Traumatic Optic Neuropathy Related to Facial Trauma: Literature Review and Case Report
- 1. DMD Candidate, University of Pennsylvania, USA
Abstract
Blindness following facial trauma is a rare but serious complication. Traumatic optic neuropathy (TON) is a condition in which vision loss is due to direct or indirect trauma to the optic nerve. Here we present a case of a 30-year-old female that was struck by a car while riding her bicycle that immediately lost vision in her right eye. The current treatment options for TON are surgical optic nerve decompression and corticosteroids. Neither treatment has been shown to be overtly effective for traumatically induced visual deficiencies. There is a need for novel research looking for new treatment modalities for TON.
Citation
Rose MJ (2022) Traumatic Optic Neuropathy Related to Facial Trauma: Literature Review and Case Report. JSM Clin Case Rep 10(1): 1198.
INTRODUCTION
Facial trauma leading to blindness has been well documented for millennia. Hippocrates unearthed a condition that was not formally documented until 1840 by William MacKenzie. Today it is known as sympathetic ophthalmia [1]. Sympathetic ophthalmia is the autoimmune triggered destruction of a previously uninjured eye following a traumatic injury to the contralateral eye.
Today, much progress has been made in the treatment and prevention of sympathetic ophthalmia [2]. However, there is still a need for advancements in the treatment of traumatically injured eyes. Traumatic optic neuropathy (TON) is a condition in which vision loss is due to trauma affecting the optic nerve directly or indirectly. Direct traumatic optic neuropathy includes situations in which the trauma or the resultant fracture directly insults the optic nerve by penetration or severing of the nerve fibers. More common is the indirect mechanism of injury where the sequela of the impact results in secondary damage to the nerve. These secondary mechanisms include disruption of blood supply to the nerve, shearing of the nerve fibers from the shock of the impact, and a variety of compartment syndrome related pathologies. Damage to the small vessels and bleeding behind the globe and in front of the exit of the optic canal to the orbit can produce a tremendous amount of pressure on the optic nerve sheath. The result is insufficient blood flow and ischemic injury to the optic nerve due to compression of the central retinal artery and other branches of the ophthalmic artery. These compressions ultimately lead to hypoxic injury of the nerve and finally to blindness [3].
CASE PRESENTATION
A 30-year-old female patient presented with immediate and complete unilateral loss of vision in her right eye after being struck by a car while riding her bicycle. Upon arrival at the hospital, she stated that she had no loss of consciousness and was wearing a helmet. Further examination noted moderate swelling over the right zygoma, right-sided periorbital ecchymosis and no light perception in her right eye. Her only facial injury was a right zygomaticomaxillary complex (ZMC) fracture [Figures 1,2].
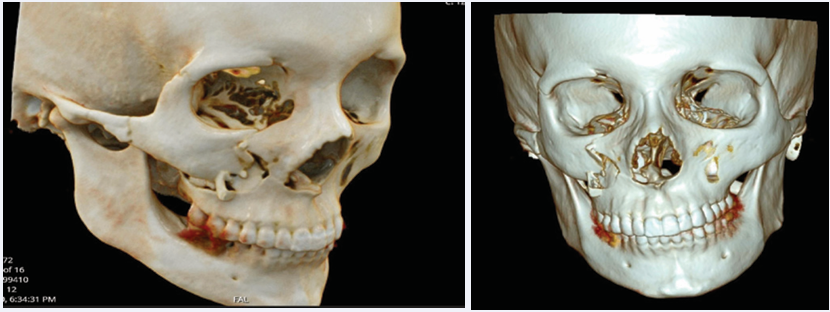
Figure 1 and 2 3D Reconstruction of CT Maxillofacial Images. Right ZMC fracture with the zygoma separated away from the maxilla at the zygomaxillary suture. A fracture of the right zygomatic arch is also present.
A nondisplaced fracture of the right middle cranial fossa across the sphenoid wing was also visualized. This fracture line extended across the inferior orbital fissure as well as along the right posterior superior orbit. The optic nerve canal was shown to have minimal distortion, but the right foramen rotundum exhibited distortion. Clinically, there was paresthesia (7/10) of the maxillary branch of the trigeminal nerve on the right side related to the fracture that involved the foramen rotundum.
Coordination between oral and maxillofacial surgery and ophthalmology concluded that the bony fractures and swelling alone did not explain the severity of her optic neuropathy. Ophthalmologic evaluation recorded no light perception and a positive afferent pupillary defect (APD) of the right eye. The loss of vision as the patient reports was instantaneous following the accident. This finding suggests the injury to the nerve was from a shearing of the axons within the optic canal.
In this situation, there is conflicting evidence for the role of systemic steroids to reduce the optic nerve edema in hopes of regaining vision [4-6]. There was not a role for surgery to attempt decompression of the optic canal as this would not restore her vision and could result in significant morbidity. She had no contraindications to steroids and was started a short course of IV methylprednisolone 1g for 3 days. Surgical repair of the ZMC fracture was completed for esthetic purposes. No surgical attempt was made to correct the blindness. She did not regain vision in her right eye.
DISCUSSION
The case presented is rarely the norm; the blunt force impact associated with a fractured ZMC does not commonly lead to immediate and permanent blindness. A review of the literature yields an equally unfortunate case report from Great Britain in 1986 [7]. A 15-year-old boy fell off his bicycle hitting the right side of his face on the pavement. He was admitted to the hospital with complete and immediate loss of vision on the right side while only sustaining minor skin abrasions. He experienced no bony injuries and no loss of consciousness. A CT scan revealed that no bones had fractured and that there was no hematoma formation. Corticosteroid therapy was initiated but discontinued after 48 hours as there was no improvement in his vision. The researchers discuss that the blindness was likely due to a variety of etiologies from hemorrhage to necrosis and shearing of nerve fibers. All together these contributed to the loss of vision. This case serves as a rare example of how blunt trauma to the face can have dramatic effects even without any skeletal fractures [7].
The medical management of traumatic optic neuropathy lacks any definitive consensus. The two dominating treatment modalities used today are high dose corticosteroids and surgical decompression of the optic canal. Following facial trauma and before conducting any definitive treatment, a CT scan provides a very effective and targeted view which can help guide the course of treatment. Visualization of bony fragments, soft tissue pathology, or an intact optic canal informs the treating physicians on how to proceed. Therefore, a CT should be the standard of care in any facial trauma [8].
Following an appropriate diagnosis of TON, the use of corticosteroids in nerve injuries has been demonstrated to be beneficial. Corticosteroids have neuroprotective effects that are vital to saving an acutely inflamed optic nerve. A combination of different cellular and molecular mechanisms contributes to the positive effects of corticosteroids. Of these, the ability of the steroids to limit free radical oxidative injury and lipid degeneration is crucial to its nerve saving properties [9]. The most commonly administered corticosteroid when deemed necessary is mega-dose (>5,400mg) IV methylprednisolone. Cementing the importance and efficacy of steroids in acute nerve injury was a 1990 study, referred to as the National Acute Spinal Cord Injury Study (NASCI) published in the New England Journal of Medicine [10].
The timing and duration of administration is also an important prognostic factor. If given within 8 hours of the injury and continued for 48 hours, better clinical outcomes were observed [11].
Inherently, patients being treated for TON are often accompanied by traumatic brain injury (TBI) as a result of the initial trauma. One study showed that there was an increased risk of death associated with TBI and corticosteroids [12]. They affirmed that corticosteroids must be avoided when managing patients with brain injuries. This study is in stark conflict with the NASCI study that many use as proof of the overall efficacy of corticosteroids in TON.
Surgical intervention is reserved for a select few circumstances in the treatment of traumatic optic neuropathy. Radiographic evidence of optic canal fracture, bony fragments impinging on the canal or edema and hematoma compressing the optic nerve are indications for surgical intervention. The surgical technique used most commonly today is the Endoscopic Optic Nerve Decompression (EOND) [4]. Apart from the lack of evidence that supports the effectiveness of surgical decompression as a treatment for TON, the complications of surgical decompression are well documented. Ten percent of patients undergoing surgical decompression experienced post-surgical cerebrospinal fluid leakage [5]. Researchers suggest that due to the high likelihood of associated morbidity that the best treatment for TON that requires surgery, is no surgery at all. Together with the limited success of surgical intervention paired with the complications of surgery and the reality that TON patients can recover vision when treated conservatively, there is very limited evidence supporting the use of surgical intervention for treating TON cases [13].
Numerous studies have discovered that there is no consensus on the best course of action for TON following facial trauma. An article published in the American Academy of Ophthalmology tracked the visual improvement in 133 patients with TON compared with the three different interventions used in their care. The three interventions were surgical decompression, corticosteroids, and no treatment. The results yielded that there was no statistical difference in visual improvement regardless of the treatment or the patient’s baseline visual acuity [5].
This sentiment was proven again by others who discovered that all patients regardless of which treatment modality used, all had a visual recovery rate of approximately 50% [4].
A third study, The International Optic Nerve Study again failed to show that one treatment modality was better than no treatment. They even go as far as to say “neither corticosteroid therapy nor optic canal decompression should be considered the standard of care for patients with traumatic optic neuropathy” [6].
The overall lack of consensus and weakness of treatment success for conservative, surgical, and corticosteroid treatments offers little to guide physicians for the treatment of acute traumatic optic neuropathy. The literature has established repeatedly that there is limited success with surgical and corticosteroid intervention in TON following facial trauma. Further studies showing more of the same would fail to add any value to the medical literature. There is a great need for novel research looking for new treatment modalities or improvements to the currently accepted treatment options. An unfortunate reality is that TON treatments are still in their infancy and that much more work is left to be done, even 2,500 years after Hippocrates noted the association of blindness following facial trauma.
REFERENCES
- Rahi A. Immunological investigations in post-traumatic granulomatous and non-granulomatous uveitis. Br J Ophthalmol. 1978; 62: 722-728.
- CC Chan, RG Roberge, SM Whitcup, RB Nussenblatt. 32 Cases of Sympathetic Ophthalmia. Archives of Ophthalmology. 1995; 113: 597.
- Ronald P. Bossert, John A. Girotto. Blindness following Facial Fracture: Treatment Modalities and Outcomes. Craniomaxillofac Trauma Reconstr. 2009; 2: 117–124.
- Kumaran A, Sundar G, Chye L. Traumatic Optic Neuropathy: A Review. Craniomaxillofac Trauma Reconstr. 2015; 8: 31–41.
- LA Levin, RW Beck, MP Joseph, SSeiff, R Kraker. The treatment of traumatic optic neuropathy. Ophthalmology. 1999; 106: 1268–1277.
- Sarvesh B Urolagin, Sharadindu M Kotrashetti, Tejraj P Kale, Lingaraj J Balihallimath. Traumatic Optic Neuropathy After Maxillofacial Trauma: A Review of 8 Cases. J Oral Maxillofac Surg. 2012; 70: 1123– 1130.
- Babajews A, Williams J. Blindness after trauma insufficient to cause bony injury: Case report and review. British Journal of Oral and Maxillofacial Surgery. 1986; 24: 7–11.
- Yu-Wai-Man P. Traumatic optic neuropathy—Clinical features and management issues. Taiwan J Ophthalmol. 2015; 5: 3–8.
- Bains M, Hall ED. Antioxidant therapies in traumatic brain and spinal cord injury. Biochim Biophys Acta. 2012; 1822: 675–684.
- Rosner MJ. National acute spinal cord injury study of methylprednisolone or naloxone. Neurosurgery. 1991; 628.
- MB Bracken, MJ Shepard, WF Collins Jr, TR Holford, DS Baskin, HM Eisenberg, et al. Methylprednisolone or naloxone treatment after acute spinal cord injury: 1-year follow-up data. J Neurosurg. 1992; 76: 23–31.
- Phil Edwards, Miguel Arango, Laura Balica, Rowland Cottingham, Hesham El-Sayed, Barbara Farrell, et al. Final results of MRC CRASH, a randomized placebo-controlled trial of intravenous corticosteroid in adults with head injury—outcomes at 6 months. Lancet. 2005; 365: 1957–1959.
- Cassandra B Onofrey, David T Tse, Thomas E Johnson, Ann G Neff, Sander Dubovy, Billy E Buck, et al. Optic Canal Decompression: A Cadaveric Study of the Effects of Surgery. Ophthalmic Plast Reconstr Surg. 2007; 23: 261–266.