Sepsis as a Cause of Acquired Protein C and Protein S Deficiency- a Case Report and Literature Review
- 1. Internal Medicine, Canton Medical Education Foundation, USA
Abstract
Warfarin Induced Skin Necrosis is a well-known and dreaded complication in patients who is being started on warfarin without adequate bridging with other anticoagulants. The mechanism is thought to be due to protein C deficiency acquired after initial exposure to warfarin. We present a rather unusual cause of protein C deficiency due to sepsis resulting in warfarin induced skin necrosis. 43 year old lady who has been on chronic warfarin therapy secondary to anti phospholipid syndrome was admitted to the hospital for acute ischemic cerebellar stroke. Warfarin was held due to acute thrombocytopenia. She was discharged to a facility after restarting the warfarin at the same dose. She presented back to the hospital with septic shock due to pneumonia. She was found to have multiple necrotic areas consistent with skin necrosis. Unfortunately, patient died due to multi organ failure despite goal directed therapy. This case demonstrates the importance of recognizing the sepsis as an acquired cause of protein C deficiency.
Keywords
Sepsis; Warfarin; Skin necrosis; Protein C; Protein S
Citation
Kannan A, Chandra S, Lizcano J, Murphy C (2014) Sepsis as a Cause of Acquired Protein C and Protein S Deficiency- a Case Report and Literature Review. JSM Clin Case Rep 2(2): 1028.
ABBREVIATIONS
APS: Antiphospholipid Syndrome; DVT: Deep Vein Thrombosis; PE: Pulmonary Embolism; WISN: Warfarin-Induced Skin Necrosis
INTRODUCTION
Warfarin-induced skin necrosis is a rare (prevalence of 0.01- 0.1% of warfarin treated patients) but potentially life threatening complication of anticoagulant therapy with an associated morbidity and mortality requiring immediate drug cessation. Warfarin is a highly effective anticoagulant widely used for the primary and secondary prevention of thromboembolic disorders in current medical practice. The drug is administered orally, absorbed in the gastrointestinal tract, bound to serum albumin, metabolized by the hepatic CYP2C9 enzyme, and excreted as an inactive metabolite into bile. Adverse effects associated with the use of warfarin include bleeding, hepatitis, priapism, alopecia, pruritic macular and papular eruption, purple toe syndrome (cholesterol microembolization), and cutaneous necrosis.
CASE PRESENTATION
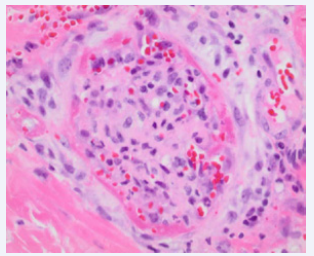
43 year old Caucasian female with a history of antiphospholipid syndrome (APLS), multiple DVTs and PEs on chronic Warfarin therapy for 10 years was admitted to the hospital. Recently patient was admitted to the hospital for ischemic cerebellar stroke and Warfarin was held due to acute thrombocytopenia. Warfarin was restarted again on the same dose (7.5 mg) with adequate bridging and sent to Nursing Home. About 10 days later patient was brought again with fever, hypotension. She was found to be in septic shock likely secondary to pneumonia and admitted to Intensive Care Unit. She also complained of black eschar lesions under inframammary and groin area. Upon further questioning it was revealed that lesion was of recent onset about 5-6 days after restarting Warfarin. It started as an erythematous lesion and within 48 hours it progressed to painful black lesions. It was 6cm by 15 cm underneath the left breast and 7cm by 12cm in the left groin. Considering the septic shock, necrotizing fasciitis was considered but it was ruled out by a surgeon. Warfarin was held and patient was put on heparin intravenously .Biopsy was done and it revealed skin with superficial dermal fibrin thrombi, hemorrhage and ischemic changes. These findings were consistent with Warfarin Induced Skin Necrosis (WISN). Unfortunately despite treatment patient died due to multi organ failure.
DISCUSSION
So far, in literature approximately 300 cases of (WISN) have been reported. The earliest symptoms of WISN appeared within 10 days of restarting the warfarin with the peak incidence between days 3 and 6 (83-90% of cases) [1,2] (Figure 1).
Figure 1 Skin necrosis seen underneath her left breast thought to be due to depletion of Protein C and S.
WISN is a potentially catastrophic complication of warfarin therapy that arises as a consequence of different half lives of different vitamin K dependent proteins. One day after initiation of the usual doses of warfarin, the level of protein C almost decreases by 50 %( same as factor VII). Rest of the vitamin K dependent clotting factors have half life longer than that (48-60 hrs) and declines more slowly in the serum leading to a transient imbalance in the proteins of the procoagulant-anticoagulant system occurring during the initial phase of anticoagulation which creates a hypercoagulable state. This leads to thrombotic occlusions of the microvasculature causing the necrosis as seen in our patient. The effect is more pronounced when a higher dose of warfarin is administered.
The commonest cause has been attributed to hereditary protein C deficiency. [3-5]. Other condition causing WISN is acquired causes of protein C deficiency like acute thrombosis, warfarin therapy, vitamin K deficiency [5], liver disease, disseminated intravascular coagulation, chemotherapeutic agents for breast cancer [6,7 ], sepsis [8,9], primary antiphospholipid syndrome [10], acute exacerbation of ulcerative colitis [11], protein C auto-antibody formation[12] (Figure 2).
Figure 2 Histopathological stain revealed dermal fibrin thrombi consistent with warfarin induced skin necrosis.
In our patient, the appearance of necrotic skin lesion which appeared on the 6-th day of reintroduction of warfarin therapy and later, on biopsy was proven to be WISN is speculated to have multifactorial etiology. Recent reintroduction of warfarin and also coexistence of septic shock which is known to be one of the causes of transient acquired protein C deficiency. Unfortunately patient was already started on heparin by weight to bridge the
therapy as she had a history of antiphospholipid syndrome with multiple episodes of thrombosis in the past and level of protein C and S could not be accessed. Patient was also started on broad spectrum antibiotics on admission due to being in septic shock, which could have further contributed to the acquired protein C deficiency by reducing gut flora, intestinal malabsorption and thus reducing vitamin K levels.
Our literature search has so far exposed only two cases of acquired protein C deficiency [13,14]. One of these patients had similar catastrophic outcome as our patient- Death from multiorgan failure.