Use of Clinical Decision Support Systems by Oncology Nurses in Monitoring High-Risk Cancer Medications
- 1. Department of Oncology-Hematology, One Day Clinic, Hellenic Airforce General Hospital, Greece
Keywords
• CDSSs; Oncology Nurses; Monitoring High-Risk; Cancer Medications
Citation
Ioanna Tsatsou RN. (2025) Use of Clinical Decision Support Systems by Oncology Nurses in Monitoring High-Risk Cancer Medications-Onset Gastric Cance. JSM Clin Oncol Res 13(1): 1076.
Abstract
Clinical Decision Support Systems (CDSSs) have emerged as vital instruments in oncology settings, particularly for nursing professionals managing high-risk cancer medications. As cancer incidence continues to rise globally, the complexity and toxicity of anticancer therapies necessitate robust mechanisms to ensure patient safety. This review explores the use of CDSSs by oncology nurses to monitor high-risk medications, focusing on their role in identifying dosage errors, contraindications, and potential toxicity. A narrative literature review was conducted using key databases, targeting studies from the last decade that examined CDSSs applications in oncology nursing. The analysis identified recurring themes related to medication safety, user experience, integration into clinical workflow, and educational implications. While CDSSs significantly contribute to error reduction and improved clinical judgment, challenges such as system interoperability, alert fatigue, and limited nurse-specific customization were noted. The findings emphasize the need for continuous development and tailored implementation of CDSSs to optimize their utility in oncology nursing practice. Clinical implications include enhanced patient safety, improved nurse confidence in medication management, and the potential for data-driven nursing education. Future directions suggest more comprehensive integration of artificial intelligence and machine learning algorithms into CDSSs, increased interdisciplinary collaboration in tool design, and further research on long-term clinical outcomes. T
INTRODUCTION
Cancer is a leading cause of morbidity and mortality worldwide, with increasing incidence rates placing a substantial burden on healthcare systems. According to the World Health Organization, global cancer cases are projected to reach 27.5 million annually by 2040 [1]. This surge is driven by various factors including aging populations, increased exposure to environmental carcinogens, unhealthy lifestyles, and advances in early detection and diagnosis [2]. With the rising number of patients undergoing complex and aggressive cancer therapies, there is an urgent need to ensure safe and effective medication management [3]. High-risk cancer medications, including chemotherapeutic agents, targeted therapies, and immunotherapies, possess narrow therapeutic indices and are associated with severe adverse effects. These treatments require precise dosing, continuous monitoring, and prompt intervention in case of toxicity [4]. Oncology nurses are central to this process, as they administer medications, observe and report side effects, educate patients, and coordinate care across multidisciplinary teams [5].
Clinical Decision Support Systems (CDSSs) are digital platforms created to aid healthcare professionals in making well-informed choices regarding patient treatment. It provides timely and relevant information, often at the point of care, to help clinicians with various aspects of their decision-making process, such as diagnosis, treatment, and medication and making informed decisions by integrating evidence-based knowledge with patientspecific data. These systems seek to enhance the delivery of healthcare by improving medical decision-making through the application of specialized clinical knowledge, individualized patient data, and additional pertinent information. The CDSSs typically work by matching patient characteristics to a computerized knowledge base, then presenting the clinician with patient-specific assessments, recommendations, or alerts. CDSSs examples are tools that may encompass computerized alerts, reminders, clinical guidelines, order sets, diagnostic support, and documentation templates. Numerous CDSSs are incorporated into electronic health records (EHR) and various computerized clinical workflows to enhance their application at the point of care [6,7].
CDSSs can help reduce errors, improve efficiency, enhance patient safety, and provide more accurate and timely information to clinicians. CDSSs have evolved significantly since their initial development, becoming more sophisticated and capable of leveraging large datasets and sophisticated analytics. In essence, CDSSs provide a tool for clinicians to combine their expertise with the power of data and knowledge to make better decisions and improve patient outcomes [8].
In oncology, CDSSs play a pivotal role in enhancing the safety and precision of cancer care. These digital tools are integrated into electronic health records to provide real-time alerts, evidence-based recommendations, and diagnostic support tailored to the complexities of oncology practice. CDSSs assist clinicians and oncology nurses in identifying potential medication errors, contraindications, and drug–drug interactions-particularly crucial when managing high-risk cancer therapies. By analyzing patientspecific data such as lab results, comorbidities, genetic markers, and treatment histories, CDSSs can support early detection of adverse effects and guide timely interventions. Furthermore, they aid in standardizing chemotherapy protocols, ensuring appropriate dosing, and improving adherence to clinical guidelines. As oncology becomes increasingly complex with personalized treatments and combination regimens, CDSSs serve as essential tools to support decision-making, reduce variability in care, and ultimately improve patient outcomes [9,10].
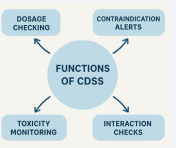
In oncology nursing practice, CDSSs are particularly valuable. Nurses often operate in high-pressure environments with heavy workloads, making cognitive support tools essential. CDSSs offer a suite of vital functions designed to enhance patient safety and care quality throughout the cancer treatment continuum (Figure 1). One of the primary functions is dosage checking, where CDSSs verify prescribed chemotherapy doses against standardized protocols and individualized patient parameters-such as body surface area, renal function, and hepatic status—to prevent potentially harmful over- or under-dosing. CDSSs can flag potential dosage errors, suggest appropriate drug regimens based on lab values and patient characteristics, and warn against contraindications [11]. Another key function is contraindication alerting, where the system automatically scans for conflicts based on patient-specific data, including medical history, comorbidities, allergies, and recent lab values, thereby reducing the risk of administering inappropriate or dangerous medications [12].
Figure 1: Functions of CDSS in oncology nursing practice.
CDSSs also contribute significantly to early detection of adverse drug reactions and treatment-related toxicities by integrating patient symptoms and biometric data into risk prediction models. This is achieved through the integration of patient-reported outcomes, laboratory trends, and clinical indicators that alert nurses and clinicians to emerging toxicities before they escalate [13]. Furthermore, interaction checks are an essential component, with the system continuously evaluating for potential drug–drug or drug–disease interactions. This is especially critical in oncology, where patients often undergo complex regimens involving multiple chemotherapeutic and supportive agents [14], Collectively, these functions support oncology nurses in making timely, informed decisions that enhance therapeutic effectiveness while minimizing risks [7,13].
Despite these benefits, the adoption and effectiveness of CDSS in oncology nursing are influenced by multiple factors. These include system design, usability, level of training provided, organizational support, and interoperability with other digital platforms. Understanding how these systems are used by oncology nurses and what outcomes they produce is critical for optimizing their implementation [7,8].
The aim of this narrative review is to evaluate the current use of CDSS by oncology nurses in monitoring high-risk cancer medications. By analyzing existing literature, we aim to provide an overview of the benefits, challenges, and future directions for CDSS in oncology nursing practice.
METHODS
A narrative literature review was conducted to gather evidence on the use of CDSSs by oncology nurses in the context of high-risk cancer medication monitoring. The review of the databases (PubMed, CINAHL, Scopus, Web of Science), focused on literature published between 2014 and 2024. The following keywords were used: “clinical decision support systems” OR “CDSS”, “oncology nursing”, “high-risk medications”, “cancer drug monitoring”,”chemotherapy toxicity”. Included studies were peer-reviewed, published in English that focus on the use of CDSS by oncology nurses for high-risk medications. Studies that did not involve nursing practice, did not address cancer medication monitoring, or were editorials, commentaries, or conference abstracts were excluded from the analysis. A thematic analysis approach was used to identify patterns and themes across the selected studies. Themes were developed iteratively through a process of categorizing key findings.
RESULTS
The thematic analysis identified several recurrent themes regarding the use of CDSSs from oncology nurses for high-risk cancer medication management.
Enhancement of medication safety
CDSSs play a critical role in enhancing medication safety within oncology settings, where the complexity and risk associated with chemotherapy regimens are particularly high. Studies consistently highlight that CDSSs significantly reduce medication errors by providing real-time alerts for incorrect dosages, inappropriate administration schedules, and dangerous drug–drug interactions. These systems are integrated into electronic health records and draw on patient-specific data, such as weight, renal function, liver enzymes, and treatment history, to ensure accurate and individualized medication recommendations [16,17].
One of the most notable benefits observed is the reduction in chemotherapy dosing errors, which are often a result of complex calculations and variable protocols. CDSSs serve as an additional layer of verification, thereby supporting oncology nurses in administering high-risk medications safely. These systems also help in identifying administration timing discrepancies, ensuring that drugs with narrow therapeutic windows are delivered precisely as prescribed [18,19]. Additionally, CDSS can detect potential interactions not only between cancer drugs but also with supportive medications commonly used to manage side effects such as nausea, pain, or infection [13].
Nurses report increased confidence in managing complex and evolving treatment regimens, especially those involving novel agents with frequently updated dosing guidelines. The use of CDSS enables nurses to remain aligned with the latest evidence-based practices without the constant need to manually verify each change [20]. Overall, CDSS contribute to a safer, more standardized, and efficient medication administration process, ultimately improving patient outcomes in oncology care.
Detection of contraindications and risk factors
Then, CDSSs have proven instrumental in assisting oncology nurses with the early detection of contraindications and patient-specific risk factors that could compromise treatment safety. These tools integrate comprehensive clinical data, including laboratory results, comorbidities, prior treatment regimens, and current physiological parameters, to screen for potential issues that may contraindicate certain cancer therapies. In high-risk oncology patients, even subtle deviations in organ function or drug sensitivity can have significant consequences, making automated, real-time screening vital [21,22].
One of the most impactful features of CDSS in this domain is their incorporation of renal and hepatic function calculators. These tools allow for automated dose adjustments based on current lab values such as creatinine clearance, AST/ALT levels, and bilirubin, which are critical in determining the patient’s ability to safely metabolize and excrete chemotherapeutic agents. For instance, dose modifications for nephrotoxic agents like cisplatin or hepatotoxic drugs such as methotrexate are more reliably calculated when these integrated decision supports are used [23,34].
Additionally, CDSS can flag risks associated with patientspecific contraindications-such as prior hypersensitivity reactions, poor marrow reserve, or concurrent illnesses like heart failure or uncontrolled diabetes—that may otherwise be overlooked in a busy clinical environment. These systems enhance clinical vigilance and support proactive decision-making, reducing the likelihood of preventable adverse events [25]. For oncology nurses, this not only improves patient safety but also provides a structured approach to managing increasingly complex treatment protocols.
Early identification of toxicity
The early detection and management of treatmentrelated toxicities are crucial components of oncology care, and CDSSs have emerged as valuable tools in achieving this goal. Advanced CDSS platforms leverage real-time data integration from electronic health records, laboratory systems, and patient-reported outcome measures to detect early warning signs of toxicity. This functionality allows oncology nurses to respond proactively to complications such as neutropenia, cardiotoxicity, hepatotoxicity, and infusion-related reactions, some of the most serious and potentially life-threatening adverse events in cancer treatment [25,26].
These systems often incorporate algorithm-based assessments that monitor laboratory trends, including white blood cell counts, troponin levels, liver enzymes, and other biomarkers that can signal the onset of toxicity. Importantly, integration with mobile patient monitoring applications enables patients to report symptoms remotely, such as fever, fatigue, shortness of breath, or palpitations. CDSS can interpret these inputs and generate real-time alerts for clinical staff, prompting timely evaluation and intervention before complications escalate [27,28].
Nurses using these systems have reported improved confidence in managing adverse events and greater ability to prioritize care for high-risk individuals [20]. Several studies have demonstrated that early intervention driven by CDSS alerts can reduce the rate of unplanned hospitalizations, decrease therapy interruptions, and ultimately improve the continuity and safety of cancer care [29]. By facilitating earlier recognition and management of toxicities, CDSS not only protect patients from serious harm but also support optimal treatment adherence and outcomes.
Monitoring of high-risk cancer medications and adverse events
A prominent theme in the literature is the use of CDSSS for proactive monitoring of high-risk cancer medications and associated adverse events [7]. These systems continuously analyze patient data, including medication regimens, laboratory results, and vital signs, to detect early indicators of complications such as febrile neutropenia, hepatotoxicity, or thrombocytopenia [8]. Nurses reported that these tools not only supported timely clinical decision-making but also served as educational resources to understand the evolving toxicity profiles of new cancer therapies [20]. Moreover, by integrating patient-reported outcomes and biometric data, CDSS enhanced remote monitoring capabilities, enabling nurses to track adverse events even in outpatient or home-based care settings [30].
Improved workflow efficiency and communication
The integration of CDSSs into oncology nursing practice has led to significant improvements in workflow efficiency and interdisciplinary communication. By automating routine but critical tasks, such as dose calculations, regimen scheduling, and toxicity risk assessments, CDSSs help streamline clinical processes and reduce manual workload for nurses. These systems also standardize documentation practices, ensuring that all clinical entries align with institutional protocols and regulatory requirements. As a result, the risk of transcription errors is minimized, and the documentation burden is alleviated, allowing nurses to allocate more time to direct patient care [31,32].
Furthermore, CDSS facilitate seamless communication across the oncology care team [10]. They serve as shared platforms where nurses, pharmacists, and oncologists can access up-to-date treatment plans, medication changes, and patient-specific alerts in real time. This shared visibility promotes faster clinical decision-making and helps prevent miscommunication, particularly in highrisk scenarios such as chemotherapy preparation and administration [33-35].
Nurses have reported fewer delays in initiating therapy and noted that CDSS reduced the need for manual clarification of orders, especially in complex regimens involving multiple dose adjustments or supportive medications [35]. Enhanced coordination with pharmacy services is another key benefit, with CDSS automatically generating alerts or flags for drug availability issues, compounding instructions, and compatibility concerns. The resulting efficiency not only improves the timeliness and safety of medication delivery but also enhances overall patient satisfaction and care continuity [13]. Collectively, these improvements underscore the vital role of CDSS in creating a more responsive, connected, and streamlined oncology care environment.
Implementation barriers and alert fatigue
Several implementation challenges have been identified, particularly in oncology nursing. One of the most commonly reported barriers is poor system design that does not align with real-world nursing workflows. Many CDSS platforms are developed with physician-oriented processes in mind, leading to a lack of customization for nursing-specific tasks such as bedside administration, symptom monitoring, and patient education. This mismatch can hinder usability and reduce the system’s overall effectiveness in nursing practice [36,37].
Another major concern is alert fatigue, a phenomenon in which users become desensitized to frequent, often nonspecific system alerts [38]. In systems with low specificity, nurses are inundated with warnings that are not clinically relevant, leading them to override or ignore alerts altogether. Over time, this desensitization can compromise patient safety and diminish trust in the system’s recommendations Studies have reported that nurses sometimes bypass alerts they perceive as redundant or not applicable to their patient population, which undermines the intended safety function of CDSS. Addressing these challenges requires the development of more intelligent, user-centered systems that prioritize relevant alerts and incorporate feedback from frontline nursing staff during design and implementation phases [39,40].
Education and training needs
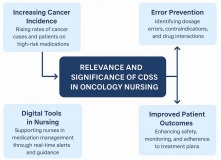
The relevance and significance of CDSS in oncology nursing practice (Figure 2) is proven, but the successful integration of them in daily practice is highly dependent on comprehensive education and ongoing training [41].
Figure 2: Relevance and significance of CDSS in oncology nursing practice.
Nurses who receive structured, hands-on instruction on CDSS functionality are significantly more likely to engage with the system effectively and adhere to its recommendations. Nurses perceive CDSSs as more trustworthy and precise compared to paper-based assessment [42]. Training ensures that users understand how to navigate the interface, interpret alerts appropriately, and integrate system outputs into their clinical decisionmaking processes [43].
Without adequate preparation, nurses may experience uncertainty or frustration when interacting with CDSS, leading to underutilization or incorrect use. Formal education sessions, including scenario-based simulations and continuous support, improve user confidence, system adoption, and overall satisfaction [44]. Nurses who felt well-trained were more likely to appreciate the system’s benefits, such as early toxicity detection and dosing accuracy, and less likely to dismiss alerts as irrelevant or burdensome [30].
Moreover, education plays a key role in bridging the gap between technological tools and patient-centered care. It empowers nurses to critically evaluate system recommendations and apply them within the context of individual patient needs. Ongoing training and system updates are essential, especially in oncology, where drug protocols and clinical guidelines evolve rapidly [45]. Investing in nurse education is therefore a foundational component of successful CDSS implementation and sustainability.
DISCUSSION
The integration of CDSS into oncology nursing practice offers profound benefits in monitoring high-risk cancer medications. One of the most salient findings of this review is the improvement in medication safety and adverse event detection. The real-time nature of CDSS alerts empowers nurses to act promptly, potentially preventing life-threatening complications. The ability of CDSS to detect dosage errors and contraindications is especially crucial in oncology, where therapeutic regimens are highly individualized and toxicity profiles vary significantly between patients [46].
The findings suggest that nurses equipped with CDSS are more confident in adjusting treatment plans, advocating for dose modifications, and collaborating effectively with physicians and pharmacists. Moreover, CDSS facilitate a more proactive approach to care. By integrating continuous patient monitoring and real-time symptom reporting, these tools help nurses identify toxicity before clinical deterioration occurs. This not only enhances patient safety but also reduces hospital readmissions and healthcare costs. Nevertheless, successful implementation of CDSS is not without challenges. Alert fatigue remains a pressing concern; excessive or lowvalue alerts can desensitize users, resulting in critical warnings being overlooked. Additionally, many CDSS are not designed with nursing-specific workflows in mind, limiting their usability and relevance to nursing tasks.
CDSSs as stated in the results offer several key advantages in oncology nursing, notably enhancing patient safety by reducing medication errors and enabling early detection of adverse events such as toxicity and contraindications. These tools support standardized, evidence-based care and improve workflow efficiency by streamlining documentation and monitoring tasks. CDSS also assist nurses in managing complex chemotherapy regimens involving multiple drugs and potential interactions.
However, limitations exist, including alert fatigue caused by frequent, non-specific notifications that can overwhelm staff and lead to important warnings being ignored. Poorly integrated systems may disrupt clinical workflows, while over-reliance on technology may inadvertently diminish critical thinking. Additionally, effective implementation requires substantial training and resources to ensure proper use and adoption by nursing staff (Table 1).
Table 1: Advantages and considerations on the use of CDSSs in oncology nursing practice.
|
Advantages |
Considerations |
|
Improved Patient Safety: Reduces medication errors, especially with high-risk cancer drugs. |
Alert Fatigue: Frequent, non- specific alerts can overwhelm nurses. |
|
Early Detection of Adverse Events: Assists in identifying toxicity and contraindications early. |
Workflow Disruption: Poorly integrated systems can interrupt clinical routines. |
|
Standardized Care: Promotes evidence-based, consistent decision-making. |
Dependence on Technology: May reduce critical thinking if over-relied upon. |
|
Enhanced Efficiency: Streamlines documentation and monitoring tasks. |
Training Requirements: Requires time and resources for proper nurse training. |
|
Enhanced Decision-Making: Access to a vast array of information, encompassing patient records, medical literature, and optimal practices, |
|
|
Support for Complex Regimens: Helps manage multi-drug protocols and interactions. |
|
In addition to the clinical benefits of CDSSs, understanding the subjective experiences of oncology nurses is critical for successful implementation. Several studies highlight challenges such as initial resistance to adopting new technologies, steep learning curve, variations in perceived utility and trust, and cognitive overload during the early phases of CDSS use. Nurses report that systems not tailored to their workflows can lead to frustration and inefficiency [8,17,41,47-49].
Qualitative findings suggest that alert fatigue is a significant concern. Nurses reported feelings of cognitive overload during the initial phases of CDSS implementation and expressed frustration with excessive alerts, contributing to alert fatigue. Repetitive or non-specific alerts lead to desensitization, reducing the likelihood that critical warnings will be heeded. In contrast, nurses expressed greater trust and engagement with CDSSs when they were involved in system design or customization, resulting in improved alignment with clinical workflows [50-53].
Despite their potential, implementing CDSSs presents economic challenges. Start-up costs include hardware procurement, software licensing, and comprehensive training programs. For resource-limited hospitals, additional barriers such as weak technology infrastructure, inconsistent internet access, and limited staff capacity further complicate adoption [54]. Nonetheless, studies suggest that CDSSs can offer cost savings by reducing medication errors [55], preventing hospital readmissions [56], and streamlining workflow [13].
To mitigate financial barriers, the use of open-source platforms and cloud-based solutions may offer more feasible alternatives. These platforms reduce the need for local hardware investment and facilitate remote technical support. The review also highlights the critical role of education and training. Without adequate instruction, nurses may underutilize or misuse CDSS features. Continuous professional development and involvement of nursing staff in system design can help overcome these barriers [8]. Finally, this is a narrative review, the absence of formal search and quality assessment of the included literature is a limitation of this work.
CONCLUSIONS
CDSSs are increasingly essential in oncology nursing for the safe and effective monitoring of high-risk cancer medications. They support clinical decisionmaking, enhance patient safety, and improve workflow efficiency. Despite challenges such as alert fatigue and implementation barriers, the evidence supports their continued and expanded use. Future efforts should focus on tailoring CDSSs to nursing workflows, enhancing interoperability with other systems, and incorporating advanced technologies like artificial intelligence for predictive analytics. Examples include artificial intelligence models to predict immunerelated or chemotherapy-induced adverse events or patient stratification tools that support personalized treatment regimens based on risk profiles. These may be random forest algorithms, support vector machines, and deep learning neural networks.
Nevertheless, these uses although helpful and promising have the risk of algorithmic bias due to unbalanced training data, and the need to preserve human oversight in CDSS-enabled care. Thus transparency is of major importance in AI decisionmaking Following, interdisciplinary collaboration is vital to ensure that CDSSs are user-friendly and clinically relevant. Further research should aim to evaluate long-term patient outcomes, cost-effectiveness, and adoption in diverse healthcare settings. As the landscape of cancer care evolves, so too must the tools that support it. CDSSs offer a promising pathway toward safer, more personalized, and efficient oncology nursing practice.
REFERENCES
- World Health Organization. Cancer. Geneva: WHO; 2022.
- Prathap R, Kirubha S, Rajan AT, Manoharan S, Elumalai K. The increasing prevalence of cancer in the elderly: An investigation of epidemiological trends. Aging Med (Milton). 2024; 7: 516-527.
- Krzyszczyk P, Acevedo A, Davidoff EJ, Timmins LM, Marrero-Berrios I, Patel M, et al. The growing role of precision and personalized medicine for cancer treatment. Technology (Singap World Sci). 2018; 6: 79-100.
- Anand U, Dey A, Chandel AKS, Sanyal R, Mishra A, Pandey DK, et al. Cancer chemotherapy and beyond: Current status, drug candidates, associated risks and progress in targeted therapeutics. Genes Dis. 2022; 10: 1367-1401.
- Rieger PT, Yarbro CH. Role of the Oncology Nurse. In: Kufe DW, Pollock RE, Weichselbaum RR, et al., editors. Holland-Frei Cancer Medicine. 6th edition. Hamilton (ON): BC Decker; 2003.
- Wasylewicz ATM, Scheepers-Hoeks AMJW. Clinical Decision Support Systems. 2018 Dec 22. In: Kubben P, Dumontier M, Dekker A, editors. Fundamentals of Clinical Data Science. Cham (CH): Springer; 2019; 11.
- Sutton RT, Pincock D, Baumgart DC, Sadowski DC, Fedorak RN, Kroeker KI. An overview of clinical decision support systems: benefits, risks, and strategies for success. NPJ Digit Med. 2020; 3: 17.
- Chen Z, Liang N, Zhang H, Li H, Yang Y, Zong X, et al. Harnessing the power of clinical decision support systems: challenges and opportunities. Open Heart. 2023; 10: e002432.
- Wang L, Chen X, Zhang L, Li L, Huang Y, Sun Y, et al. Artificial intelligence in clinical decision support systems for oncology. Int J Med Sci. 2023; 20: 79-86.
- Pawloski PA, Brooks GA, Nielsen ME, Olson-Bullis BA. A Systematic Review of Clinical Decision Support Systems for Clinical Oncology Practice. J Natl Compr Canc Netw. 2019; 17: 331-338.
- Patel J, Ogletree R, Sutterfield A, Pace JC, Lahr L. Optimized Computerized Order Entry can Reduce Errors in Electronic Prescriptions and Associated Pharmacy Calls to Clarify (CTC). Appl Clin Inform. 2016; 7: 587-595.
- Desmedt S, Spinewine A, Jadoul M, Henrard S, Wouters D, DalleurO. Impact of a clinical decision support system for drug dosage in patients with renal failure. Int J Clin Pharm. 2018; 40: 1225-1233.
- Shahmoradi L, Safdari R, Ahmadi H, Zahmatkeshan M. Clinical decision support systems-based interventions to improve medication outcomes: A systematic literature review on features and effects. Med J Islam Repub Iran. 2021; 35: 27.
- Helmons PJ, Suijkerbuijk BO, Nannan Panday PV, Kosterink JG. Drug- drug interaction checking assisted by clinical decision support: a return on investment analysis. J Am Med Inform Assoc. 2015; 22: 764-772.
- Nibbelink CW, Young JR, Carrington JM, Brewer BB. Informatics Solutions for Application of Decision-Making Skills. Crit Care Nurs Clin North Am. 2018; 30: 237-246.
- Chung C, Patel S, Lee R, Fu L, Reilly S, Ho T, et al. Implementation of an integrated computerized prescriber order-entry system for chemotherapy in a multisite safety-net health system. Am J Health Syst Pharm. 2018; 75: 398-406.
- Stillman RC. Clinical decision support tools improving cancer care. In Seminars in Oncology Nursing. 2018; 34: 158-167.
- Moss J, Berner ES. Evaluating clinical decision support tools for medication administration safety in a simulated environment. Int J Med Inform. 2015; 84: 308-318.
- Ibáñez-Garcia S, Rodriguez-Gonzalez C, Escudero-Vilaplana V, Martin-Barbero ML, Marzal-Alfaro B, De la Rosa-Triviño JL, et al. Development and Evaluation of a Clinical Decision Support System to Improve Medication Safety. Appl Clin Inform. 2019; 10: 513-520.
- Thompson C, Mebrahtu T, Skyrme S, Bloor K, Andre D, Keenan AM, et al. The effects of computerised decision support systems on nursing and allied health professional performance and patient outcomes: a systematic review and user contextualisation. Health Soc Delive Care Res. 2024; 12: 1-93.
- Huibers CJA. Clinical decision support-assisted pharmacotherapy optimisation for older hospitalised patients. University Medical Center Utrecht, Utrecht, The Netherlands. 2023
- Mazo C, Kearns C, Mooney C, Gallagher WM. Clinical Decision Support Systems in Breast Cancer: A Systematic Review. Cancers. 2020; 12: 369.
- Wada R, Takeuchi J, Nakamura T, Sonoyama T, Kosaka S, Matsumoto C, et al. Clinical Decision Support System with Renal Dose Adjustment Did Not Improve Subsequent Renal and Hepatic Function among Inpatients: The Japan Adverse Drug Event Study. Appl Clin Inform. 2020; 11: 846-856.
- Sonoda A. A clinical decision support system promotes the appropriate use of drugs in hospitalized patients with kidney impairment. J Pharm Health Care Sci. 2025; 11: 26.
- Syrowatka A, Motala A, Lawson E. Computerized Clinical Decision Support To Prevent Medication Errors and Adverse Drug Events: Rapid Review. 2024 Feb. In: Making Healthcare Safer IV: A Continuous Updating of Patient Safety Harms and Practices. Rockville (MD): Agency for Healthcare Research and Quality (US); 2023.
- Pitt E, Bradford N, Robertson E, Sansom-Daly UM, Alexander K. The effects of cancer clinical decision support systems on patient- reported outcomes: A systematic review. Eur J Oncol Nurs. 2023; 66: 102398.
- Medic G, Kosaner Kließ M, Atallah L, Weichert J, Panda S, Postma M, et al. Evidence-based Clinical Decision Support Systems for the prediction and detection of three disease states in critical care: A systematic literature review. F1000Res. 2019; 8: 1728.
- Cai L, Deutsch TM, Sidey-Gibbons C, Kobel M, Riedel F, Smetanay K, et al. Machine Learning to Predict the Individual Risk of Treatment- Relevant Toxicity for Patients With Breast Cancer Undergoing Neoadjuvant Systemic Treatment. JCO Clin Cancer Inform. 2024; 8: e2400010.
- Samal L, Fu HN, Camara DS, Wang J, Bierman AS, Dorr DA. Health information technology to improve care for people with multiple chronic conditions. Health Serv Res. 2021; 56: 1006-1036.
- AL-Dossary RN. Nurses’ Perceptions of the Clinical Decision Support System Effect on Patient Safety. Safety. 2023; 9: 86.
- Olakotan OO, Mohd Yusof M. The appropriateness of clinical decision support systems alerts in supporting clinical workflows: A systematic review. Health Informatics J. 2021; 27: 14604582211007536.
- Olakotan OO, Yusof MM. Evaluating the alert appropriateness of clinical decision support systems in supporting clinical workflow. J Biomed Inform. 2020; 106: 103453.
- Al Kulayb SH, Alyami YH, Alyami AH, Aldashl EY, Al Salem HMH, Alyami HMH et al. Information Systems in Pharmacy: Enhancing Patient Safety and Outcomes. J Int Crisis Risk Commun Res. 2024; 7: 60.
- Nanji KC, Seger DL, Slight SP, Amato MG, Beeler PE, Her QL, et al. Medication-related clinical decision support alert overrides in inpatients. J Am Med Inform Assoc. 2018; 25: 476-481.
- Rahimi R, Moghaddasi H, Rafsanjani KA, Bahoush G, Kazemi A. Effects of chemotherapy prescription clinical decision-support systems on the chemotherapy process: A systematic review. Int J Med Inform. 2019; 122: 20-26.
- Wang T, Tan JB, Liu XL, Zhao I. Barriers and enablers to implementing clinical practice guidelines in primary care: an overview of systematic reviews. BMJ Open. 2023; 13: e062158.
- Meunier PY, Raynaud C, Guimaraes E, Gueyffier F, Letrilliart L. Barriers and Facilitators to the Use of Clinical Decision Support Systems in Primary Care: A Mixed-Methods Systematic Review. Ann Fam Med. 2023; 21: 57-69.
- Backman R, Bayliss S, Moore D, Litchfield I. Clinical reminder alert fatigue in healthcare: a systematic literature review protocol using qualitative evidence. Syst Rev. 2017; 6: 255.
- Obisesan O, Barber E, Martin P, Brougham N, Tymkew H. Original Research: Alarm Fatigue: Exploring the Adaptive and Maladaptive Coping Strategies of Nurses. Am J Nurs. 2024; 124: 24-30.
- Ancker JS, Edwards A, Nosal S, Hauser D, Mauer E, Kaushal R. with the HITEC Investigators. Effects of workload, work complexity, and repeated alerts on alert fatigue in a clinical decision support system. BMC Med Inform Decis Mak. 2017; 17: 36.
- Cortez S, Dietrich MS, Wells N. Measuring Clinical Decision Support Influence on Evidence-Based Nursing Practice. Oncol Nurs Forum. 2016 1; 43: E170-E177.
- Ackerhans S, Huynh T, Kaiser C, Schultz C. Exploring the role of professional identity in the implementation of clinical decision support systems-a narrative review. Implement Sci. 2024; 19: 11.
- Piscotty R, Kalisch B. Nurses’ use of clinical decision support: aliterature review. Comput Inform Nurs. 2014; 32: 562-568.
- McGreevey JD 3rd, Mallozzi CP, Perkins RM, Shelov E, Schreiber R. Reducing Alert Burden in Electronic Health Records: State of the Art Recommendations from Four Health Systems. Appl Clin Inform. 2020; 11: 1-12.
- Altmiller G, Pepe LH. Influence of Technology in Supporting Quality and Safety in Nursing Education. Nurs Clin North Am. 2022; 57: 551- 562.
- Basak D, Arrighi S, Darwiche Y, Deb S. Comparison of Anticancer Drug Toxicities: Paradigm Shift in Adverse Effect Profile. Life (Basel). 2021; 12: 48.
- Horwood C, Luthuli S, Mapumulo S, Haskins L, Jensen C, Pansegrouw D, et al. Challenges of using e-health technologies to support clinical care in rural Africa: a longitudinal mixed methods study exploring primary health care nurses’ experiences of using an electronic clinical decision support system (CDSS) in South Africa. BMC Health Serv Res. 2023; 23: 30.
- Zhai Y, Yu Z, Zhang Q, Zhang Y. Barriers and facilitators to implementing a nursing clinical decision support system in a tertiary hospital setting: A qualitative study using the FITT framework. Int J Med Inform. 2022; 166: 104841.
- Gholipour M, Dadashzadeh A, Jabarzadeh F, Sarbakhsh P. Challenges of Clinical Decision-making in Emergency Nursing: An Integrative Review. The Open Nursing J. 2025; 19.
- Cánovas-Segura B, Morales A, Juarez JM, Campos M. Meaningful time-related aspects of alerts in Clinical Decision Support Systems. A unified framework. J Biomed Inform. 2023; 143: 104397.
- Gani I, Litchfield I, Shukla D, Delanerolle G, Cockburn N, Pathmanathan A. Understanding “Alert Fatigue” in Primary Care: Qualitative Systematic Review of General Practitioners Attitudes and Experiences of Clinical Alerts, Prompts, and Reminders. J Med Internet Res. 2025; 27: e62763.
- Lu SF, Kuo YW, Hung SH, Wu CH, Wang CY, Chou SS, et al. Coping strategies of intensive care units nurses in alarm management: a qualitative research study. BMC Nurs. 2024; 23: 713.
- Li M, He S, Peng M, Liu H, Chen C, Liu X, et al. Experiences and Challenges for Critical Care Nurses in Work Related to Medical Device Alarms: A Qualitative Study. Comput Inform Nurs. 2025; 43: e01214.
- Kamel Rahimi A, Pienaar O, Ghadimi M, Canfell OJ, Pole JD, Shrapnel S, et al. Implementing AI in Hospitals to Achieve a Learning Health System: Systematic Review of Current Enablers and Barriers. J Med Internet Res. 2024; 26: e49655.
- Syrowatka A, Motala A, Lawson E, et al. Computerized Clinical Decision Support To Prevent Medication Errors and Adverse Drug Events: Rapid Review. 2024 Feb. In: Making Healthcare Safer IV: A Continuous Updating of Patient Safety Harms and Practices [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2023.
- Park Y, Bang Y, Kwon J. Clinical decision support system and hospital readmission reduction: Evidence from US panel data. Decision Support Systems. 2022; 159: 113816.