Targeting PI3K or AKT or mTOR Pathway in the Breast Cancer Therapy
- 1. Key Laboratory for Molecular Enzymology & Engineering, Jilin University, China
- 2. College of Life Science, Jilin University, China
Abstract
Phosphatidylinositol 3-kinase (PI3K)/AKT/ (mTOR) mammalian target of rapamycin signaling pathway is one of the most important pathways that regulates critical cellular functions including survival, metabolism and proliferation. Now many studies have shown that mutations or over-activation of this pathway induces tumorigenesis and metastasis in various kinds of cancers. Here, we presented the components and anti-apoptotic mechanisms of PI3K/AKT/mTOR signaling pathway in cancer cells. We also provided a reference data of PI3K/AKT/mTOR inhibitors in pre-clinical or clinical trials. All together, we explored the reason why inhibition of the pathway may serve as a promising target for cancer therapy.
Keywords
• PI3K/AKT/mTOR Breast cancer target therapy
Citation
Chai S, Shi W (2016) Targeting PI3K/AKT/mTOR Pathway in the Breast Cancer Therapy. JSM Clin Oncol Res 4(1): 1048.
INTRODUCTION
Breast cancer has been one of the most common diseases in the worldwide, and the incidence of breast cancer tends to rise especially in the female groups. Recent studies showed that mutations with 48% PI3CA genes and 16% PTEN genes occurred in invasive lobular carcinoma (ILC), a histologic subtype of invasive breast cancer [1-3]. Activated p-AKT plays an important role in proliferation, differentiation and survival of cells. There were studies showed that high activity of PI3K/AKT/mTOR signal induced resistance of chemotherapy and HER2-targeted therapy [4]. Therefore, inhibitors targeting EGFR and PI3K/Akt/mTOR pathway have emerged as potential treatment for the breast cancer [5-8]. Currently, more and more inhibitors targeting PI3K/AKT/mTOR pathway have been identified as promising drugs alone or in combination with other chemotherapy. So we will share our views on the preclinical and clinical results that inhibitors targeted PI3K/AKT/mTOR signal pathway in the treatment of different subtypes of breast cancer.
Breast cancer subtypes and its relevance of alterations in PAM pathway
Clinically, according to biologic or phenotypic markers, breast cancer was divided into the subtypes. Estrogen receptor alpha-positive (ER+) and/or progesterone receptor positive (PR+) - hormone receptor positive (HR+) - breast cancer (70-75%) is the most common clinical subtype [4]. Azim, HA., et al., has reported that in patients with HR +/HER - metastatic breast cancer had mutated PIK3CA (29.2%) [9]. In a recent study by the Cancer Genome Atlas Network, PIK3CA mutations were detected in 45% and 29% of ER+/HER- and ER+/HER+ subtypes, respectively [2]. Another report showed that 15.8% of the primary breast carcinomas possessed PIK3CA mutations in either exon 9 or exon 20. Also, they referred that PIK3CA mutation was found to be a frequent genetic change in all breast cancer subtypes but occurred with the highest rate in HR(+)/HER2(-) tumors [10]. Extensive evidences have implicated PI3K/AKT/mTOR axis aberrations in a series of breast cancer subtypes [11-15]. The mutations in the PI3K/AKT/ mTOR pathway induced resistance with breast cancer therapy, which gave a strong rational reason to develop inhibitors to restore the sensitivity to the traditional treatment with different subtypes of breast cancer [9].
PI3K/AKT/mTOR signal transduction pathway
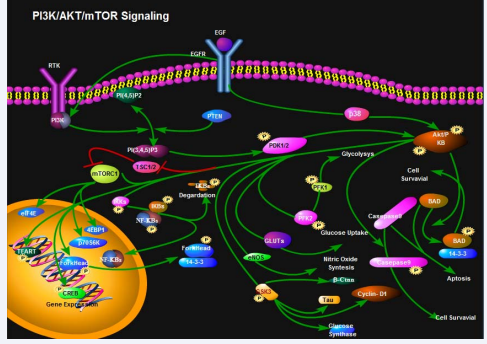
PI3K/AKT/mTOR signaling pathway is mainly composed of phosphatidylinositol 3-kinase (PI3K), serine/threonine kinase B (AKT) and mammalian target of rapamycin (mTOR) [16]. PI3K is a member of lipid kinases family, and it includes a p110 catalytic subunit and a regulatory p85 subunit which were encoded by PIK3CA gene and PIK3R1 gene respectively. It plays an important role in multiple cellular processes, including metabolism, differentiation, migration, survival and proliferation [17]. PI3K is activated in response to binding of extracellular signals to a receptor tyrosine kinase (RTK) such as HER2, epidermal growth factor receptor (EGFR) or insulin-like growth factor 1 receptor (IGF1R) [18,19] (Figure 1).
Figure 1 PI3K/AKT/mTOR signal pathway.
Once activated, p110 subunit of PI3K phosphorylates phosphatidylinositol (3,4) - bisphosphate (PIP2) to form phosphatidylinositol (3,4,5) - trisphosphate (PIP3). The aforementioned process could lead to activation of the serine/ threonine kinase AKT (protein kinase B) [20]. And the AKT was fully activated when the Ser473 site was phosphorylated by mTORC2 [21]. Since AKT is the central mediator of the pathway, it phosphorylated a series of downstream substrates including mTOR. Activated p-AKT regulates cell growth through promoting survival and anti-apoptosis. One of the downstream substrates, Gsk-3β could regulate cellular microtubule dynamics and organization [22]. Through inhibition of TSC1/2, p-AKT blocked ribosome biogenesis and protein translation by indirectly activating mTORC1 [23]. P-AKT promoted cells survival by inactivation of pro-apoptotic proteins such as caspase3, Bad/Bax [4,24]. In PI3K pathway, mTOR acts as both a downstream effect or and an upstream regulator [25-27]. mTOR includes two kinds of complex, rapamycin-sensitive (mTORC1) and rapamycin-insensitive (mTORC2). By inhibition of tuberous sclerosis complex (TSC) 1/2 activity, the activated AKT initiate the mTORC1-mediate signaling pathway, involving in the phosphorylation of ribosomal protein S6 kinase (pS6k), eukaryotic initiation factor 4E (eIF4E) and eukaryotic initiation factor binding protein 1(4EBP1), which participate in protein translation, ribosome biogenesis as well as cell growth [27-29]. The PI3K/AKT pathway is negatively regulated by phosphatase and tensin homolog (PTEN), a lipid phosphatase that dephosphorylates PIP3 [4,30]. Recent studies showed that mutations with 48% PI3CA genes and 16% PTEN genes occurred in invasive lobular carcinoma (ILC), a histologic subtype of invasive breast cancer [1].
The development of inhibitors targeting PI3K/AKT/ mTOR pathway
As described earlier, activation of the PI3K/AKT/mTOR signal pathway often were related with the multidrug resistance (MDR) phenotype in breast cancer. Therefore, a number of preclinical inhibitors targeting PI3K/AKT/mTOR pathway have been reported effective for different types of breast cancer both in vitro and in vivo [31-33]. And more and more inhibitors of this pathway were undergoing clinical trials (Table 1).
Table 1: Clinical trials targeting PI3K/AKT/mTOR pathway.
|
Drug
|
Targets
|
Combination Partner |
Patient group
|
Phase
|
State
|
Trail ID
|
|
BKM120 |
PI3K |
|
triple-negative breast cancer |
II |
completed |
NCT01629615 |
|
BKM120, Neoadjuvant Trastuzumab |
PI3K, HER2 |
Paclitaxel |
HER2-positive primary breast cancer |
II |
completed |
NCT01816594 |
|
BKM120 BEZ235 |
PI3K, PI3K/mTOR |
Letrozole |
HR-positive breast cancer |
II |
completed |
NCT01248494 |
|
BEZ235 |
PI3K |
|
advanced breast cancer |
Ι |
completed |
NCT00620594 |
|
BKM120, GSK1120212 |
PI3K, MEK |
|
triple-negative breast cancer |
Ιb |
completed |
NCT01155453 |
|
MK2206
|
AKT |
LapatinibDitosylate |
HER2-positive breast cancer |
Ι |
completed |
NCT01245205 |
|
AZD5363 |
AKT |
|
invasive breast cancer |
II |
recruiting |
NCT02077569 |
|
GSK2141795 |
AKT |
Trametinib |
triple-negative breast cancer |
II |
recruiting |
NCT01964924 |
|
AZD5363
|
AKT |
Paclitaxel
|
triple-negative breast cancer |
II |
recruiting |
NCT02423603 |
|
AZD5363, AZD2014 |
AKT, mTORC1/2 |
|
triple-negative breast cancer |
Ι/II |
recruiting |
NCT02208375 |
|
GSK1120212, GSK2110183 |
AKT, MEK |
|
breast cancer |
Ι |
completed |
NCT01476137 |
|
Everolimus |
mTOR |
Erlotinib |
metastatic breast cancer |
Ι/II |
completed |
NCT00574366 |
|
Lapatinib, Everolimus |
EGFR, mTOR |
|
triple-negative breast cancer |
II |
terminated |
NCT01272141 |
|
Everolimus |
mTOR |
Trastuzumab |
HER2-positive breast cancer |
Ι |
completed |
NCT00317720 |
|
Everolimus |
mTOR |
Exemestane |
ER-positive breast cancer |
III |
completed |
NCT00863655 |
|
Everolimus |
mTOR |
Cisplatin, Paclitaxel |
metastatic breast cancer |
Ι/II |
completed |
NCT01031446 |
|
Tamoxifen |
mTOR |
Tamoxifen-RAD001 |
anti-aromatase resistant breast cancer |
II |
ongoing |
NCT01298713 |
|
Everolimus |
mTOR |
Everolimus-Placebo |
metastatic breast cancer |
III |
terminated |
NCT01773460 |
|
Everolimus |
mTOR |
Exemestane,Everolimus -Placebo |
ER-positive breast cancer |
III |
completed |
NCT00863655 |
|
Everolimus |
mTOR |
Trastuzumab, Paclitaxel |
HER2-Positive breast cancer
|
III |
ongoing |
NCT00876395 |
Abbreviations: HR-Hormone Receptor; HER2-Human Epidermal growth Factor Receptor-2; ER-Estrogen receptor.
BKM120 can significantly inhibit the proliferation of the triple-negative breast cancer cell lines [34]. Y Hu et al., reported that BKM120 showed significant cytotoxic activity on MDR breast cancer cells both in vitro and in vivo [3]. A phase I clinical study of BKM120 has been done in patients with advanced breast cancers. And the results demonstrated that BKM120, at the maximum-tolerated dose (MTD) of 100 mg/d, is safe and well tolerated, with a favorable pharmacokinetics (PK) profile, clear evidence of target inhibition, and preliminary antitumor activity [35]. BKM120 single drug has been completed the phase clinical trials (NCT01629615) (Table 1). Besides, BKM120 was also reported to be effective when in combination with other drugs [36,37]. And now phase clinical trials on BKM120 in combination with trastuzumaband paclitaxel for HER2-positive primary breast cancer was in the completed status (NCT01816594) (Table 1).
Because of AKT playing a central role in the PI3K/AKT/mTOR pathway, inhibitors targeting AKT were also critical in blocking the pathway. Allosteric AKT inhibitor MK-2206 has antitumor activity alone and in combination with chemotherapy [38]. Some other reports showed that combining anastrozole with AKT inhibitor MK-2206 showed more sensitivity to breast cancer cells in vitro [39]. MK-2206 in combination with lapatiniband ditosylateon HER2-positive breast cancer was completed in phase Ι clinical trials (NCT01245205) (Table 1) [7]. Hudis C, Swanton C et al., has reported the AKT inhibitor MK-2206 can be safely combined with trastuzumab, and is associated with clinical activity in a phase I study on HER2-positive patients [40]. A Phase I b study on MK-2206 at a dose of 135 mg/week in combination with weekly paclitaxel and trastuzumab was conducted, the results of which was demonstrated safe and well tolerated [8]. Another specific AKT inhibitor was reported to effectively induce cancer cell apoptosis [41,42]. AZD5363 single drug was ongoing phase clinical trial with the invasive breast cancer (NCT02077569) (Table 1). The combination of AZD5363 with fulvestrant was reported as a potential therapy for breast cancer that is sensitive or resistant to E-deprivation or tamoxifen [43]. Now a phase clinical trial on AZD5363 in combination with paclitaxel for triple-negative breast cancer is recruiting (NCT02423603) (Table 1).
As the downstream of activated AKT, mTOR was another therapeutic target to block the transduction of PI3K/AKT/ mTOR pathway. As mTOR plays a key role in the initiation and development of breast cancer, and its inhibitor CCI-779 exerts a strong suppressive activity against MDA-MB-231 cells [44]. The safety, tolerability and pharmacokinetic parameters were demonstrated to be reasonable in the phase I study. Also, the Phase I study results showed that CCI-779 displayed no immunosuppressive effects with manageable and reversible adverse events at doses up to 220 mg [45]. A Phase II Study of temsirolimus (CCI-779) was conducted by Stephen Chan, Max E. Scheulen, et al. In this study, two groups of different doses were set in heavily pretreated patients with locally advanced or metastatic breast cancer, 75 and 250 mg temsirolimus. The results showed both groups presented the antitumor activity and 75 mg temsirolimus showed a generally tolerable safety profile [46]. Another mTOR inhibitor, everolimus was rapamycin analogues and one of the important mTORC1 inhibitors especially in breast cancer [47-49]. A Phase Ι/II clinical trial showed that inhibition of mTOR restored the sensitivity to trastuzumab-treatment in patient HER2-overexpressing metastatic breast cancer MBC (NCT00317720) [50]. To evaluate the efficacy and safety of everolimus in combination with tamoxifen, the randomized Phase II TAMRAD (everolimus plus tamoxifen) was performed in the aromatase inhibitors (AIs) resistance MBC patients. The results showed that clinical benefit rate (CBR) was 61% in the combination group whereas it was 42% in the tamoxifen monotherapy group (P = 0.04) [51]. In this study, time to progression (TTP) was 4.5 months and 8.6 months in the tamoxifen and combination groups, respectively (P = 0.002) [52]. However, the incidences of serious side effects were similar in both groups, with 32% for each group. In overall, the Phase II TAMRAD study demonstrated that tamoxifen plus everolimus increased CBR and TTP comparedto tamoxifen monotherapy in aromatase inhibitor resistant postmenopausal MBC patients.
In a Phase III randomized BOLERO-2 (The Breast Cancer Trials of Oral Everolimus-2) trial, HER2-negative MBC patients were recruited. Median PFS of the exemestane plus everolimus group was 6.9 months, while the exemestane plus placebo group was 2.8 months (P < 0.001) [53]. After a median 18months follow-up, the final PFS analysis of the BOLERO-2 trial show edeverolimus plus exemestane compared to exemestane plus placebo had significantly higher PFS (7.8 months vs 3.2 months; P < 0.0001) [54]. The exemestane plus everolimus group was reported a 25.4% death rate, fewer than the exemestane plus placebo group with a 32.2% death rate [52]. Thus, the exemestanein combination with everolimus may be more promising for future clinical application.
A randomized Phase III study (BOLERO-3) was designed to assess whether the addition of the mTOR inhibitor everolimus to trastuzumab might restore sensitivity to trastuzumab in trastuzumab-resistant, taxane-pretreated HER2-positive MBC patients [52]. Median PFS was 7.00 months with everolimus and 5.78 months with placebo (p = 0.0067). Serious adverse events were reported in 117 (42%) patients in the everolimus group and 55 (20%) in the placebo group; two on-treatment deaths due to adverse events occurred in each group [55]. The BOLERO-3 clinical trial results showed that the addition of everolimus to trastuzumabin combination with vinorelbine could significantly prolong PFS in patients with trastuzumab-resistant and taxane-pretreated, HER2-positive, advanced breast cancer.
A Phase III, randomized BOLERO-1 trial was conducted. And it aimed to assess the efficacy and safety of the combination of everolimus with trastuzumab plus paclitaxelas first-line treatment for patients with HER2-positiveadvanced breast cancer [56]. In the full population, median progression free survival (PFS) was 14.95 months with everolimus versus 14.49 months with placebo (p = 0.1166). In the HR-negative subpopulation (n = 311), median progression-free survival with everolimus was 20.27 months versus 13.08 months with placebo (p = 0.0049). In this BOLERO-1 trial results, progression-free survival was not significantly different between groups in the full analysis population, however, the 7.2 months prolongation was noted with the addition of everolimus in the HR-negative, HER2- positivepopulation. Clinical application of everolimus is generally very well tolerated with most common side effects including stomatitis, rash, fatigue, hyperglycemia, hyperlipidemia, and myelosuppression [57]. So, other mTOR analogues including CCI-779 (temsirolimus) and AP23573 (ridaforolimus) are developed [58,59].
CONCLUSIONS
As we discussed here, PI3K/AKT/mTOR signal pathway plays an important role in proliferation and survival of breast cancer. Different subtypes of breast cancer had mutations of this pathway, which induced multidrug resistance phenotype in breast cancer. Therefore, inhibitors targeting this pathway seem promising and rational in the breast cancer therapy. Although more and more inhibitors targeting PI3K/AKT/mTOR pathway have been reported, most of them stayed preclinical research stage because of existed problems including poor solubility, poor stability, cytotoxicity. Breast cancer also had complex conditions compared to other solid tumors. Different subtypes of breast cancers presented mutations of PI3K/AKT/mTOR pathway in different degrees, which resulting in different sensitivity to these inhibitors. Collectively, there are all relevant restrictions to targeted therapy based on PI3K signal pathway. Combination of multiple targets and personalized treatment may be the future perspective for breast cancer therapy.
REFERENCES
18. Cantley LC. The phosphoinositide 3-kinase pathway. Science. 2002; 296: 1655-1657.
25. Guertin DA, Sabatini DM. An expanding role for mTOR in cancer. Trends Mol Med. 2005; 11: 353-361.
26. Guertin DA, Sabatini DM. Defining the role of mTOR in cancer. Cancer Cell. 2007; 12: 9-22.
28. Hay N, Sonenberg N. Upstream and downstream of mTOR. Genes Dev. 2004; 18: 1926-1945.