Osteogenesis Imperfecta Type I and Diverticular Disease of the Colon -Do They Relate? : Report of a Case
- 1. 2nd Department of Surgery, Aristotle University of Thessaloniki, Greece
- 2. West Suffolk Hospital, UK
Abstract
Osteogenesis imperfecta is a heterogeneous group of genetic disorders that affect the integrity of the connective tissue. Manifestations of the disease include bone fragility, osteoporosis, dentigenesis imperfecta, blue sclera, easy bruising, joint deformity and scoliosis. On the other hand, colonic diverticular disease is the most common acquired disease of the large bowel in the western population. More recent studies propose that that multiple factors among which also genetic influences on extracellular matrix molecules, could play a role in the genesis of colonic diverticula.
We report the case of a 57 year old man with known Osteogenesis imperfecta type I disease who presented with acute lower left abdominal pain due to sigmoid diverticulitis. We present the hypothesis that these two entities (Osteogenesis Imperfecta and diverticulosis), as diseases attributed to weakening of the connective tissue, could have a common causative relation.
Keywords
Osteogenesis imperfect; Diverticular disease; Sigmoid diverticulitis
Citation
Papaziogas B, Doulias T, Tsiaousis P, Christopoulos P, Paraskevas G, et al. (2014) Osteogenesis Imperfecta Type I and Diverticular Disease of the Colon -Do They Relate? : Report of a Case. JSM Clin Case Rep 2(1): 1013.
INTRODUCTION
Osteogenesis imperfecta (OI) is a genetic disorder mainly characterized by the increased bone fragility [1]. Its incidence varies between 1:10.000 to 1:20.000 live births [2]. 90% of the patients show a mutation in COL1A1 or COL1A2, the genes encoding collagen type I, which is considered the major protein of bones, skin and tendons. Seven subgroups of OI patients have been described (type’s I-VII) [3].
Type I is the most common type and is characterized by blue sclera, absence of dentinogenesis imperfecta and minimal bony deformity. Type II is associated with increased perinatal lethality due to multiple rib fractures and pulmonary insufficiency. Type III presents the most severe form of OI in patients surviving the neonatal period. Over 50% of these patients become crippled at an early age. Respiratory insufficiency remains the main lethal complication. Type IV consists of a clinically diverse group, without the classical phenotypic expression type I or III [1]. The last three subtypes (V-VII) are characterized by absence of collagen mutation.
On the other hand, colonic diverticulosis is a disease of the Western world [4]. In these countries, over 90% of patients with diverticular disease present with left-sided diverticula [5]. Its incidence raises from about 5% in individuals under 40 years old, to 65% in those aged over 65 years [6]. Colonic diverticulosis is described as protrusion or herniation of the mucosal and sub mucosal layer through the circular muscle layer at the entering points of the wall vessels, which present weak points of the colonic wall. The pathogenesis of diverticular disease includes environmental, epidemiologic as well as genetic factors, leading to changes in mechanical and structural features of the colonic wall, elevated intraluminal pressure and functional “segmentation” [7]. Alterations in collagen, elastin and proteoglycans, either congenital or acquired, could lead to weakness of the bowel wall thus predisposing to the development of diverticula [6]. Furthermore, colonic diverticulosis is more prevalent in young patients with inherited connective tissue diseases [8,9]. This is the first description of a patient with known OI type I, who presented with acute diverticulitis.
CASE PRESENTATION
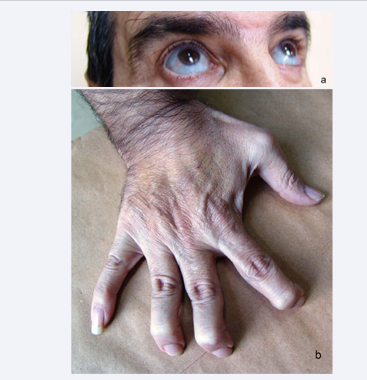
A 57-year old man was admitted to our department with acute left-sided lower abdominal pain, mild fever and leukocytosis. Anorexia and nausea neither were present, but no alteration in bowel habits nor were urinary symptoms noted. Abdominal findings included localized tenderness in the left iliac fossa, together with involuntary guarding. Decreased bowel sounds were noted. Digital rectal examination revealed a mild tenderness in the Douglas pouch. The patient had no history of previous surgery but was under medication (bisphosphonates) for known OI type I. Blue sclera, (Figure 1a), joint deformation and laxity (Figure 1b) and minimal bony deformity were present.
Figure 1 Patient’s clinical presentation with Osteogenesis Imperfecta type I, including blue sclera (Figure 1a) and hand joint laxity (Figure 1b).
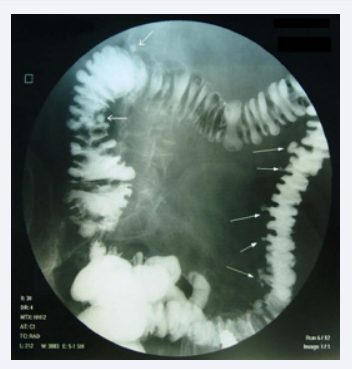
The patient reported several similar but milder episodes of left sided abdominal pain during the last 15 years. A CT-scan of the abdomen showed multiple sigmoid diverticula and a localized inflamed peri-colonic fat. The diagnosis of an uncomplicated diverticulitis was established and conservative treatment with IV antibiotics and food abstinence was initiated. After five days the patient was discharged and returned for a barium swallow a month later (Figure 2), which confirmed the diagnosis of leftsided diverticular disease, which extended through the whole length of the left colon reaching to the left colic flexure, as well as small solitary diverticula’s of the transverse colon and the ascending colon.
Figure 2 Barium enema examination of the colon. Diverticular disease of the descending and sigmoid colon, as well as solitary diverticula of the transverse colon and colon ascendens(white arrows).
DISCUSSION
Collagen comprises a structural protein found in all multicellular organisms, with almost 20 distinct types being described until now [2]. Type I collagen is the most common type of collagen comprising 95% of the entire bone collagen, and is found in all connective tissues except of hyaline cartilage [2].
Osteogenesis imperfecta (OI) is a genetic disorder mainly characterized by the increased bone fragility (1). 90% of the patients with OI show a mutation in COL1A1 or COL1A2, the genes encoding collagen type I [3]. Over 100 different mutations have been described in these genes [2]. The presence of abnormal collagen chains may have a strong influence on both the tensile strength of the collagen fibrils and also the metabolism of the
non-collagenous bone components [10,11,12]. . Type I of OI is classically related to reduced quantity of collagen type I due to a stop, frame shift or splice site mutation in COL1A1 or COL1A2. Since these mutation lead only to quantitative defect of collagen, the phenotype of this group is relatively mild [1]. Mutations in OI type II and type III patients usually involve glycine substitution in COL1A1 or COL1A2 genes leading to a qualitative defect in collagen type I. Thus, the phenotypic expression of these groups\ is much more severe than that of type I [1]. Our patient had known OI type I, which is in consistency with the relatively mild expression of the disease.
On the other hand, the mechanical properties of the colonic wall depend on the interaction of its anatomic components. The sub mucosa of the large bowel is composed almost exclusively of collagen fibrils, while collagen is also present in all the other layers of the colon [13]. These components of the colonic wall are known to deteriorate with advanced age as well as in diverticulosis. Thomson et al. [14] showed that collagen fibrils
of the left colon became smaller and more tightly packed than those in the right colon with advanced age. These alterations were also accentuated in diverticular disease. Watters et al. [15] and Whiteway et al. [16] reported an increase in the thickness of collagen and elastin fibrils in patients with diverticulosis coli. Wess et al. [13] investigated collagen solubility in relation with age and presence of diverticulosis. They proved that, although total collagen content remains unchanged, the collagen solubility index in the entire colonic wall significantly decreases after the age of 60 years as well as in the presence of diverticulosis, thus lowering the tensile strength and facilitating the formation of diverticula. Furthermore, Stumpf et al. [17] and Bode et al. [18] showed a significantly lower collagen I/III ratio in the diverticulitis group. Specifically, the amount of mature type I collagen was significantly lower in the diverticulitis group, while immature collagen type III (which has less mechanical strength than its mature counterpart) was higher than in healthy controls. Ye et al. [19] supported the role of connective tissue changes in diverticulosis of the colon, by referring to patients with inherited conditions such as Marfan and Ehlers–Danlos syndromes, which involve mutations in fibrillin and type III collagen genes, respectively. There are reported cases of early onset diverticulosis of the colon in these patients. Finally, “herniosis”, the probably hereditary systemic connective tissue disease, is thought to be the cause of the Saint’s triad (diverticulosis of the colon, hiatal hernia and cholelithiasis [20].
In view of the above mentioned we believe that these two conditions (osteogenesis imperfecta and diverticulosis) share a common causative pathway, namely the impaired collagen type I. Diverticulosis is more likely to present in patients with OI type I , since these patients are more likely to survive to adulthood, due to the milder presentation of the disease. Among these patients, the development of diverticulosis could be more prevalent, developing at a younger age than expected or extending more proximally than the sigmoid colon as in our case. It is noteworthy that our patient mentioned that he had similar clinical episodes over the last 15 years, which could be attributed
to repeated episodes of mild sigmoid diverticulitis. Furthermore, he presented on barium enema more proximal location of the diverticulosis extending through the whole length of the left colon until the left colonic flexure, as well as solitary diverticula of the transverse colon and ascending colon. These facts are in further support of our hypothesis.
In conclusion, although OI is an extremely rare disease, its possible correlation with other diseases attributed to weakness of the connective tissue, congenital or acquired, should be further investigated. The only way to verify our hypothesis would be to screen the patients with osteogenesis imperfecta for the presence of diverticular disease in younger age (eg. after 30 years of age) and compare the incidence of diverticular disease with the rest of the population.