Palliative Rehabilitation in Spinal Cord Injury: A Case Report
- 1. Rutgers New Jersey Medical School, Newark, USA
- 2. Cancer Rehabilitation Medicine, The Kessler Institute for Rehabilitation, USA
Abstract
Introduction: Patients diagnosed with cancer may experience a myriad of difficulties secondary to the malignancy itself and treatments received. Such patients may undergo intensive inpatient rehabilitation therapy to improve functionality and independence. In cases with unknown or poor prognoses, inpatient rehabilitation may serve as a beneficial intervention, enabling patients to remain at home for end-of-life care and potentially improving patient outcomes.
Case Presentation: The case presented here details the experience of a patient with progressive tetraplegia resulting from a cervical glioma. The patient presented with decreased ability to perform activities of daily living and underwent 29 days of inpatient rehabilitation, resulting in overall improved functioning and ability to remain safely at home.
Discussion: Inpatient rehabilitation for patients with progressive or terminal cancer may enable longer in-home residence and prevent or delay transfer to nursing facilities or hospice care. Increased functionality can decrease caregiver burden, mitigate complication rates, reduce healthcare costs, and improve morale. By applying cancer-specific performance scales to rehabilitation, practitioners can better assess and predict suitability for inpatient rehabilitation in this complex population.
Keywords
Palliative Rehabilitation, Cancer, Case Report
Citation
Birkenfeld B, Stubblefield MD (2022) Palliative Rehabilitation in Spinal Cord Injury: A Case Report. JSM Clin Case Rep 10(3): 1206
INTRODUCTION
Inpatient rehabilitation can be a valuable option for some individuals as it helps to restore independence, functionality, and quality of life following life-altering events. Common pathologies treated with an inpatient stay include spinal cord injuries, brain injuries, and cancer [1]. In order to qualify for inpatient rehabilitation, several criteria must be met. These include ongoing therapy via multiple disciplines (physical therapy, occupational therapy, speech-language pathology, or prosthetics/orthotics), the ability to participate in three hours of therapy daily for five days a week, supervision by a rehabilitation physician, and active participation in and anticipated improvement from the intensive inpatient rehabilitation program [2].
While patients with many conditions improve over time, especially with tailored inpatient rehabilitation therapy, patients diagnosed with progressive conditions, such as cancer, may experience progressive decline in overall function, regardless of treatment with chemotherapy, radiation, or other modalities [3]. Throughout their journey, patients may experience many challenges that can be addressed by inpatient rehabilitation including bowel and bladder management, ambulation, transferring, and self-care [4,5].
The need for inpatient cancer rehabilitation is warranted given that longevity and overall survival rates continue to increase. In the case report described below, we review a patient with spinal cord injury and deteriorating function from incurable cancer. Despite ongoing difficulties, this patient nonetheless benefitted from inpatient rehabilitation as determined by improvement in his Continuity Assessment Record and Evaluation (CARE) Item Set, a tool used to compare patient abilities upon admission and discharge [6]. His improvement illustrates the role rehabilitation can play in improving cancer patient outcomes and allow for the ability to safely stay home, even when facing progressive, terminal disease [5].
CASE PRESENTATION
A 57-year-old man presented for worsening bilateral upper extremity function and fatigue. His history includes C5 anterior cervical discectomy and fusion, hypertension, post-traumatic stress disorder, depression, and presumed multilevel cervical compressive myelopathy status post C3-C7 laminectomy and spinal fusion. Following the procedure, the patient experienced only minimal improvement in bilateral upper extremity function. Post-surgical MRI of the cervical spine demonstrated an edematous cervical cord with hyperintense T2 signal that was deemed to be unrelated to post-compressive myelopathy. He was diagnosed as C4 ASIA D (C7 motor/C4 sensory) as per the ASIA/ ISCoS International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) [7].
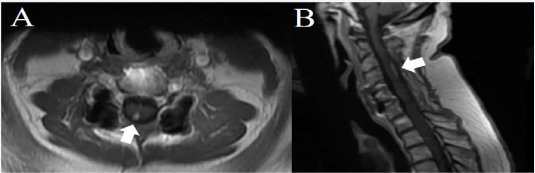
His failure to improve warranted repeat imaging, which demonstrated a spinal lesion suggestive of a neoplasm, most likely a low-grade glioma (Figure 1). The patient received proton beam radiotherapy with concurrent temozolomide and subsequent adjuvant temozolomide. Despite these interventions, the patient experienced continued progressive upper extremity weakness, loss of balance, and fatigue.
Figure 1: Axial (A) and Sagittal (B) T1 gadolinium enhanced MRI of the spine demonstrating glioma in the right paramedian dorsal aspect of the spinal cord at the level of C3-C5.
To improve the patient’s symptoms, outpatient physical therapy and occupational therapy as well as baclofen for spasticity were prescribed. During this time, repeat imaging demonstrated increased spinal cord edema and increased signal within the cord, consistent with disease progression. The patient continued to experience worsening weakness, most notably in the upper extremities, associated with fatigue and loss of balance. The patient was started on avastin and lomustine to slow tumor progression. Based on the rapid progression of disease and poor response to the antineoplastic therapy, it was clear that his cancer would continue to progress, causing complete tetraplegia and ultimately death.
Due to worsening cancer status and lack of improvement with outpatient rehabilitation, the patient was admitted for 29 days of inpatient rehabilitation for therapy with various modalities. The patient experienced marked improvement in functionality and independence across several domains as demonstrated by his scores on the CARE Item Set (Table 1). Most notably, the patient gained mobility while sitting in a wheelchair, self-dressing, and moving between positions in a bed or chair. Importantly, the patient did not perform worse on any task than he did upon arrival. In some instances, despite rehabilitation, the patient remained unable to perform certain tasks, such as walking or overcoming steps, given his lower extremity weakness and impaired balance. The patient neither improved nor worsened in some categories, including eating and oral hygiene tasks, which the patient had performed nearly independently at baseline.
| PT/OT Goals | CARE Score Upon Admission | CARE Score Upon Discharge |
| Car Transfer | 2 | 3 |
| Walk 10 Feet | 88 | 88 |
| Walk 50 Feet with Two Turns | 88 | 88 |
| Walk 150 Feet | 88 | 88 |
| Walking 10 Feet on Uneven Surfaces | 88 | 88 |
| 1 Step (curb) | 88 | 88 |
| 4 Steps | 88 | 88 |
| 12 Steps | 88 | 88 |
| Picking up Object | 88 | 88 |
| Wheel 50 Feet with Two Turns | 88 | 6 |
| Wheel 150 Feet | 88 | 6 |
| Eating | 5 | 5 |
| Oral Hygiene | 5 | 5 |
| Toileting Hygiene | 88 | 1 |
| Shower/Bathe Self | 88 | 88 |
| Upper Body Dressing | 9 | 5 |
| Lower Body Dressing | 9 | 1 |
| Putting On/Taking Off Footwear | 9 | 1 |
| Roll Left and Right | 2 | 3 |
| Sit to LyingLying to Sitting on Side of Bed | 2 | 3 |
| Sit to Stand | 2 |
3 |
| Chair/Bed-to-Chair Transfer | 2 | 3 |
| Toilet Transfer | 88 | 3 |
| Legends: 1-Dependent, 2-Substantial/maximal assistance, 3-Partial/ moderate assistance, 4-Supervision or touching assistance, 5-Setup or clean-up assistance, 6-Independent, 7-Patient Refused, 9-N/A, 88-Not attempted due to medical condition or safety concern | ||
DISCUSSION
Improved treatments and, in turn, increased rates of survivorship have contributed to an ever-increasing need for cancer rehabilitation [8]. While rehabilitation is generally recommended for individuals in the recovery phase of their journey, patients with limited life expectancy may also benefit from such comprehensive inpatient rehabilitation. Determining the appropriate length of stay for patients with terminal cancer is paramount for ensuring a successful course of rehabilitation [5]. For example, patients with shorter life expectancies (i.e., those who are within a few days or weeks of the end of their lives) are not likely to make significant functional gains due to progression of their cancer. Therefore, such patients may benefit from shorter stays focused on supporting the return home with hospice. On the other hand, patients with longer life expectancies (i.e., those who have months or years left in their lives) may benefit from longer stays. Longer stays may allow patients to effectively cope with anticipated declines while remaining in the home environment.
In the case described above, inpatient cancer rehabilitation therapy provided the opportunity for the patient to undergo extensive physical and occupational therapy with concurrent oncologic treatment in the context of impending complete tetraplegia and likely death. By participating in such care, the patient’s functional capacity improved and caregiver burden decreased, enabling him to spend more time at home without the need of moving to a skilled nursing facility or hospice center.
Caring for compromised individuals can be an arduous task. Dressing, feeding, and maintaining appropriate hygiene for dependent patients is both mentally and physically exhausting. Caregivers may experience impaired psychological health, social isolation, and financial hardships [9,10]. Therefore, any improvement in a patient’s ability to care for themselves will likely reduce caregiver burden. Reduction of caregiver burden is an important goal given that caretakers are often spouses or close relatives of the patient. In the case described here, the patient’s wife, who served as his primary caretaker, experienced increasing difficulty managing on her own as her husband’s cancer progressed. Without inpatient rehabilitation, he would likely have been forced to relocate to a nursing facility. This outcome, while common, precludes patients from remaining at home or among family, where they feel most comfortable. Instead of relocating to a nursing facility, the patient was able to be safely discharged to his home following an inpatient rehabilitation stay that facilitated improvement in function and independence.
In addition to reducing caregiver burden and enabling patients to remain at home, inpatient rehabilitation may reduce long-term complications rates [11]. Patients with terminal cancer may experience emerging and progressive neurological, musculoskeletal, or other deficits. Educating patients and caregivers about the identification and management of progressive disorders may allow for earlier recognition and may minimize or delay their effects on functioning [12]. Physically transferring patients with limitations is a risky endeavor for both patients and their caregivers as poor preparation may result in falls and injuries [13]. The training patients and their caregivers receive while in rehabilitation will likely mitigate negative consequences associated with such maneuvers. Furthermore, a decrease in complication rates may translate to reduced healthcare costs, saving families and healthcare systems from preventable financial strains.
Cancer and its treatment also have a significant emotional toll on patients. Indeed, subsequent depression, anxiety, or emotionrelated fatigue may impact prognosis [14]. Importantly, decreases in functionality and independence resulting from cancer likely contribute to patients’ emotional decline. Optimizing patients’ function and quality of life will ideally improve overall mental state, motivation, and ability to continue treatment.
As physicians consider inpatient rehabilitation as an option for their patients, it is important to recognize that not all patients are suitable candidates. Performance status as assessed by the Eastern Cooperative Oncology Group (ECOG), Palliative Performance Scale (PPS), and Karnofsky Performance Status (KPS) appear to be good indicators of survival in patients with advanced cancer [15]. For example, recent research suggests that a KPS of 40 to 50 in patients with advanced cancer, for instance, is associated with a median survival of only 51 days [15]. Further McNair et al. (2021) have proposed using the KPS as a component of assessing patient suitability for inpatient cancer rehabilitation and risk for acute care transfer and early death [16]. Through the incorporation of the KPS for inpatient rehabilitation, practitioners should be able to identify good candidates for admission and better understand patient prognoses.
The integration of rehabilitation into the care of cancer patients allows for identification of early declines in function and the provision of as needed intervention. As noted in the case presented above, patients with terminal cancer can, when properly selected, benefit from inpatient rehabilitation. Inpatient rehabilitation can increase functionality and independence, permitting patients to remain at home further into the disease course. The integration of inpatient rehabilitation extends beyond those diagnosed with spinal cord tumors to include brain, digestive tract, bone, and respiratory system cancers. As cancer treatment continues to improve and survival rates increase, future research should examine the immediate and late effects of cancer therapy. Continued research will ideally inform evidence-based rehabilitation programs that benefit this unique patient population. Additionally, more advanced and nuanced means of assessing patient appropriateness for inpatient cancer rehabilitation should enable patients to maximize activities of daily living, even in the context of poor or unknown prognoses.
AUTHOR CONTRIBUTIONS
BB was responsible for performing chart reviews and drafting the manuscript. MS was responsible for editing and general oversight of the project.