Recalcitrant Atrial Tachyarrhythmias: An Emphasis on Managing Underlying Metabolic Irregularities
- 1. Department of Internal Medicine, Mayo Clinic Rochester, USA
- 2. Division of Cardiovascular Diseases; Mayo Clinic Rochester, USA
Abstract
A 76-year-old male presented in new-onset atrial flutter with rapid ventricular response. Pharmacologic and electric attempts at rate control with intravenous diltiazem, esmolol, digoxin, amiodarone and transesophageal echocardiogram-guided cardioversion were unsuccessful. While hospitalized, thyroid function studies detailed a low thyroid stimulating hormone level (TSH) and elevated free thyroxine accompanied by the findings two thyroid nodules on ultrasound, suggesting the diagnosis of toxic multinodular goiter. The patient’s methimazole dosage was titrated upwards which led to prompt conversion to normal sinus rhythm. This case demonstrates a distinct temporal correlation between the administration of methimazole and successful rate control and conversion to normal sinus rhythm in a gentleman who had failed typical pharmacologic and electric therapies.
Citation
Anderson BW, Liang JJ, Nkomo VT (2013) Recalcitrant Atrial Tachyarrhythmias: An Emphasis on Managing Underlying Metabolic Irregularities. JSM Clin Case Rep 1(1): 1003.
INTRODUCTION
Management of atrial fibrillation/flutter in the setting of thyrotoxic states including toxic multinodular goiter can be particularly challenging and refractory to conventional treatment unless the underlying metabolic abnormality is successfully recognized and reversed. Methimazole, a common treatment modality in the setting of toxic multinodular goiter, reduces thyroxine and triiodothyronine (T3) formation by inhibiting thyroperoxidase, diminishing the positive pacemaker function of T3. This case demonstrates a clear correlation between methimazole allocation, pharmacokinetics, and the achievement of heart rate control with conversion to normal sinus rhythm in the setting of recalcitrant atrial fibrillation/flutter.
CASE PRESENTATION
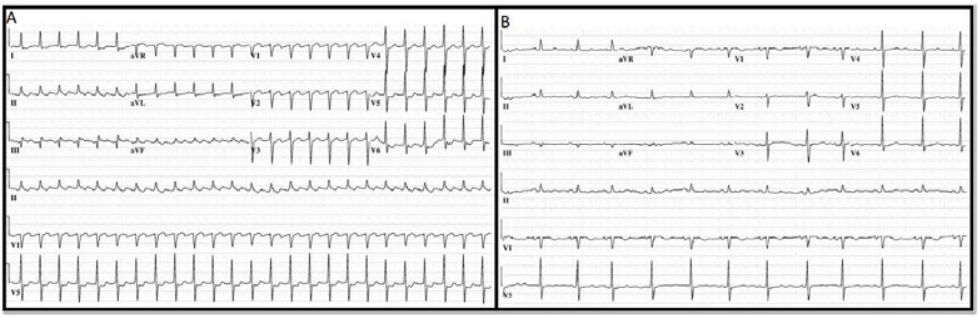
A 76-year-old male with no prior cardiac history presenting to the emergency department for abdominal pain was found to be in new-onset rapid atrial flutter with a ventricular rate of 150 beats per minute (Figure 1A).
Figure 1 (A) Electrocardiogram on presentation, demonstrating atrial flutter with rapid ventricular rate; (B) Electrocardiogram demonstrating conversion to normal sinus rhythm, 2.5 hours after 20 mg methimazole dosing.
Thyroid function studies detailed thyroid stimulating hormone (TSH) 0.03 mIU/L (normal 0.3- 5.0), free thyroxine 2.8 ng/dL (normal 0.8-1.8), free T3 2.9 pg/ mL (normal 2.0-3.5). History and physical examination revealed no obvious signs or symptoms of thyrotoxicosis. Coumadin and low-dose methimazole were initiated. Over the course of three days, pharmacologic attempts at rate control with intravenous
diltiazem, esmolol and digoxin failed. He subsequently underwent transesophageal echocardiogram-guided cardioversion which was unsuccessful. He was given intravenous amiodarone which temporarily converted him to a normal sinus rhythm, but he soon relapsed into atrial fibrillation. Thyroid ultrasound demonstrated two nodules, suggesting the diagnosis of toxic multinodular goiter. Given the recent introduction of amiodarone, I-123 scan or radioactive iodine ablation were not diagnostic or therapeutic possibilities. His methimazole dosage was subsequently titrated upwards which led to prompt conversion to normal sinus rhythm approximately 2.5 hours after the medication allotment (Figure 1B). Dexamethasone was started given the potential for Jod-Basedow phenomenon, or the production of thyroid hormone which is independent of normal regulation following iodine exposure [1]. After three days of continued normal sinus rate, the patient was discharged on dofetilide, propranolol, and methimazole. On hospital dismissal, he remained in normal sinus rhythm with a free thyroxine level of 1.5 ng/dL.
DISCUSSION
The recognition of underlying metabolic abnormalities in the setting of refractory atrial fibrillation/flutter is particularly important in elderly patients who are at increased risk for cardiovascular complications [2]. Methimazole plays an important role in the pharmacologic management of toxic multinodular goiter. Thionamides, including methimazole, inhibit the action of thyroperoxidase leading to reduction in iodine oxidation and subsequent formation of thyroxine and T3. Others have described several changes to cardiac pacemaker function by T3 which include the enhancement of sodium and potassium permeability,
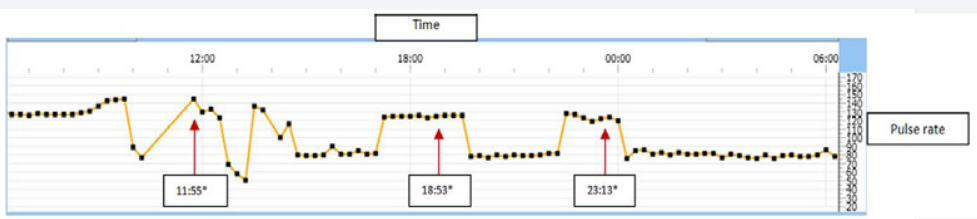
sodium pump density, and the expression of L-type calcium channel 1D which act to decrease action potential duration as well as atrial/ventricular node and atrial myocardium refractory periods [2,3,4]. The low-dose methimazole initiated several days prior to transfer to our facility likely made the patient receptive to the observed effects of methimazole upward titration given several days’ suppression of T3 synthesis. Okamura, et al have demonstrated maximal serum concentrations 1.8 +/- 1.4 h and 2.3 +/- 0.8 h following single doses of 10 mg in hyperthyroid patients but report similar peak concentrations using up to 30 mg dose while others have verified an elimination half-life of 4.9 to 5.7 hours [5,6]. As illustrated in (Figure 2), administration of 20-mg doses of methimazole was associated with acute change in heart rate and rhythm in a pattern which mirrored the expected kinetics of methimazole.
Figure 2 Heart rate response with 20-mg doses of methimazole given at indicated times (*).
CONCLUSIONS
This case highlights the dramatic effect of successful recognition and treatment of an underlying metabolic aberration in the setting of recalcitrant atrial tachyarrhythmia. Identification of etiologies such as toxic multinodular goiter is essential prior to the use of amiodarone therapy given its interference with further diagnostic and treatment modalities.