Isolated Unilateral Optic Nerve Infiltration in Childhood Acute Lymphoblastic Leukemia
- 1. Department of Cellular Biotechnologies and Hematology, Sapienza University of Rome, Italy
- 2. Department of Ophtalmology Unit, Sapienza University of Rome, Italy
- 3. Department of Radiology, Sapienza University of Rome, Italy
- 4. Department of Ophtalmology, Sapienza University of Rome, Italy
Abstract
Isolated optic nerve involvement is rarely reported as an initial site of relapse after complete systemic remission of childhood acute lymphoblastic leukemia. In such cases, a full ophthalmologist exploration, radiologic investigations and a complete disease evaluation including cerebral spinal fluid and bone marrow studies with molecular evaluation of minimal residual disease have to be immediately performed for confirming the diagnosis of relapse and ensuing early treatment. The prognosis is usually poor and there is no consensus on the optimal management of such rare cases. More controversial is the treatment of patients with no detectable overt leukemia and suspected optic nerve leukemic infiltration.
Keywords
• CNS relapse
• Lymphoblastic leukemia
• ALL relapse
• Optic nerve
• Isolated nerve infiltration
Citation
De Benedittis D, Chisini M, Moleti ML, Plateroti R, Gualdi G, et al. (2016) Isolated Unilateral Optic Nerve Infiltration in Childhood Acute Lymphoblastic Leukemia. JSM Clin Oncol Res 4(1): 1047.
ABBREVIATIONS
ALL: Acute Lymphoblastic Leukemia; CNS: Central Nervous System; i.t.: Intrathecal; CR: Complete Remission; WBC: White Blood Cells; AIEOP: Associazione Italiana Ematologia e Oncologia Pediatrica; CSF: Cerebrospinal Fluid; BM: Bone Marrow; MRI: Magnetic Resonance Imaging; VA: Visual Acuity; CMV: Cytomegalovirus; EBV: Epstein-Barr virus; HHV-6: Human Herpes Virus 6; HSV1, HSV2: Herpes Simplex Virus 1 and 2; VZV: Varicella-Zoster Virus; BKV: Polyoma Virus BK; JCV: Papova Virus JC; OCT: Optical Coherence Tomography; BFM: Berlin-Frankfurt-Munster.
INTRODUCTION
With modern chemotherapy, Acute lymphoblastic leukemia (ALL), the most common childhood cancer, is cured in over 80% of cases [1]. Reports of central nervous system (CNS) relapse in childhood ALL are becoming less frequent nowadays because of improved CNS-directed systemic and intrathecal i.t. therapy [2,3]. Isolated optic nerve involvement is even more rare and usually associated with poor outcome, even though prompt and intensive chemo-radio-therapy is immediately started [4-10].
Here we describe a 12-year-old patient who developed an isolated left sided optical nerve relapse during maintenance therapy for T-cell ALL in absence of systemic and meningeal leukemic infiltration; overt bone marrow (BM) and cerebrospinal fluid (CSF) leukemia occurred only 4 months later.
CASE PRESENTATION
A 12-year-old male with T-cell ALL in first complete remission (CR), at the start of maintenance phase, presented itchiness in both eyes. His previous hematological history was as follows: he received diagnosis of T-cell ALL 16 months earlier; he showed hyperleukocytosis (white blood cells (WBC) 78.8 x 103 /μl) at disease presentation without CNS involvement. He was enrolled in the Associazione Italiana Ematologia e Oncologia pediatrica (AIEOP) ALL 2009 protocol, high-risk arm (T-cell ALL + prednisone poor responder); he achieved a CR at day +33 (end of Phase IA) and continued Phase IB, intensive consolidation (3 blocks of polichemotherapy) and three reinduction courses without major complications. Prophylactic i.t. therapy was administered during all protocol phases and CSF examination was carried out prior to each i.t. drug instillation and never showed CNS disease. Fifteen days prior to the occurrence of ocular symptoms, he had received i.t. methotrexate, with a negative CSF, and performed a BM aspiration which confirmed the CR status, both morphologically and by flow cytometry. A funduscopy revealed tinge of the left edge of papilla; an orbit and brain magnetic resonance imaging (MRI) revealed no space occupying lesion or hydrocephalus; a left sided optic disc edema and peripapillary nerve fiber layer edema were detected.
An electroretinogram test and visual evoked potentials were normal in both eyes; CSF was normal at morphologic and immunophenotypic studies and showed a normal blood brain barrier. BM was repeated and no disease was detected at molecular level (real-time quantitative polymerase chain reaction for T cell receptor.
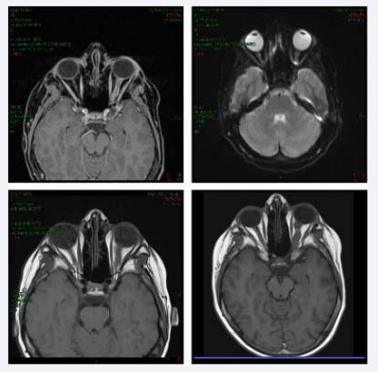
A few days later, because of the worsening of the visual acuity (VA), an orbit MRI was repeated and the left nerve edema proved unchanged but showed an increased perineural impregnation of contrast medium (Figure 1).
Figure 1 Brain MRI - Sequential magnetic resonance imaging showing enhancement along the left optic nerve.
BM and CSF examinations once again confirmed the CR status. CSF viral studies (CMV, EBV, HHV-6, HSV1, HSV2, VZV, BKV, JCV) were performed and proved negative. Based on the ophthalmologist’s suggestion, the patient received intravenous methylprednisolone (1 g/day). Two weeks later a MRI was repeated and documented an increase of left intra-orbital optic nerve perineural edema (4.2 mm vs 2.5 mm at the previous MRI).
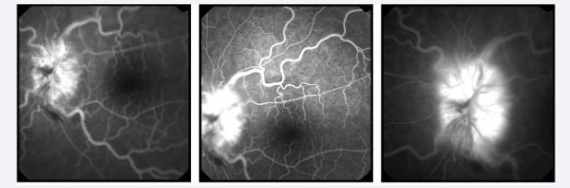
A fluorescein retinal angiography showed late fluorescence of left optic disc with blurring of its margins (Figure 2).
Figure 2
Figure 2 Left optic nerve fluorangiography - Left optic disc fluorescence increasing in the late stages.
Anti-edema treatment with dexamethasone and an osmotic diuretic was carried out; this was followed by a small reduction of the optic nerve perineural hyperintensity at MRI.
Given the lack of clinical improvement and negativity of all hematologic studies, but suspecting isolated optic nerve disease recurrence, i.t. chemotherapy was administered without any success. CSF was negative; BM molecular study again confirmed the CR. Neuro-ophthalmologic examination described peripapillary edema with exudates and perivascular hemorrhages in the left eye, strongly suggestive to be secondary to infiltrative disease of the optic nerve meningeal sheaths. CSF examination was again negative for morphological, immunophenotypic, infectious studies and for galattomannan search.
With a strong suspect of optic nerve leukemia recurrence, even without documented evidence of leukemic infiltration, the patient received high-dose chemotherapy (-cytarabine 3g/ m2 /12 hours x 6 doses) with i.t cytarabine that preceded and followed systemic treatment. This strategy resulted in a slight VA improvement. This was confirmed at an optical coherence tomography (OCT) of the left optic nerve that showed a decreasing of the thickening and perimacular edema.
One month later from beginning chemotherapy, the patient showed a worsening of the vision; a MRI revealed an increase thickness of the left optic nerve, while the CSF and BM continued to be negative for disease recurrence.
Whole-brain radiotherapy was initiated and an improvement in VA was reported after the first few sessions. During radiation treatment, four months after the initial symptoms, the CSF revealed 73% of leukemic cells. A BM aspirate showed no evidence of leukemia. The patient received i.t. chemotherapy (methotrexate) and completed the planned radiotherapy. At the end of cranial radiation the CSF was clear but the BM showed 27% of leukemic cells with the same immunophenotypic profile of diagnosis.
Systemic chemotherapy with cyclophosphamide, etoposide and nelarabine resulted in a perfect recovery of the left eye sight, but the patient failed to achieve a BM CR; he died ten months later, due to disease progression.
DISCUSSION
Since the introduction of BFM-like protocols for the treatment of childhood ALL, the incidence of isolated or combined CNS relapse significantly decreased and unilateral optic nerve infiltration as an initial site of relapse in first ALL remission, is a very rare manifestation [4,5,7,8,11]. In CR patients with a decreased VA, other causes - such as infection, vasculitis, radiation optic neuropathy or chemotherapy side effects - have to be evaluated [8,12]. In our patient, in first CR for 16 months, who had recently received i.t. chemotherapy, a loss of VA was initially referred to i.t. drug-related toxicity. Indeed, BM and CSF exams excluded the presence of minimal residual disease. Systemic steroid treatment and osmotic diuretics, administered in an attempt to decrease optic nerve swelling, resulted only in temporary benefit.
Rare cases of childhood leukemia recurrence with optic nerve infiltration have been reported in the literature (Table 1); BM and/or CSF examinations usually show leukemic infiltration confirming the relapse. Optic nerve infiltration is usually bilateral (4/6 patients) and associated with CSF leukemia (5/6 cases) [4-7,13,14]. In such cases, immediate intravenous and i.t. chemotherapy as well as high-dose intravenous methylprednisolone, with or without radiotherapy, usually reduce optic nerve swelling and improve VA. Despite aggressive treatment the prognosis is poor [4,9]. The mechanisms underlying optic nerve swelling are not fully understood, but the obstruction of the venous outflow by perivascular leukemic cells and the elevated inducible nitric oxide synthase levels with toxic effect on the neural tissue may have a role in optic damage [15]. The optic nerve passes through small bony space where leukemic cells can create anatomic barrier to CSF flow. For this reason, cytotoxic drugs may be unable to reach the affected nerve and the prognosis of visual recovery is poor. In our patient, the progressive worsening of ocular symptoms, in the absence of evidence of leukemia even at the molecular level, forced us to start systemic high-dose chemotherapy, followed by cranial radiotherapy. Both procedures, performed also in an attempt to avoid irreversible optic nerve damage, resulted in a complete recovery of left eye sight, but unfortunately were not able to avoid disease progression.
This case underlines the importance of optic nerve infiltration as a site of leukemia recurrence; the rarity of this entity in the literature, may be due to unreported cases and optic nerve leukemic infiltration should always be kept in mind in high-risk patients and/or those with T-cell ALL. It also underlines the difficulty in early diagnosis and management of patients not showing signs of leukemia. In such cases, the accurate ophthalmologist examination revealing monolateral peripapillary edema with VA preserved, not responding to steroid treatment and in the absence of MRI space occupying lesion or hydrocephalus, can strongly suggest early diagnosis of optic nerve leukemic infiltration.