, with a high risk of complications.
KEYWORDS
- Non-compaction
- Left ventricle
- Thrombi
- Vascular accident
CITATION
NACANABO MW, SEGHDA AT, SAWADOGO LF, TALL/THIAM A, YAMEOGO VN,et al (2025) Non-Compaction of the Left Ventricle with Multiple Left Intraventricular Thrombi Complicated By Left Hemispheric Ischemic Stroke: A Case Report. JSM Clin Case Rep 13(1): 1254.
INTRODUCTION
Non-compaction of the left ventricle (NCVG) is a rare and often under-diagnosed cardiopathy, which forms part of the primary cardiopathies [1]. Although its exact prevalence remains difficult to establish, LVNC is becoming increasingly recognised, particularly with advances in cardiac imaging techniques [2]. It is characterised by abnormal myocardial architecture, with abnormally deep trabeculations and intramural sinuses [3]. This embryological abnormality in cardiac development leads to systolic dysfunction, which can be complicated by a variety of clinical manifestations, including arrhythmias, heart failure and, in some cases, stroke [4]. This type of stroke is a direct consequence of thrombus formation in an uncompacted left ventricle, where inefficient blood flow can lead to the formation of clots, which can break loose and migrate to the cerebral circulation, clogging arteries and inducing ischaemic stroke [5]. Our case illustrates this association in a patient with LVNC with multiple intraventricular thrombi, who developed a total left hemispheric ischaemic stroke.
CLINICAL OBSERVATION
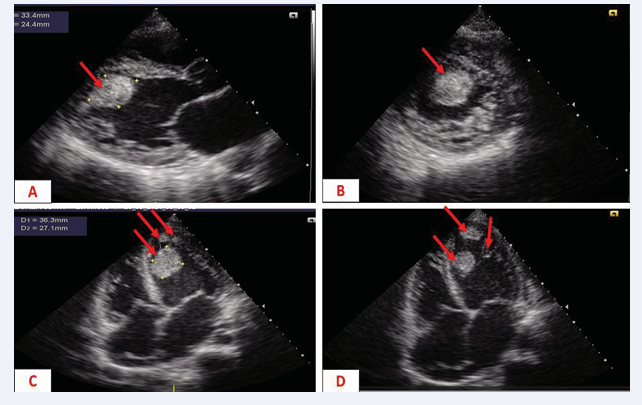
The patient was 24 years old, primigravida, primiparous, with no previous pathological history, and was referred for New York Health Association stage IV dyspnoea. This dyspnoea began one week after vaginal delivery, followed by a progressive worsening, becoming orthopnoic, associated with moderate precordialgia and oedema of the lower limbs. On physical examination, the patient’s general condition was stage III (WHO performance status), her conjunctivae and mucous membranes were pale, her blood pressure was 130/88 mmHg, she had congestive heart failure, and she had a 3/6 murmur of mitral insufficiency. This clinical picture led to the suspicion of peripartum cardiomyopathy, valvularheartdiseaseoradecompensated anaemic heart. The electrocardiogram showed regular sinus tachycardia. Doppler echocardiography showed dilatation of the left ventricle (diastolic diameter 57 mm), an altered left ventricular ejection fraction of 35%, and hypertrabeculation inside the left ventricle, which was very vascular on colour Doppler, with three trombi in the left ventricle (Figure 1).
Figure 1: Doppler echocardiogram showing
A: para-sternal long-axis section, large intra-VG thrombus (red arrow)
B: trans-ventricular short-axis paraspinal slice, large intra-GV thrombus (red arrow)
C and D: apical 4-cavity slice, three intra-VG thrombi (red arrow)
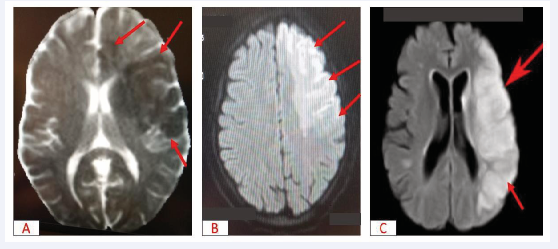
The initial diagnosis of non- compaction of the left ventricle complicated by intra- VG thrombi was accepted. The patient was treated with furosemide 80 mg daily, enalapril, spironolactone and enoxaparin in curative doses. The immediate course was marked at 48 hours by the sudden onset of massive left hemiplegia associated with Broca’s aphasia and respiratory distress. Magnetic resonance imaging of the brain revealed diffuse cortico-subcortical hypersignal areas in the left frontal, left parieto-temporo-occipital and left caudo-capsulo-lenticular regions, suggesting a recent left hemispheric ischaemic stroke (Figure 2).
Figure 2: Brain MRI showing
A: Left fronto-temporal-parietal hyposignal suggestive of recent constituted ischaemia, T1 sequence (red arrow)
B: Left fronto-temporal-parietal hypersignal suggestive of recent constituted ischaemia, diffusion sequence (red arrow)
C: Left fronto-temporal-parietal hypersignal suggestive of recent constituted ischaemia, sequence, 3DTOF, transventricular slice (red arrow)
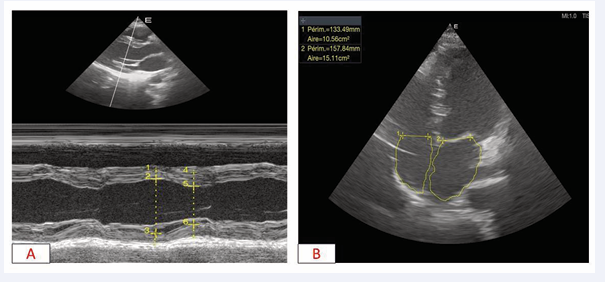
A follow-up echocardiogram showed a thrombus-free left ventricular cavity (Figure 3).
Figure 3: Transthoacic Doppler echocardiography
A: long-axis para-sternal slice, absence of intraventricular thrombi B: apical 4-cavity slice, absence of intraventricular thrombi
The patient died 24 hours later from respiratory distress.
DISCUSSION
NCVG is often diagnosed in young adults, with a slight male predominance [3]. Epidemiological studies report an estimated prevalence of between 0.014% and 0.05% in the general population [6]. Although rare, the association between HNV and thromboembolic events, particularly stroke, is well documented [7]. Intraventricular thrombus formation is more common in complicated forms of LVNC, due to systolic failure and blood stasis resulting from the abnormal morphology of the left ventricle.
The symptoms of LVNC vary considerably from patient to patient. Some patients may be asymptomatic, while others show signs of left ventricular dysfunction, ventricular tachycardia or heart failure [1,6]. In complex forms, such as the one presented here, intraventricular thrombus formation leads to blood stasis and an increased risk of thromboembolism [5]. Patients may show signs of stroke, such as motor impairment or cognitive problems [5]. Total hemispheric stroke, as in our case, is a serious and often fatal complication.
Diagnosis of LVNC is based on cardiac imaging techniques, in particular echocardiography, which can visualise the abnormal trabeculations of the left ventricle and the intramural sinuses [8]. Cardiac MRI remains the gold standard for assessing non-compaction and the degree of cardiac dysfunction, although it was not performed in this patient [9]. Transoesophageal echocardiography may be useful for detecting intraventricular thrombi, which are common in LVNC due to blood stasis [1]. A cerebral CT scan or MRI is essential for diagnosing stroke, confirming the territory of arterial occlusion and the extent of cerebral lesions. These paraclinical examinations also make it possible to assess secondary complications of the disease, including cardiac and cerebral lesions.
The management of HNV is based on a multimodal and preventive approach. The main aim is to optimise cardiac function and prevent thromboembolic events [1]. Anticoagulant therapy is often indicated to prevent the formation of new thrombi in the left ventricle [10]. Drugs such as direct oral anticoagulants or warfarin are used to reduce the risk of stroke, although the choice of molecule depends on the patient’s clinical situation [10]. In some cases, implantation of a cardiac defibrillator (ICD) or pacemaker may be necessary to control cardiac arrhythmias [11]. Treatment of heart failure with beta- blockers, angiotensin-converting enzyme (ACE) inhibitors or diuretics is also essential [6]. Patients with total hemispheric stroke require urgent stroke treatment, including thrombolysis or thrombectomy,
The prognosis of LVNC depends on several factors, such as the severity of left ventricular dysfunction, the presence of cardiac arrhythmias and the degree of complications, particularly thromboembolic [11]. Patients with intraventricular thrombi and stroke generally have a poorer prognosis [12]. Neurological complications can have a major impact on a patient’s quality of life and life expectancy [4]. However, with early diagnosis and appropriate treatment, the prognosis can be improved, although the management of thromboembolic events remains a major challenge. The importance of regular monitoring and active management of cardiovascular risk factors is crucial in limiting long-term complications.
CONCLUSION
Non-compaction of the left ventricle is a complex condition requiring early and appropriate management. The case presented highlights the diagnostic and therapeutic challenges associated with non-compaction of the heart, a phenomenon that is still poorly understood, with complications that can significantly affect the patient’s quality of life. Treatment must be personalised, combining optimal management of heart failure, prevention of thrombus and treatment of stroke. Multidisciplinary management, combining advanced cardiac imaging and neurovascular monitoring, is essential to optimise the management of this complex condition.
Patient Consent
We have obtained the consent of the patient’s parents for the publication of these data.
REFERENCES
- Damas F, Ancion A, Tridetti J, Lancellotti P. Non-compaction ventriculaire gauche : diagnostic et prise en charge. Rev Med Liege. 2020; 75: 781-785.
- Maron BJ, Towbin JA, Thiene G, Antzelevitch C, Corrado D, Arnett D, et al. Contemporary definitions and classification of the cardiomyopathies : an American Heart Association Scientific Statement from the Council on Clinical Cardiology, Heart Failure and Transplantation Committee ; Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups ; and Council on Epidemiology and Prevention. Circulation. 2006; 113: 1807-1816.
- Fennira S, Tekaya MA, Kraiem S. La non-compaction du ventricule gauche : ce qu’il faut savoir ! Ann Cardiol Angéiologie. 2019; 68: 120- 124.
- Finsterer J, Stöllberger C. Impact de la non-compaction du ventricule gauche sur le cerveau. Neurol Neurochir Pol. 2023; 57: 320-321.
- Benyounes N, Obadia M, Gout O. Non compaction cardiomyopathy: Une cause rare d’infarctus cérébral chez un jeune adulte. Rev Neurol (Paris). 2011; 167: 356-357.
- Gaye ND, Ngaïdé AA, Bah MB, Babaka K, Mbaye A, Abdoul K. Non- compaction of left ventricular myocardium in sub-Saharan African adults. Heart Asia. British Med J Publishing Group. 2017; 9: e010884.
- Finsterer J, Stollberger C, Mölzer G, Winkler-Dworak M, Blazek G. Cerebrovascular events in left ventricular hypertrabeculation/ noncompaction with and without myopathy. Int J Cardiol. 2008; 130: 344-348.
- Habib G. Non-compaction du ventricule gauche. Apport de l’échocardiographie. In : Boyer L, Guéret P, éditeurs. Imagerie en coupes du cœur et des vaisseaux. Paris : Springer Paris. 2013; 107- 115.
- Thuny F, Jacquier A, Jop B, Giorgi R, Gaubert JY, Bartoli JM, et al. Assessment of left ventricular non-compaction in adults : Side- by-side comparison of cardiac magnetic resonance imaging with echocardiography. Arch Cardiovasc Dis. 2010; 103: 150-159.
- Arbelo E, Protonotarios A, Gimeno JR, Arbustini E, Barriales- Villa R, Basso C, et al. 2023 ESC Guidelines for the management of cardiomyopathies. Eur Heart J. 2023; 44: 3503-3626.
- Bai W, Xu R, Li X, Xu H, Fu H, Hou R, et al. Prognostic value of cardiac magnetic resonance imaging parameters in left ventricular noncompaction with left ventricular dysfunction. BMC Cardiovasc Disord. 2022; 22: 526.
- Stöllberger C, Blazek G, Dobias C, Hanafin A, Wegner C, Finsterer J. Frequency of Stroke and Embolism in Left Ventricular Hypertrabeculation/Noncompaction. Am J Cardiol. 2011; 108: 1021-1023.