Yolk Sac Tumor of the Lung with Elements of Mixed Germ Cell Tumor in Pediatrics: Case presentation and literature review
- 1. Degree Specialist in Pediatric Surgery, Cuba
- 2. Degree Specialist in Pediatric Surgery and Oncology, Cuba
- 3. Professor, Senior Researcher, Master in Comprehensive Child Care, Doctor in Medical Sciences. “William Soler Ledea” University Pediatric Hospital, Cuba
Summary
Introduction: Germ cell tumors in childhood occur at a rate of 2 to 3 cases per million inhabitants, representing 1 to 2% of malignant solid tumors in the pediatric population, becoming the malignant tumors with the highest incidence in testicles in males and ovaries in females. The second place of presentation of extragonadal germ cell tumors is in the mediastinum with or without infiltration of the lung. One of the main means for diagnosis is the determination of serum markers: Alpha-Fetoprotein (AFP) and Beta fraction of chorionic gonadotropin.
Objective: To describe a patient with a malignant tumor of the yolk sac of the lung with bone metastases at debut.
Case presentation: White male patient who, at the age of 3 years, began to experience painful urination, constipation, edema of the lower limbs, and gait disorders. In the diagnostic imaging studies, a tumor was detected in the right lung, with metastasis to the Lumbar Spine (L-5) at debut, with elevation of the alpha-fetoprotein tumor marker. A thoracoscopic biopsy was performed and the result was yolk sac tumor with elements of mixed germ cell tumor.
Our greatest desire is to make the medical population aware of the infrequent location of this variant of tumor in the lung in pediatric age and the
importance of timely diagnosis of the disease.
KEYWORDS
- Yolk sac tumor
- Germ cell tumor
- Lung
- Pediatrics
CITATION
Cañizares CCV (2024) Yolk Sac Tumor of the Lung with Elements of Mixed Germ Cell Tumor in Pediatrics: Case presentation and literature review. JSM Clin Case Rep 12(4): 1250.
INTRODUCTION
Malignant tumors in pediatrics represent only 2% of cancer cases, however, neoplasms are currently the second cause of death in children over 1 year of age. In our country, approximately 300 to 350 new cases are diagnosed each year [1,2].
Endodermal sinus tumors (yolk sac) are malignant neoplasms of germinal origin, which are characterized by their embryological differentiation from structures of the yolk sac. They are very rare tumors, of rapid growth and that usually develop in adolescent ovaries and young women, of reproductive age and in testicles mainly in children and adolescents, other locations are rare, and despite some similarities between childhood Yolk sac tumors with In adults, there are important differences, for example, the spread of pediatric tumors is carried out especially via the hematogenous route [3-5], unlike malignant testicular tumors in adults, which do so via the lymphatic route.
The most used tumor marker is Alpha-Fetoprotein (AFP), which is linked to the presence of the yolk component, which is elevated in more than 90% of cases [6,7].
Primary malignant lung tumors in childhood are very rare, with bronchial adenoma being the most common; Next in frequency is bronchogenic carcinoma, which occurs mainly in patients with cystic Adenomatoid Malformations (ACM) or bronchogenic cysts; Another neoplasm associated with congenital lung pathology is Pleuropulmonary Blastoma, associated with intralobar sequestrations and MAQ [1,8].
The majority of lung tumors in pediatrics correspond to metastases, generally from nephroblastoma, bone sarcomas and soft tissue sarcomas, especially rhabdomyosarcoma. Pulmonary metastases from thyroid carcinomas, malignant liver tumors, melanoma and teratocarcinoma are also cited [1,5,8].
MEDIASTINAL TUMORS
It is proposed that 40% of mediastinal masses in pediatrics correspond to malignant tumors. The anatomical location of the mass within the mediastinum suggests the origin of the lesion; posterior mediastinal tumors are frequently of neurogenic origin such as neuroblastoma or ganglioneuroma; Anterior mediastinal tumors are mostly lymphomas and in young children germ cell tumors such as teratomas. In the middle mediastinum the most common tumors are lymphomas and intracardiac tumors [1,4,9].
Depending on the imaging characteristics of the tumor and the presence of other systemic lesions, it is determined whether primary resection of the tumor is feasible or only a biopsy is appropriate [2,6,10].
The treatment of lung metastases depends on the histological type, size and location within the organ, preferring resection in nephroblastoma, osteosarcoma, hepatoblastoma and mesenchymal tumors. Resection via minimal access route (thoracoscopy) has very precise indications, but it would be a route to consider, mainly to make the diagnosis [1,9,11].
The diagnosis of germ cell tumors is based on the combination of imaging studies with elevated plasma levels of tumor markers such as alpha-fetoprotein and biopsy. Treatment is eminently surgical associated with systemic chemotherapy combined with Bleomycin, Etopoxide and Cisplatin [2,7]. On the other hand, histological analysis of the tumor with Immunohistochemistry shows positivity for Alpha-Fetoprotein (AFP) and Pan CK, with negativity for CK 7, CD30, WT1, HCG, OCT-4 and AME.
CASE PRESENTATION
Male patient, 3 years old at admission, white, from rural origin. With a history of good health, until mid-January 2023, which begins with pain in the lower limbs, scrotal edema and difficulty urinating. For this reason, he goes to the pediatric hospital in his native province, where he is admitted and urgently studied, detecting leukocytosis in the blood count and starting treatment with intravenous Ceftriaxone, interpreting the condition as urinary sepsis. When performing a simple anteroposterior and lateral abdominal x-ray, they detected a bladder balloon and opacity at the base of the right hemithorax. An anteroposterior chest x-ray was performed, confirming a radiopaque lesion that occupied the middle and lower third of the right lung.
Pre-surgical tumor markers are performed with a report of alpha feto protein greater than 1000IU/ml (elevated), B negative human chorionic gonadotropin, less than 0.10mIU/ml and LDH of 1098U/L (elevated). The family members decide to travel to the capital and they are urgently admitted to our hospital in February 2023 in the Oncosurgery service. Extension studies are quickly completed with:
Abdominal ultrasound: checking for the presence of a bladder balloon of more than 500 ml, liver, pancreas, gallbladder, spleen and both kidneys appearing normal. No ascites, no intra- abdominal lymph nodes.
Chest ultrasound: presence of an echogenic image of approximately 52mm x 66mm that is poorly defined in the middle and lower third projection of the right lung. Normal mediastinum, no bone alterations.
Contrast CT of the abdomen: presence of a hyperdense oval image in front of L5, with bone destruction of the vertebral body (wedge vertebra), giant bladder balloon.
Chest CT: Image of variable densities in the lower two thirds of the right lung, without calcifications. Slight linear spill on the base.
The case is discussed in a multidisciplinary team within the tumor committee in the presence of pediatricians, oncologists, radiologists, orthopedists and surgeons, taking as an initial agreement to bring to the room operations for spinal decompression at the level of L5 that caused urinary and defecatory sphincter disorders that The patient already presented, as well as motor disorders in the lower limbs. Studies with tumor markers with elevated alpha-fetoprotein 1000 mu/l are completed.
It is taken to the solon by the orthopedic team on Monday, February 13, 2023, decompression is performed at the level of the L4 and L5 lumbar spine, obtaining tissue for biopsy of the friable tumor of both soft tissue and bone. There were no postoperative complications, urination control gradually improved by stopping the bladder balloon and the sensation of the anal sphincter was recovered more slowly since he was experiencing severe constipation. But there was no recovery from the lower limb sensory disorders.
The tissue biopsy was not conclusive of the histological variant of malignant tumor in our center, it was decided to send it to the National Reference Center for Pathological Anatomy of the Hermanos Amejeiras Hospital.
While the result was in, it was discussed again in a multidisciplinary team since the patient worsened clinically, the right pleural effusion increased and the diameter of the right lung lesion increased. He also presented symptoms of a systemic inflammatory response, so he was admitted to intensive care. And is reported as critical.
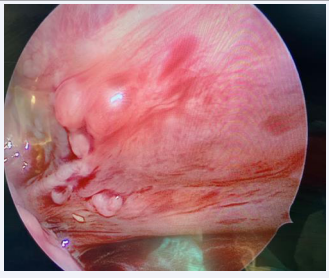
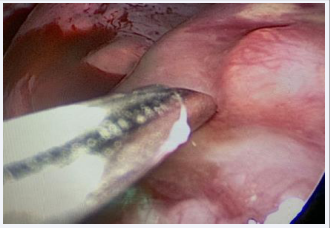
It was agreed in this discussion to perform Fine Needle Aspiration Biopsy (FNAB) of the right lung lesion under ultrasound control, which showed positive results for malignant cells, also with inflammatory elements, lymphocytes and nuclear polymorphism. The antibiotic therapy was changed to intravenous Vancomycin and Meronem and it was then decided to perform a biopsy of the lung tumor lesion, via thoracoscopy, which was performed in the operating room on February 27, 2023 (Figures A,B).
Figure A: Image showing the thoracoscopic view of the right lung tumor, with areas of necrosis.
Figure B: Image showing the thoracoscopic biopsy of the tumor.
March 1, 2023, result of the lung biopsy: malignant tumor composed of nests of clear cells, some with mucoproduction, formation of papillae and perivascular rosettes, cellular anaplasia, high mitotic index and abundant necrosis. The histological appearance is compatible with yolk sac tumor; it is
not can rule out the possibility of mixed germ cell tumor. Pending Immunohistochemistry to complete the histopathological study.
March 2, 2023- Result of the immunohistochemical study of the spinal canal lesion at the level of L5: bone metastasis of germ cell tumor with endodermal sinus pattern.
PANCK positive CK 7 focal positive
CD 117 focal positive Ki 67 positive 80% negative PLAP
Alpha-fetoprotein not evaluable Vimentin negative
CK 20 negative
P 63 negative
DC 30 negative
CD 99 negative
With these results studies are completed.
Medullogram: presence of the three series of bone marrow, not cells foreign to the medullary parenchyma.
Iliac crest bone marrow biopsy: not infiltrated, depressed
erythropoietic system.
He required preoperative transfusion due to hemoglobin levels of 7.0g/l.
It is agreed in a multidisciplinary team, given the extension of the disease at the onset of stage IV, due to the primary lung tumor with mediastinal infiltration and bone metastasis at the L5 level, to begin polychemotherapy with a BEP scheme (Bleomycin day 1, Cisplatin and Etopoxide for 5 consecutive days) obtaining. In the first cycle of treatment there was great clinical improvement.
The patient underwent six complete cycles of chemotherapy and presented disease progression. In August 2023, a pathological partial left femur fracture was detected. In the month of September, spontaneous consolidation of the fracture and appearance of new osteolytic lesions in the hip and right femur. He changed to another more intense chemotherapy regimen with VAC/IE (vincristine, cyclophosphamide and adriamycin on day 1 of the cycle and etoposide and ifosfamide starting on day 2 of the cycle for 5 consecutive days.
He presented cachexia, loss of appetite in the month of October, requiring the transfusion of positive B blood cells due to anemia of 7 g/l. It was decided to perform a new CT scan of the pelvis where the appearance of small osteolysis lesions was confirmed in both femoral heads, mainly on the left, the fracture was confirmed at that level and at the level of the spine. lumbosacral also osteolysis lesions (Figure C).
Figure C: Osteolytic lesions in femoral heads.
Upon admission in November, great clinical deterioration was observed, evident collateral circulation in the abdominal wall, with pain in both lower extremities and from a radiological point of view manifest worsening of the bone lesions (metastasis), ultrasound November 21, 2023 in In the proximal third of the left femur, a solid-looking lesion measuring 28 x 27 x 18 mm is observed, with irregularity and rupture of the cortex and involvement of soft tissues at the level of the surrounding area.
In the proximal third of the right femur, a cortical rupture and a similar homogeneous lesion of 18 x 8 mm were observed, and in the middle third, another smaller lesion of approximately 13 mm with a metastasic appearance was observed.
Progressive worsening of the patient with anemia of 7.5g/l, moderate leukopenia and moderate thrombocytopenia post chemotherapy. Clinically, increased volume of the upper third of both lower extremities, predominantly right, with local pain that prevents mobilization of the extremities.
In the month of December 2023, palliative care and pain relief begins, which is achieved with the use of tramadol, since pain control was not achieved with diclofenac, paracetamol and dipyrone.
The patient progressively worsened with an increase in osteolytic lesions and infiltration of soft tissues in the upper two thirds of both lower extremities, extreme cachexia and loss of appetite, with transfusion requirements with hemoglobin levels of 6 grams. He died on January 16, 2024 with great clinical deterioration, generalized edema and multiple organ failure.
DISCUSSION
It is suggested in the literature that endodermal sinus tumor (yolk sac tumor) generally affects the ovaries or testicles and the lower part of the spine. Growing rapidly and infiltrating other tissues. It has a high degree of malignancy [1,3,11].
Teratoma is the most common germ cell tumor in pediatrics. The etiology of these tumors is unknown; it is suggested that their appearance may be associated with certain syndromes such as Turner syndrome and Klinefelter syndrome. Children with cryptorchidism are also at risk of developing testicular teratomas [1-3].
Nakhla and collaborators [10] present a case similar to ours but in an adult patient, who responded to the same cytostatic treatment regimen with the BEP chemotherapy scheme (Bleomycin, Etoposide and Cisplatin) and others report the VIP chemotherapy scheme (etoposide, Ifosfamide and Cisplatin), achieving post-chemotherapy tumor surgery [2,4].
The most common symptoms are: abdominal and chest pain, respiratory difficulty, cough, isolated and intermittent fever, pain at the lumbar spine, urinary disorders (frequency, urination pain, urinary retention and defecatory disorders, mainly constipation, as occurred in our patient. Anorexia may be present and there may even be increased body hair growth [1,2,11].
Other symptoms in girls: vaginal bleeding or amenorrhea,signs of precocious puberty, short stature, nausea and vomiting [2,5,7].
AFP has an important role not only in the diagnosis of yolk sac tumor, which increases its serum concentrations in 90% of cases,1 but also as a follow-up marker to identify tumor recurrence or metastasis [1,5,6]. AFP can be elevated due to other causes such as some inflammatory liver diseases (cirrhosis, hepatocellular carcinoma and some gastrointestinal tumors).
Elevated AFP levels in the child should be interpreted with caution as they may correspond to normal physiological elevations, for example, AFP levels at birth are approximately 50,000 ng/mL, they are reduced to 10,000 ng/mL at birth. 2 weeks, 300 ng/mL at 2 months, and 12 ng/mL at 6 months,1,2 so AFP must be monitored to differentiate it from residual disease [1].
In the diagnosis of yolk sac tumor, imaging studies are required that include ultrasound, Computed Tomography (CT) of the chest and abdomen to evaluate the retroperitoneum and stage the oncological process. In addition, a chest x-ray must be performed to evaluate possible lung metastases [1-3].
There are few cases reported in the literature of yolk sac tumor in the lung. Hernández Benedicto R, et al. [2] published a case of a 23-year-old male patient with a history of bronchial asthma who attended the emergency room with dry and frequent cough, weight loss of 7 kg in one month, and a fever of 38o C for two days. After analytical studies, chest x-ray, lung computed tomography and histological study, it was concluded that a primitive extra-gonadal germ cell neoplasia of the anterior mediastinum turned out to be a seminoma. Being necessary to differentiate it from other tumors such as: aortic aneurysm, bronchogenic cyst, choriocarcinoma, cystic hygroma, embryonal carcinoma, lymphomas, thymoma, endothoracic goiter [1,2,11].
The anterior mediastinal germ cell tumor originates from congenital defects in the embryonic stage due to migration of the primordial germ cell and is derived from cells that are within the gonads (germinal), they can migrate and be located outside of these (extra gonadal). like the case we present, and be located in the anterior mediastinum with or without lung infiltration. The most reported location of extra gonadal tumors is in the anterior mediastinum [2,10,11,12].
Its origin in the prostate in pediatrics is extremely rare; most reports of this tumor variant are in adult patients. There are reports of these tumors in the thymic and pineal gland [4,5,7,12].
It is suggested that in addition to chemotherapy and surgery, there is a good response to treatment with radiotherapy, which has been shown to increase survival in these patients [1,3,5,12].
REFERENCES
- Marrero AE, Pérez JMH, Chesa MV, Llanos JMD. Extensive pulmonary involvement as a presentation of an ovarian yolk sac tumor. Open Respir Arch. 2022; 4: 100156.
- Hernández-Benedicto R, Pile R, Rosales P. Cell germ primary tumor of mediastinum (seminoma of mediastinum) Medical Archive Camagüey. 2019; 23.
- Busch J, Seidel C, Zengerling F. Male extragonadal germ cell tumors of the adult. Oncol Res Treat. 2016; 39: 140-144.
- Velazco CN, Mallea JC. Sac tumor of the testicle in pediatrics:presentation of a case. Rev Med Peace. 2022; 28.
- Cao J, Zhou Y, Zou F, Ma JA, Hu C. Intensity modulated radiation therapy to treat primary female mediastinal seminoma and massive pericardial effusion: A case report. Oncol Lett. 2017; 13: 1299-1302.
- Zheng W, Wang L, Yang D, Fang K, Chen X, Wang X, et al. Primary extragonadal germ cell tumor: A case report on prostate seminoma. Oncol Lett. 2015; 10: 2323-2326.
- Weissferdt A, Rodríguez Canales J, Liu H, Fujimoto J, Wistuba II, Moran CA. Primary mediastinal seminomas: A comprehensive im- munohistochemical study with a focus on novel markers. Hum Pathol. 2015; 46: 376-383.
- Chahoud J, Zhang M, Shah A, Lin SH, Pisters LL, TuS M. Managing seminomatous and nonseminomatous germ cell tumors. Curr Opinion Oncol. 2018; 30: 181-188.
- Segura Guevara JM, Peña MM, Molina VN. Sinergia Medical Magazine. 2019; 4: 108-113.
- Nakhla SG, Sundararajan S. A rare case of primary anterior mediastinal yolk sac tumor in an elderly adult male. Case Rep Oncol Med. 2016; 2016: 8961486.
- Ramirez Gil ME, Martinez PV, Menal MP, Hernandez F, Muñoz GG, Rivas JJ. Pulmonary pure yolk-sac tumor. A Rare Anatomopathological Entity. Arch Bronconeumol. 2011; 47: 157-158.
- Jing X, Jinglan Z, Shaoqing G, Qi W, Pengfei W, Chunling Z, et al. Primary seminoma arising in the middle mediastinum: A case report. Oncol Lett. 2016; 12: 348-350.