Synchronous Quiescent Pulmonary Metastasis from Clear Renal Cell Carcinoma Activated after 18 Years
- 1. Department of General Thoracic Surgery, Catholic University of the Sacred Heart, Italy
- 2. Division of Thoracic Surgery, European Institute of Oncology, Italy
Abstract
We herein report a case of a pulmonary metastasis from renal cell carcinoma suspended in quiescent state for 18 years. At the time of renal cancer diagnosis, the patient already had some nodules in both lungs, so he underwent CT-scan follow-up of the suspect nodules for 5 years, and only a CT-scan done for other reasons after 18 years showed increase in dimension. Therefore the patient was subjected to atypical resection of the right nodules sprung up. Pathologic analysis was compatible with metastases from the primitive renal cell carcinoma. Pulmonary nodules were present at the time of diagnosis of renal cancer, but for 18 years they didn’t show any type of growth or modifications.
Keywords
• Lung
• Metastasis
• Clear renal cell carcinoma
• Delayed surgery
Citation
Chiappetta M, Novellis P, Nachira D, Petracca CL, Margaritora S, et al. (2016) Synchronous Quiescent Pulmonary Metastasis from Clear Renal Cell Carcinoma Activated after 18 Years. JSM Clin Oncol Res 4(1): 1046.
ABBREVIATIONS
CT: Computed Tomography
INTRODUCTION
Metastases in clear cells renal carcinoma (ccRC) are present in the 25-30% of patients. Lungs are the most common site of initial recurrence, while are interested in metachronous way in the 30-50% of patients with ccRC [1]. Surgical resection of pulmonary metastases is an established treatment in selected patients with ccRC and the reported 5-year survival after metastasectomy is 21% to 60% which is higher than the 3% to 11% survival reported for non-operated patients [1].
CASE PRESENTATION
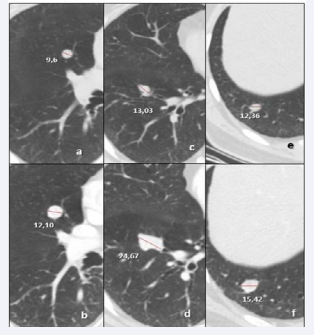
We herein present the case of a71 year-old man, ex-smoker, with history of surgically treated ccRC in 1996 (pT2 N0M0) and colonic adenocarcinoma operated in 2007 (pT1 N0). At the time of diagnosis of ccRC some solid nodules have been found in both lungs, in particular three solid lesions were found in the right lung: one of 1,4 centimeters (cm) in diameter in the anterior segment of the lower lobe, a small subcentimetric nodule in the basal segment of the same lobe and another one of 1 cm in the anterior segment of the upper lobe (Figure1).
Figure 1 a)Nodule in anterior segment of upper lobe in 1996 and b) in 2013; c) Nodule in anterior segment of lower lobe in 1996 and d) in 2013, e) nodule in the basal segment of the right lower lobe in 1996 and in 2013 (f)
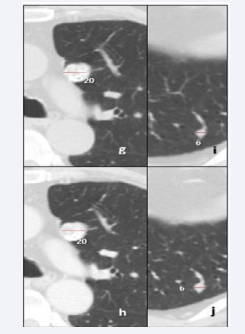
In the left lung was observed the presence of one nodule (0,6 cm in diameter) in the lower lobe and one of 2 cm in the upper lobe, typed as amarthoma by bronchoscopy, (Figure 2).
Figure 2 g) Amarthoma of the left upper lobe in 1996 and 2013 (h); i) 6mm nodule in the left lower lobe in 1996 and 2013 (j)
After surgery for renal cancer, an annual total-body CT scan of the thorax was performed for 5 years, showing stability of the lung nodules. For the history of colonic cancer, the patient has been annually subjected to total-body CT scan again, with stability of the nodules in the previous exams, but the control of December 2013 showed an increase in size of the lesions located in the anterior segment of the right lower lobe and of the one in the lower lobe, 23 vs 14 millimeters (mm) and 16 vs 13 respectively (Figure 1). A multidisciplinary equipe decided for the surgical treatment of the note lesions Therefore, the patient was subjected to surgical resection of the pulmonary nodules. The intraoperatory frozen section histological examination of the specimen showed renal origin of the tumor. For this reason the removal of the two additional nodules localized in the right lung was indicated. In particular an enucleation of the nodule in the right upper lobe was performed, while atypical wedge resection was done for the other two lesions. Hilar and mediastinal lymphadenectomy was performed.
The post-operative was complicated by Non-ST elevation Myocardial Infarct treated conservatively by the use of antiplatelet agents. The patient was discharged in the 6th post-operative day.
Histology of excised nodules showed diffuse positivity for PAS diastase, focal positivity to Vimentin and CD10 and negativity for TTF1. Lesions were compatible with metastatic ccRC with free margins. The 8 resected lymphnodes didn’t show localization of ccRC.
DISCUSSION
Reports on cases of pulmonary metastases from clear cells renal carcinoma (ccRC) are quite common in the literature and in some cases the appearance of secondary lesions may also occur after many years from the primary tumor. In literature are reported cases of pulmonary metastases from ccRC even after a long time (15 to 18 years) [2,3]. In our case the particularity is not only due to a recurrence after 18 years, but also in the fact that the presence of nodules was observed from the time of diagnosis. The patient subsequently developed an adenocarcinoma of the colon, and restarted a radiological follow-up confirming the stability of these pulmonary nodules. To our knowledge only Shiono S. and colleagues published a similar case [4] in which the presence of three little nodules in left lung was synchronous with the nephrectomy, but their growth was observed only eight year after their appearence.
Patients with isolated pulmonary metastases have a favorable prognosis compared with other disseminations. Several factors have been associated with improved outcome, including complete resection, long disease free interval, absence of lymph nodes metastases and small solitary metastases [5]. Our case leaves many open questions about the reasons why these nodules have remained in a state of quiescence for 18 years and only subsequently showed a tumor growth even if the patient has never been subjected to adjuvant treatments. The other open question concerns the presence of pulmonary nodules in the left lower lobe: our idea is to continue in a strict radiological FUP and to plan a surgical intervention in case of significant growth. This choose is conditioned by the slow growth of the tumor and by the cardiac comorbidities of the patient that presents an high risk of complications.
This case confirmed that ccRC may have a slow progression with late-onset secondary lesions, so an accurate pre-operative staging must always be executed and the presence of pulmonary nodules in this class of patients should always be face with possible extended radiological follow-up also in presence of stable lesions.