Report on Two Cases of Familial Restless Legs Syndrome Type 1 with Mutation and Literature Review
- 1. College of Acupuncture, Fujian University of Traditional Chinese Medicine, China
- 2. Department of Rehabilitation, Xiamen Hospital of Traditional Chinese Medicine, China
Abstract
Objective: The purpose of this study is to enhance the understanding of restless legs syndrome (RLS) and its variant types to reduce misdiagnosis in clinical practice.
Methods: Retrospective analysis of two cases of variant RLS in a family and a review of related literature was conducted.
Results: The first patient had recurrent shoulder pain for 8 years, and the mother had intermittent discomfort in both elbows and knees for more than 40 years. Both patients experienced relief of limb discomfort after activity, and the symptoms were more severe at night than during the day. After admission, RLS was diagnosed based on a comprehensive analysis, and both patients were treated with oral Pramipexole,with significant improvement in symptoms.
Conclusion: Although RLS typically involves only the legs, it may also affect other parts of the body. When patients complain of abnormal discomfort in a certain part of the body during rest and have a strong desire to move which can disappear temporarily after activity but recur during rest periods, RLS or its variant should be considered in the differential diagnosis.
Keywords
Variant restless legs syndrome, Restless shoulder syndrome, Restless elbow syndrome, VPS13C gene, Dopamine agonists
CITATION
Liu Y, Zhuang X, Li X, Shi Z, Wang Y, et al. (2023) Report on Two Cases of Familial Restless Legs Syndrome Type 1 with Mutation and Literature Review. JSM Clin Case Rep 11(4): 1223.
ABBREVIATIONS
RLS: Restless Legs Syndrome; MRI: Magnetic Resonance Imaging
INTRODUCTION
Restless Legs Syndrome (RLS) is primarily characterized by an intense, irresistible desire to move the legs, usually occurring in the evening or at night and worsening when the patient is at rest or inactive, but improving with movement. Abnormal urge to move in RLS can affect not only the legs but also other body parts of patients. When discomfort affects anatomical locations such as shoulders, arms, bladder, oral cavity, face, perineum, and meets the diagnostic criteria for Restless Legs Syndrome International Study Group [1]. It is referred to as RLS variant [2]. RLS variant is uncommon, with limited case reports, and patients often present with vague and diverse complaints [3]. Clinical physicians could easily misdiagnose, miss the diagnosis or have difficulty reaching a definitive diagnosis due to insufficient understanding of RLS variants and atypical symptoms in patients, delaying the treatment of the disease. Based on two cases of RLS patients from one family treated in our department and a review of relevant literature, this article explores the pathogenesis and treatment progress of RLS variants to increase clinical awareness of the disease for doctors.
CASE PRESENTATION
Medical Record
The first patient, a 39-years-old male, presented with a chief complaint of “repeated shoulder pain for over 8 years, aggravated for over 1 year.” He sought medical attention at the Rehabilitation Department of Xiamen Traditional Chinese Medicine Hospital, affiliated with Fujian University of Traditional Chinese Medicine, on May 18th, 2021. The patient reported that his shoulder pain appeared over 8 years ago without an obvious cause and worsened in cold weather. Rest provided minimal relief. He received acupuncture treatment for a diagnosis of “shoulder periarthritis” at an external hospital, with no significant improvement in symptoms. Over 1 year ago, the pain intensified, became persistent, and worse at night. The patient experienced pain in both shoulders alternately and lasted for about 1-2 hours, affecting his sleep, with no limb weakness or numbness. The shoulder pain could be relieved somewhat by a hot bath or therapy patches but not significantly eased. The patient had a history of “hyperthyroidism” in 2013 and developed “hypothyroidism” after receiving “131I” therapy in 2018.
Physical examination showed no abnormalities in the advanced neurological functions and cardiac, pulmonary, and abdominal checkups. Both shoulder joints were of normal appearance, without swelling or discoloration. The local skin color and temperature of both shoulder joints are normal, and there was no scapular deformity. Tenderness was noted in the bilateral shoulder posterior region, with a negative brachial plexus traction test, negative compression neck test, no tenderness in the cervical spine area, and a negative lift-off test. There was no notable muscle atrophy, and the skin sensation, muscle strength, and muscle tension of both upper limbs was normal, with normal tendon reflexes and no pathological signs found.
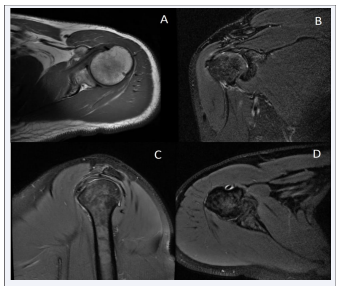
The auxiliary examination showed that the ultrasound of the bilateral shoulder joints revealed that there was partial bursa surface injury at the attachment site of the Greater Tuberosity of the Humerus muscle tendon on the right side and left side, thickening of the subacromial-subdeltoid bursa, and suspected bursitis. There was a lesion on the posterosuperior lip. The magnetic resonance image of the right shoulder joint revealed the following pathological changes: 1) a pseudo-cyst formation at the attachment site of the Greater Tuberosity of the Humerus muscle tendon; 2) degeneration of the supraspinatus muscle tendon; and 3) a small amount of effusion around the subacromial-subdeltoid bursa, the infraspinatus muscle tendon, and the long head tendon of the biceps brachii [Figure 1].
Figure 1: MRI images of the shoulder joint in patient 1 (A) –pseudocyst formation at the attachment of the greater tuberosity tendon of the humerus. (B) –degeneration of the supraspinatus tendon and subscapularis muscle edema. (C-D) –a small amount of fluid accumulation around the subacromial-subdeltoid bursa and the long head of the biceps tendon)
Medical history: Diagnosed with “1. Restless leg syndrome 2. Non-organic sleep disorder 3. Subacromial bursitis 4. Glenoid labrum injury”. Prescribed with Pramipexole dihydrochloride tablets 0.125mg, three times a day, oral; Diazepam tablets 2.5mg, once a day at night, orally. After taking the above medications for 9 days, the patient’s symptoms of nocturnal shoulder pain have disappeared, sleep has improved, and the patient is clinically cured.
Family history: Patient 2, the mother (73 years old), has a disease history similar to the proband for over 40 years. She experiences indescribable discomfort in the elbows and knees,such as tightness, acidity, and coldness, especially in the lower limbs. The discomfort occurs after the elbows and knees are static for more than half an hour, and can be relieved by joint activity such as flexion and extension. The discomfort worsens before sleep at night, and the patient gets up 3-4 times due to repeated discomfort in both knees during sleep. After examination by our department, the patient was found to have normal muscle strength and tension in both limbs, and the bilateral biceps reflex (+), triceps reflex (++), radial membrane reflex (+), knee tendon reflex (++), and Achilles tendon reflex (++). There was no patellar clonus or ankle clonus on both sides, no pathological signs were provoked, and the coordination test was normal. Additional tests, including routine tests, tumor markers, 6 items of thyroid function, glycosylated hemoglobin, complete biochemistry panel, serum ferritin determination, and erythrocyte sedimentation rate were conducted, but no significant abnormalities were found in coagulation function or electrocardiogram. The diagnosis was “restless legs syndrome”. The patient was treated with Pramipexole hydrochloride tablets 0.125mg, tid, po. The discomfort in the elbows and knees were significantly relieved after 13 days of treatment. The patient denied any other familial hereditary diseases.
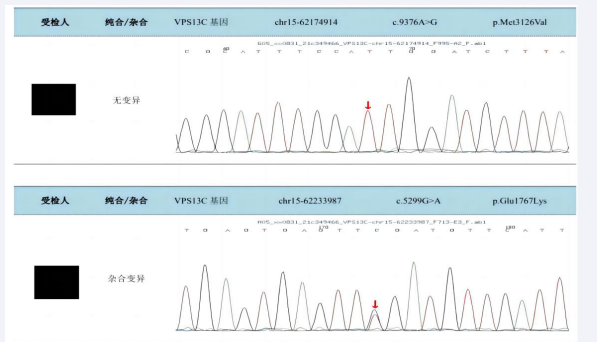
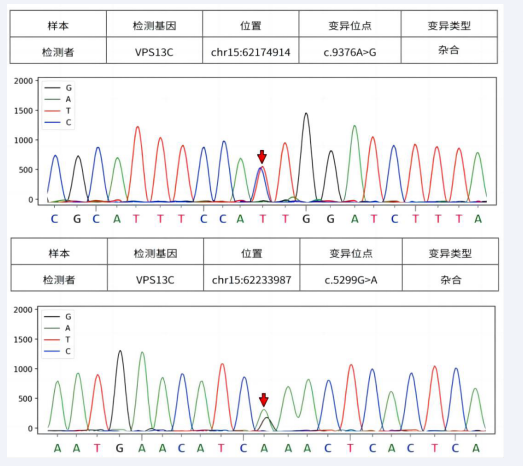
Genetic testing and mutation analysis: Patient 1 underwent high-throughput sequencing and was found to have a heterozygous mutation at position c.5299G>A on the VPS13C gene [Figure 2]. Patient 2 underwent high-throughput sequencing and was found to have two heterozygous mutations on the VPS13C gene at positions c.9376A>G and c.5299G>A [Figure 3].
Figure 2: High-throughput sequencing results shows that patient 1 has a heterozygous mutation of c.5299G>A in the VPS13C gene.
Figure 3: High-throughput sequencing showed that patient 2 carried the heterozygous mutation c.9376A>G and c.5299G>A in the VPS13C gene.
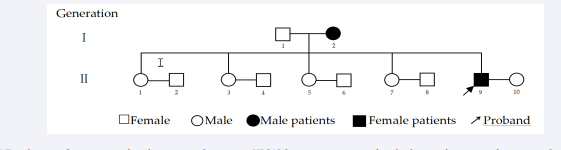
Patient family investigation: There are two patients in this family, one in the first generation (patient 2) and one in the second generation (patient 1). Patient 1 mainly presents symptoms of discomfort in both shoulder areas, with a course of disease exceeding 8 years. Patient 2 mainly presents symptoms of discomfort in both elbow and knee areas, with a course of disease exceeding 40 years [Figure 4].
Figure 4: Family tree of a patient with a chromosomal recessive VPS13C gene mutation, with only the pre-documented patient in 2 generations.
DISCUSSION
The article reports on the analysis of a family with RLS. Patients in this family exhibit persistent shoulder or elbow and knee discomfort, with discomfort worsening at night and relieving after activities. Secondary causes and behavioral habits have been excluded based on medical history, and primary RLS is considered. After treatment with Pramipexole, symptoms of limb discomfort in two patients in this family improved significantly, indicating a correlation between RLS occurrence in this family and genetic inheritance and dopamine dysfunction.
Currently, primary RLS is believed be a complex genetic disease. Foreign scholars have conducted genetic studies on RLS patients and found many genetic loci such as MEIS1, PTPRD, and NOS1 have relation to RLS occurrence [4,5]. Among them, the MEIS1 locus has the highest correlation with RLS [6]. However, known genetic mutation sites can only explain the pathogenesis of a few RLS patients, and the genetic characteristics of the vast majority of RLS patients remain unclear. Previous reports have revealed that diseases such as stroke, diabetes, uremia, brain tuberculoma, Parkinson’s disease (PD), and spinocerebellar ataxia carry a risk of secondary RLS.
The treatment of RLS aims to relieve or eliminate restless symptoms, thus improving sleep and quality of life. For secondary RLS caused by an underlying condition, the treatment focuses on addressing the primary cause. Current guidelines recommend medications such as dopamine agonists, anticonvulsants, opioids, and sedatives for RLS treatment, as well as non-pharmacological therapies such as exercise therapy, traditional Chinese medicine, and physical therapy, which can also help improve restless leg symptoms
The genetic testing results of the two patients in this article both showed mutations in the VPS13C gene. Patient 1 had a variation at site c.5299G>A, while Patient 2 had variations at sites c.9376A>G and c.5299G>A. According to relevant databases, the disease associated with these variant sites is autosomal recessive early-onset parkinsonism type 23 [7]. Based on the patients’ disease data, the pathogenic significance of the mutant RLS caused by this variation is not yet clear. Parkinson’s disease is a movement disorder, while RLS belongs to the category of sleep disorders. The incidence of RLS in PD patients is not low [7], but the existence of a genetic causal relationship between RLS and PD is still disputed [8,9]. The “suspect” genes mutated in the two patients in this case report are related to early-onset PD, which is characterized by the onset of PD in young adults and progressive cognitive impairment leading to dementia and autonomic dysfunction. Whether the restless symptoms in this family are a preclinical manifestation of PD and whether they will develop into PD with cognitive impairment and other diseases in the future remains unknown, and the relationship between the two needs further exploration. Our team will track and follow up on this family, and record any changes in their condition in the future.
Researchers in China have summarized and classified various subtypes of restless legs syndrome (RLS), including five subtypes of restless leg syndrome - restless mouth syndrome, restless arms syndrome, restless abdomen syndrome, restless genital syndrome, and restless bladder syndrome - according to a study [10]. In addition, foreign scholars have reported clinical cases of back [11,12], facial [13], head [14], chest [15], anal [16], intestinal [17], and shoulder [18] restlessness. Matsubara [18] reported a case of a patient with post-stroke symptoms who experienced a strong desire to move both shoulders during quiet periods and before bedtime. After taking dopamine medication, the symptoms improved remarkably. The author suggested that shoulder restlessness may be a subtype of RLS and speculated that the occurrence of abnormal sensations on both sides of the shoulders in the patient may be related to cervical vertebra C5 damage and stroke, although there was no detailed examination of the cervical vertebrae in the article. The etiology of variant RLS is not yet fully understood, and the incidence of each subtype is still unknown. Based on the clinical data of two patients in this article, it remains to be discovered and explored whether there are other variant subtypes of RLS, such as “restless shoulder syndrome” or “restless elbow syndrome.”
CONCLUSION
In summary, the clinical diagnosis of variant RLS relies mainly on the clinical presentation of the patient, but discomfort in other parts of the body has similar or even overlapping clinical manifestations to their systemic disorders, and the lack of specificity in the ancillary investigations often leads to confusion and misdiagnosis by the receiving physician. Therefore, this case report also suggests that clinicians should consider the possibility of RLS or its variants if they encounter discomfort in an anatomical area of the body during sleep or in a quiet state at night, causing the patient to have a desire to move frequently, in order to diagnose and treat the patient early and alleviate suffering.
FUNDING
Fujian Province Health and Health Young and Middle-aged Backbone Talent Training Project. (2020GGB066).