Spinal Myeloid Sarcoma Presenting as Paraplegia: A Case Report
- 1. Department of Clinical Oncology, Jinnah Postgraduate Medical Center, Pakistan
Abstract
Objective: Myeloid sarcoma comprising of immature granulocytic cells is a rare, extra medullary tumor. Spinal cord compression caused by a myeloid sarcoma is even more so. This study reports a case of spinal myeloid sarcoma presenting with paraplegia.
Patient and method: 18-year-old male presented with progressively worsening back pain leading to paraplegia. Magnetic resonance imaging (MRI) dorsal spine revealed a soft tissue mass extending from D4 through D8 causing compression of cord in mid dorsal region. The patient underwent surgical decompression. Histology confirmed the diagnosis of myeloid sarcoma. Post operatively bone marrow biopsy showed no evidence of myeloproliferative neoplasm. The patient then received systemic chemotherapy in line of Acute Myeloid Leukemia (AML).
Result: After 9 months patient reports complete relief of symptoms. Post treatment MRI shows no evidence of compressive or residual disease.
Conclusion: Spinal myeloid sarcoma presenting as paraplegia is very rare. We suggest that clinical suspicion can lead to early diagnosis and appropriate management.
Keywords
- Myeloid sarcoma
- Myeloid leukemia
- Spinal tumor
- Paraplegia
Citation
Nouman M, Shaikh M, Haider G, Meher K (2019) Spinal Myeloid Sarcoma Presenting as Paraplegia: A Case Report. JSM Clin Oncol Res 7(1): 1061.
INTRODUCTION
Myeloid sarcoma or chloroma comprising of immature granulocytic cells is a rare, extramedullary tumor. It may be seen in the setting of acute or chronic leukemia or myeloproliferative disorders but seldom reported in otherwise healthy patients without any evidence of systemic disease [1]. Spinal epidural myeloid sarcoma is uncommon, and spinal cord compression caused by a myeloid sarcoma is even more so[2]. This study reports a rare case of spinal myeloid sarcoma presenting as paraplegia. It was treated successfully with surgical decompression of spinal cord followed by chemotherapy.
CASE PRESENTATION
An 18-year-old male presented to us with progressively worsening back pain for the past 18 months. It was dull and continuous, not radiating. There were no predisposing factors like trauma. Initially he consulted a local medical practitioner and received systemic and local analgesics along with muscle relaxants. In spite of these measures, his pain continued to increase over the time and eventually led to paraplegia.
Following this, the patient consulted a neurosurgeon who referred him for imaging of the spine.
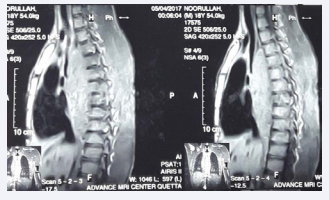
MRI dorsal spine with contrast revealed large enhancing extradural soft tissue mass extending from D4 through D8 with intra the cal extension causing compression of cord in mid dorsal region. It was predominantly on the right side with extension in the right paraspinal muscles with cranio-caudal extension of about 10.2cm (Figure 1).
Figure 1 Showing an enhancing extradural soft tissue mass extending from D4 through D8.
Keeping in view the worsening of symptoms and paraplegia, he underwent excisional biopsy of dorsal spinal mass, laminectomy and decompression.
Following surgical decompression, he underwent radiation therapy of the spinal cord for cord compression; total dose of 30Gy.
Histopathology revealed a neoplastic lesion comprising of intermediate to large sized cells arranged in sheets with background showing abundant eosinophil infiltrate. These cells stained positive for LCA, MPO, CD 68, CD 117 with increased Ki-67 proliferative index. It was negative for Pan B (CD 20/ 79a), Pan T (CD 3), Tdt, CD 30, CD 138 and PAX 5. These immunohistochemical findings were consistent with the diagnosis of myeloid sarcoma.
The patient was referred to us in Medical Oncology for further management. We carried out thorough history and physical examination. Karyotyping showed normal cytogenetics. We did bone marrow biopsy to rule out myeloid sarcoma associated with Acute Myeloid Leukemia (AML). It showed no evidence of bone marrow involvement with myeloproliferative disorder.
The patient underwent “3+7” induction chemotherapy with daunorubicinand cytarabine followed by four cycles of consolidation with high dose cytarabine.
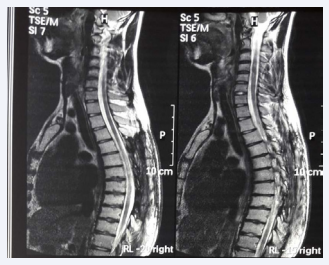
Post consolidation MRI of the dorsal spine with contrast revealed complete response to treatment with no residual disease. It shows post-surgical changes with evidence of laminectomy from D2 to D8 (Figure 2).
Figure 2 Showing laminectomy with complete resolution of mass.
The patient reports complete resolution of symptoms with ability to walk and perform daily activities. He is disease and symptom free on follow up of one year.
DISCUSSION
A myeloid sarcoma also known as chloroma or granulocytic sarcoma is a rare, extra medullary myeloid tumor. It is a solid tumor composed of immature granulocytes [3]. It is a rare hematologic phenomenon in patients with AML with an incidence as low as 2.5 to 9.1% [1, 4].It may occur during the course or just preceding or following leukemia [1,4].
Myeloid sarcoma has a predilection for males (male-to-female ratio, 1.2:1) [5,6].
Sites commonly involved include the skin, lymph nodes, gastrointestinal tract, bone, soft tissue, and testis.[7,8] However, spinal cord involvement is even less than 1 percent [9].
Spinal myeloid sarcoma may present with varied symptoms depending upon the site. Those with involvement of para-spinal muscles may lead to spinal cord compression due to mass effect [2]. In the case presented here, patient initially reported progressively increasing back pain that eventually led to paraplegia.
Spinal myeloid sarcoma is often challenging to diagnose because the clinical data and imaging is usually nonspecific. It often appears as a soft tissue mass on computed tomography or MRI that does not point to a specific diagnosis [2,9]. Hence, it is crucial to obtain a tissue biopsy to formulate a diagnosis of myeloid sarcoma. Following this, immunohistochemistry and a series of markers is a practical guide that aids in the diagnosis and further characterization of the tumor [10].
In this case, the patient underwent excisional biopsy of the dorsal spinal mass, laminectomy, and cord decompression. Immunohistochemical stains showed positive staining with LCA, MPO, CD 68, CD 117 with increased Ki-67 proliferative index which helped to confirm the diagnosis as these are the most commonly expressed markers of myeloid differentiation[11].
Given the rare incidence of spinal myeloid sarcoma, the clinical suspicion of the disease should be kept high so that the treatment can start at optimal timing. Possible treatment strategies include chemotherapy, hematopoietic stem cell transplantation (HSCT), radiotherapy and surgery. Literature reveals large randomized studies, which assessed the prognosis of isolated myeloid sarcoma. Systemic chemotherapy used in the treatment of AML remains the best strategy for treating this set of patients, but the optimal timing remains controversial [13,15-17]. Surgery is however limited to the cases with symptomatic compression due to the tumor [12]. We reviewed cases of spinal myeloid sarcoma presenting with cord compression from the literature (Table 1), [18-26]. Surgical excision of the tumor appeared to be the first treatment option in these cases.
In our case, patient underwent surgery for decompression followed by systemic chemotherapy that led to complete response.
Inoue et al identified 26 patients of myeloid sarcoma from the literature who had no evidence of myeloid leukemia, and it was found that the treatment strategy varied from individual to individual [14]. Surgical decompression was performed in 22 patients, and 21 of the patients received additional AML-type systemic treatment. However, the outcome of the patients varied and was poor in those who showed progression to leukemia. Overall, prompt diagnosis and adequate treatment are critical to achieve a better outcome.
CONCLUSION
Spinal myeloid sarcoma presenting as paraplegia is very rare. Clinical suspicion of the disease can lead to early diagnosis and appropriate management. Keeping in view our patient and previous cases from literature, we suggest that prompt diagnosis followed by emergency decompression and intensive chemotherapy in the line of management of AML can lead to complete recovery objectively and clinically and can prevent neurological damage.
Table 1:
| No. | Reference | Age/ Gender | Diagnosis and IHC | Site / Extent | Signs and symptoms | Treatment | Outcome |
| 1 | Amalraj et. Al [18] | 4/M | Granulocytic sarcoma promyelocytic leukemia AML M3 | T3-T10 | *Acute paraplegia *Weakness of both lower limbs *Numbness of both lower limbs *Back pain |
radiotherapy and chemotherapy | Paraplegia improved |
| 2 | Olcay et al. 2009 [19] | 12/M | Acute myeloid leukemia CD45:95.15%, CD15: 35.56%, CD33:77.57%, CD117:79.3%, CD34:43.38%, CD13:29.32 %. |
*Lumbar (L3) -Conus medullaris *Left maxillary mass |
Conus medullaris syndrome | *Chemotherapy + triple intratecal therapy *Radiotherapy | Symptom partially resolved died because of pneumonia and disseminated intravascular coagulation |
| 3 | Yin et al. 2010 [20] | 28/M | myeloid sarcoma with acute myeloid leukemia CD68, CD45, CD43, CD117 and lysozyme but not of MPO, CD20 | T12-L1 | *low back pain *numbness of his legs *bladder incontinence *hypoesthesia below T12 paraparesis |
High-dose methyl-prednisolone Decompression with T12-L1 laminectomy and tumor resection. | Paraparesis Improvement |
| 4 | Bittencourt et al. 2011[21] | 53/M | *Acute promyelocytic leukemia presenting as extradural mass *PCR for the PML-RARα gene was positive | T6-T8 | *Progressive fatigue, pain legs weakness Paraparesis *Gingival hemorrhage, hepatomegaly |
*delais 4 months/ chemotherapy (daunorubicin) *Radiotherapy |
/Evolution: no neurologic improvement + died of sepsis |
| 5 | Kyaw et al. 2012[22] | 26/M | Myeloid sarcoma: acute promyelocytic leukemia CD33, CD117, CD64, CD34 and cytoplasmic MPO were presented Reverse transcriptase-polymerase chain reaction showed BCR1-type PML-RARα fusion copies | T2-T4 and T12 – L2 | Progressive back pain and bilateral leg weakness: -paraparesis Loss of pain and sensory perception | *Radiotherapy *Chemotherapy: retinoic acid + ida rubicin |
*Neurological improvement -Good remission |
| 6 | Ben et al. 2013 [23] | 21/M | *chloroma *positive for myeloperoxidase *acute myeloblasti cleukaemia (AML |
T4/ T7, T1-T2 | Progressive paraplegia. urinary retention | *laminectomy + tumour was totally removed. *rubidomycine (45 mg/m2 daily for 3 days) and cytosine arabinoside (200 mg/ mm2continuous infusion for 7 days) |
improvement paraplegia |
| 7 | Krishna murthy et al. 2014 [24] | 16 /M | Granulocytic sarcoma associated with acute myeloblasticleukaemia (AML) | Low backaches follow proptosis, spinal cord causing significant compression of the spinal cord. | -radiotherapy and chemotherapy | ||
| 8 | Joseph JR 2015 [25] | 20/M | Myeloid sarcoma associated with AML | acute onset weakness and numbness in his lower extremities | *Radiation *surgical decompression |
Worsening of symptoms | |
| 9 | Hyun Ho Oh 2016 [26 | 66/M | Myeloid Sarcoma | T12-L2 | *Progressive back pain *Numbness in lower extremities |
*Dexamethasone *Radiation chemotherapy with daunorubucin and cytarabine |
Partial improvement in symptoms |