A Novel Bioabsorbable Sleeve for Staple Line Reinforcement in Laparoscopic Sleeve Gastrectomy (LSG) For Morbid Obesity: Possible Usefulness for the Future Application in Operations for Alimentary Tract Cancers
- 1. Department of Digestive Surgery, Kyoto Prefectural University of Medicine, Japan
- 2. Doshisha University, Faculty of Life and Medical Sciences, Graduate School of Life and Medical Sciences, Japan
ABSTRACT
Laparoscopic sleeve gastrectomy (LSG) for morbid obesity is showing increased uptake worldwide. However, gastric wall weakness due to lipid sedimentation in cases of morbid obesity can lead to bleeding and leakage from the gastric stump, which is a major postoperative complication. We describe herein our experience using a new bioabsorbable polyglycolic acid (PGA) sleeve in six patients to provide staple line reinforcement in LSG for morbid obesity, as well as a comparison with suture reinforcement.
The PGA sleeve can be easily equipped with the Endo GIA™ linear stapling device. The use of PGA sleeve produced less bleeding from the gastric stump than suture reinforcement, with notably shorter operative time because there was no need to suture the staple line. The postoperative course was uneventful for all patients.
The use of a PGA sleeve in LSG for morbid obesity is a safe, timesaving procedure that results in minimal bleeding and negates the need to suture the staple line. The PGA sleeve is an appealing alternative to suturing for staple line reinforcement. This bioabsorbable sleeve may also be applicable for the staple line reinforcement in operations for alimentary tract cancers for the decrease of blood loss and shorter operative time.
KEYWORDS
• LSG
• Staple line reinforcement
• PGA sleeves
CITATION
Sakakura C, Ozamoto Y, Togawa T, Hagiwara A, Otsuji E, et al. (2013) A Novel Bioabsorbable Sleeve for Staple Line Reinforcement in Laparoscopic Sleeve Gastrectomy (LSG) For Morbid Obesity: Possible Usefulness for the Future Application in Operations for Alimentary Tract Cancers. JSM Clin Oncol Res 1(1): 1003.
ABBREVIATIONS
PGA: polyglycolic acid; LSG; laparoscopic sleeve gastrectomy
INTRODUCTION
Metabolic surgeries for obesity, such as laparoscopic sleeve gastrectomy (LSG), are now widely practiced and increasing in prevalence [1,2]. However, morbidly obese patients, often have comorbidities such as diabetes and atherosclerosis, which may predispose them to an increased risk of surgical complications. A particularly challenging complication after LSG is postoperative bleeding and leakage, which causes increased morbidity and hospital stay. Continuous suturing on the staple lines is commonly employed to reduce the probability of bleeding and leakage; however, this can be time consuming and technically difficult in many cases. A variety of other techniques have also been applied to reinforce the staple line [3,4]. The purpose of this randomized study was to compare LSG reinforced with a polyglycolic acid (PGA) sheet versus staple line 3-0 vicryl suturing.
PATIENTS AND METHODS
Between 2010 and 2013, 13 patients received either a PGA sleeve (Gunze, Ayabe, Japan; n = 6) or interrupted sutures (n = 7) for staple line reinforcement during LSG. The Endo GIA™ 60 mm automatic linear stapling device (U. S. Surgical Corp, Norwalk, CT, USA) was used for all cases. The PGA sleeve was incorporated into a dispensable sheath for easy application according to the method of Cooper [5]. The linear stapler was applied five or six times during each LSG. Parallel staple lines were used wherever possible; however, staple lines did intersect on a few occasions. Where staple lines did cross, additional sutures were used at the join with the PGA sheet. As there was no significant difference in the mean total operation time between the PGA sleeve and suture reinforced groups, the procedure times to excise the greater curvature of the stomach in each group was compared.
RESULTS
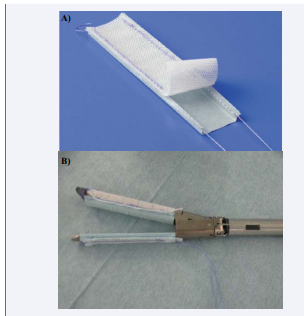
A macroscopic view of the PGA sleeve is shown in Figure 1.
Figure 1: A macroscopic view of the PGA sleeve. Panel A: The PGA sheet is fixed to an expandable nylon mesh sheet with 3-0 vicryl. Panel B. The Endo GIA stapler is covered with a PGA sleeve.
The PGA sheet was fixed to an expandable nylon mesh sheet with 3-0 vicryl, which was subsequently removed from the abdominal cavity using the 3-0 vicryl after stapling with the Endo GIA device.
Typical views of the surgical margins reinforced with or without the PGA sheet are shown in Figure 2.
Figure 2: The stump of the sleeve gastrectomy was reinforced by a PGA sleeve at the time of stapling. Oozing was noted along the staple line but there was no bleeding where the staple line is reinforced with PGA sleeve.
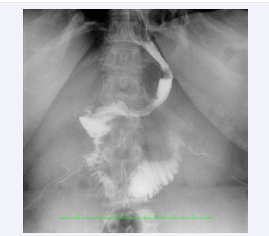
Although oozing may have been present along the staple lines, there was no bleeding associated with the PGA sheet. There was no abnormal form in resulting sleeved stomach and contrast medium passed through the sleeved stomach without leakage, as shown in Figure 3.
Figure 3: Contrast medium passed through the sleeved stomach without leakage after LSG.
The mean percentage of excess weight loss (%EWL) was 53.6% and 57.6% at 12months. There was no surgical complication in each group. There were no conversions due to massive bleeding. Comorbidities improved or resolved in most patients, including arterial hypertension (83.3%) and diabetes mellitus (85.7%). As we can omit suturing by using PGA sleeve, the time to excise the greater curvature of the stomach was significantly reduced in the PGA sleeve group (Table 1).
Table 1: Clinicopathological features of patients treated undergoing LSG.
|
|
PGA sheet (n=6) |
Sutures (n=7) |
Statistical analysis??? |
|
Age |
31−49 (39.4) |
28−55 (44) |
n. s. |
|
BMI |
36.2−72 (52.6) |
38.6−57.2 (52.8) |
n. s. |
|
**Time (min) |
27-44 ( 34.6 ) |
40-66 ( 52.8 ) |
*p < 0.05 |
|
Blood loss (ml) |
21-113 ( 64.3 ) |
32-151 ( 67.7 ) |
n. s. |
**Time is calculated as procedure time to excise the greater curvature with or without interrupted sutures.
However, there was no significant difference in total operation time (data not shown). The total blood loss also decreased in this group, but the difference was not significant.
DISCUSSION
Implantable devices made from biodegradable materials are widely used to repair tissues or reinforce fragile tissues [6]. PGA has been widely used as a suture and sheet material. PGA sheets have been successfully applied in pulmonary wedge resection of the emphysematous lung and pancreas tail resection. To our knowledge, this is the first clinical report on a bioabsorbable PGA sleeve for staple line reinforcement in LSG. The bioabsorbable PGA sleeve is less expensive than non-absorbable materials for staple line reinforcement and is a promising candidate material for use in LSG.
The most frequent and troublesome complications after LSG are postoperative bleeding and leakage [7,8,9], which increase morbidity and hospital stay. The likelihood of these complications increases in morbidly obese patients because the gastric wall is weak due to lipid sedimentation. For these patients, we recommend the use of a tall stapler and reinforcement with a PGA sheet to prevent bleeding and/or splitting of the gastric wall. We also noted few operative complications in our series of patients. There was less bleeding from the gastric stump when a PGA sheet was used (although not statistically significant) and the operative time was significantly less than that of a conventional procedure (application of a continuous or interrupted suture). The PGA sleeve can be easily equipped with the Endo GIA linear stapling device and the procedure can be regarded as safe and straightforward. The postoperative course of all patients was uneventful.
Previous reports have indicated that care should be taken to avoid excessive rotation of the stapler when a PGA sleeve is used for staple line reinforcement [6]. Therefore, we always employ gastric endoscopy just before stapling, and staples are placed in parallel lines wherever possible. The biological behavior of PGA sheet has not yet been fully clarified; however, animal models of the lung have demonstrated that it gradually degrades in a time dependent manner [6]. The use of a PGA sleeve did not show evidence of leakage in our series (Figure 3).
In conclusion, the use of a PGA sleeve in LSG for morbid obesity is a safe, timesaving procedure that causes minimal bleeding and negates the need to suture the staple line. The PGA sleeve is an appealing alternative to suturing for staple line reinforcement, which may also be applicable for the resection of the pancreas as well as resection of the duodenum in laparoscopy-assisted Billroth-I gastrectomy. The results of our study are limited by the small sample size and warrant further investigation in a larger patient series. This bioabsorbable sleeve may also be applicable for the staple line reinforcement in operations for alimentary tract cancers for the decrease of blood loss and shorter operative time.
Table 1: Clinicopathological features of patients treated undergoing LSG.
| PGA sheet (n=6) | Sutures (n=7) | Statistical analysis | |
| Age | 31−49 (39.4) | 28−55 (44) | n. s |
| BMI | 36.2−72 (52.6) | 38.6−57.2 (52.8) | n. s |
| **Time (min) | 27-44 ( 34.6 ) | 40-66 ( 52.8 ) | *p < 0.05 |
| Blood loss (ml) | 21-113 ( 64.3 ) | 32-151 ( 67.7 ) | n. s |