Traumatic Intracranial Aneurysm (TICA) following Closed Head Injury in Children : A Case Report
- 1. Department of Surgery, Universiti Kebangsaan Malaysia, Malaysia
- 2. Department of Neurosurgery, Hospital Sultanah Nur Zahirah, Malaysia
- 3. Faculty of Medicine, Universiti Sultan Zainal Abidin, Malaysia
Abstract
We report a case of traumatic intracranial aneurysm (TICA) in a 9-year-old boy who sustained a closed traumatic head injury and presented with signs and symptoms of intracranial hemorrhage complicated with high intracranial pressure (ICP) associated with hydrocephalus after 11 days of motor vehicle acccident (MVA). TICA is a very rare form of intracranial aneurysm and only represent for less than 1% of all intracranial aneurysm. Children and adolescents account for 30% of the reported incidence of TICA: in which 44% were diagnosed in the first decade of life, and 56% in the second decade. Despite the advancement of imaging techniques, diagnosis of TICA still requires a high index of suspicion and continued vigilance, particularly in traumatic head injury children with worsening neurologic deterioration, or those who fails to improve neurologically as expected following treatment. TICA in children may present early or late. Majority of the cases will presented early with intracranial hemorrhage, while late presentation occurs infrequently as an aneurysmal mass. Outcome of TICA among children is determined by the extent of traumatic injury and the preoperative clinical status of the children which directly determined by the diagnosis of the aneurysm prior to either initial or repeated hemorrhage.
Keywords
Traumatic Intracranial Aneurysm (TICA), Children, Closed traumatic head injury, Endovascular occlusion
Citation
Emir AF, Udin N, Othman AK, Salim NN, Mohamad Supi NAL, Abdullah AS (2022) Traumatic Intracranial Aneurysm (TICA) following Closed Head Injury in Children : A Case Report. JSM Clin Case Rep 10(2): 1204.
CASE PRESENTATION
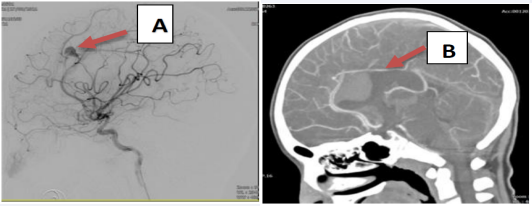
A 9-year-old boy had been healthy prior to sustaining a moderate traumatic brain injury in a motor vehicle accident. Urgent CT scan of brain revealed posterior interhemispheric bleed with no skull bone fracture. He was discharged home with no neurological deficit after 5 days of observation in the neurosurgical ward. However, 11 days after sustaining moderate brain injury, the boy was presented to our emergency department (ED) with generalized seizure with uprolling of eyeballs and jerky movement of both upper and lower limbs, preceeded by multiple episodes of vomiting prior to his seizure. His GCS upon admission to emergency department was E3V2M5 with pupils of 2mm and reactive bilaterally. CT scan of the brain revealed a new anterior interhemispheric bleed with intraventricular hemorrhage; but no hydrocephalus. While warded for close observation, 3 days later he developed another episode of generalized seizure and repeated CT scan of the brain revealed a worsening hydrocephalus [1]. Emergency external ventricular drainage insertion was performed to relieve the hydrocephalus. CT Angiography of the cerebral artery revealed a small saccular aneurysm at A3 segment of left anterior cerebral artery circulation measuring 0.3cm x 0.2cm x 0.2cm. He was referred to specialized tertiary centre with interventional rediologist and underwent Digital Substraction Angiography (DSA) which revealed a left A3 segment saccular aneurysm measuring 0.8cm x 0.8cm with the neck of 0.3cm (Figure 1). An endovascular coilling was successfully done with no complication and was referred back to our care for further management and observation. He was discharged home with no recurrence seizure 11 days after endovascular coilling of his cerebral artery aneurysm. He was planned for repeat DSA after 1 year with 3 monthly follow up to review his neurological status.
Figure 1: CTA showing A3 aneurysm (A) with interhemispheric bleed (B).
DISCUSSION
Mechanism of arterial injury that lead to TICA can be related to closed head injury, missile injuries, penetrating head injury, and iatrogenic injury during the course of surgery within or about, the skull or its base, the ear, the nose or sinuses, the orbit, or other facial structures [2]. Most common sites [3] of TICA in children are distal ACA (38%), ICA (29%), Distal MCA (25%) and vertebralbasilar system (8%). As for our patient, the aneurysm developed at A3 segment of left anterior cerebral artery circulation which were probably related to acceleration-deceleration injury related to his motor vehicle accident. This occurence were siimilar to the observation done by Buckingham3 in which accelerationdecelaration injuries commonly traumatize the distal ACA or its branches. In his observation, Buckingham [3] also revealed that closed head injury typically involves three arterial sites; skull base fracture injures the carvenous or supraclinoid ICA, or, less commonly, the petrous ICA; convexity fractures often injures the cortical MCA branches; and acceleration-decelaration injuries commonly traumatize the distal ACA or its branches.
The interval from trauma to the onset of symptoms or diagnosis of TICA varied considerably, with most of the patients presented with the interval of within 3-4 weeks [1] after the trauma, which was defined as early presentation in children and adults. Early presentation of TICA are commonly manifested as intracranial hemorrhage, while late presentation of TICA which occurs infrequently, typically manifested as aneurysmal mass.
It is known that clinical presentation of TICA in children vary considerably. The most common symptoms include an acutely decreasedlevel of connsciousness, seizure, or focal neurological deficit [4]. Our patient presented with generalized seizure associated with vomiting after 11 days of the initial trauma. This sudden neurologic deterioratian after days of closed head injury triggered us to think about the possibility of TICA. As observed by Yazback et al [5], delayed neurologic decline or failure to improve as expected after blunt or penetrating head injury suggest that a traumatic aneurysm or an undiagnosed vascular injury may occured. It is important to stated that timely diagnosis of TICA depends upon a high index of suspicion that lesion is, or may be present in our patients. Once triggered, the patient must promptly undergo diagnostic intracranial imaging. As mentioned by Ventureyra et al [2], documented subarachnoid hemorrhage, intracerebral or intraventricular hemorrhage, or subdural hemorrhage should be further investigated by cerebral angiography to exclude TICA or other vascular lesion.
The mortality rate for patients with TICA can be as high as 50%. Survival and functional outcome of children with TICA depends on several factors [6] which include; the severity and extent of the primary and secondary brain and central nervous system (CNS) insult generated during the initial trauma, the presence or absence of one or more aneurysmal hemorrhage prior to the diagnosis of TICA, the interval and clinical outcome prior to definitive treatment of TICA, and the presence or absence of treatment complications in managing TICA.
With the prompt diagnosis of TICA based on areriography, our goal of treatment for our patient is to exclude the aneurysm from the circulation either by surgical approach or by endovascular methods. Fleischer et al6 reported those patients with TICA who were treated conservatively had a 41% mortality as compared to 18% mortality to those who were treated surgically, and those who were treated conservatively had a poorer outcomes. Therefore, we were agreed that aggressive surgical management is the most appropiate approach for our patient and prompt craniotomy with clipping, resection, or trapping of the aneurysm is considered to be the choice of definitive management for our patient. Our patient was immediately referred to specialized tertiary centre for endovascular occlusion and embolization of the aneurysm.
SUMMARY
TICA following closed head injury represent with both diagnostic challenge and surgical difficuties to the clinician. Although its comprising of less than 1% of all cerebral aneurysm, it was associated with significant morbidity and a mortality rate as high as 50%. Despite the advancement of imaging techniques, diagnosis of TICA still requires a high index of suspicion and continued vigilance, particularly in traumatic head injury children with worsening neurologic deterioration, or those who fails to improve neurologically as expected following treatment. Outcome of TICA among children is determined by the extent of traumatic injury and the preoperative clinical status of the children which directly determined by the diagnosis of the aneurysm prior to either initial or repeated hemorrhage with the goal of treatment is to exclude the aneurysm from the circulation either by surgical approach or by endovascular methods.
ACKNOWLEDGEMENTS
The authors would like to thank the Director General of Health Malaysia for his permission to publish this article. The authors would also like to acknowledge all the multidisciplinary members of neurosurgery, anaesthesia and histopathology for their dedications and support in managing this case.
COMPLIANCE WITH ETHICS GUIDELINES
AF Emir, Nujaimin Udin, and Abdul Karim Othman, Nur Najmi Salim, Nur Aiman Liyana Mohamad Supi and Amira Salwa Abdullah declare that they have no conflict of interest. Patient anonymity was preserved, and this article does not contain any studies with animal subjects performed by any of the authors.
REFERENCES
1. Fox JL. Intracranial aneurysms. Springer, New York Berlin Heidelberg. 1983; 419-431: 1453-1463.
5. Yazbak PA, McComb JG, Raffel C. Traumatic aneurysm in childhood. Pediatric Section, American Academy of Neurological Surgeons, 21st Winter Meeting, Vancouver. 1992.