Left Ventricular Pseudoaneursym with a Bidirectional Blood Flow
- 1. Department of Cardiac MRI, Division of Cardiovascular Medicine, Allegheny General Hospital, USA
- 2. Department of Internal Medicine, Marshfield Clinic, USA
Citation
Khan MS, Shah M, Williams R (2017) Left Ventricular Pseudoaneursym with a Bidirectional Blood Flow. JSM Clin Med Imaging Cases Rev 2(1): 1008.
CLINICAL IMAGE
A 78 years old female with a history of Diabetes Mellitus and peripheral vascular disease presented with a complaint of exertional dyspnea. On TTE (Transthoracic echocardiography), a cystic structure attached to the LV (left ventricle) was noted but TTE was not able to characterize it further. CMR (cardiac magnetic resonance) imaging performed subsequently revealed a large pseudoaneurysm sac (6.3 cm x 5.4 cm) having a bidirectional blood flow, at the basal inferoseptal wall of the LV (Figure).
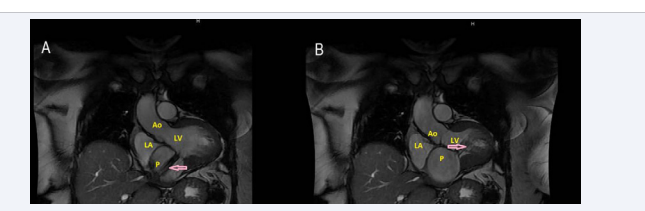
Figure 1 Panel A and B are 3 chamber views of the heart on MRI (SSFP). Pink arrow points at de-phasing protons, which indicate jet of blood. Ao: Aorta; LV: Left Ventricle; LA: Left Atrium; P: Pseudoaneurysm sac.
Jet of blood (pink arrow) is forced into pseudoaneurysm sac during systole (panel A) and exits the sac on its way back to LV during diastole (panel B). This kind of bidirectional blood flow is a feature of arterial pseudoaneurysm. Pseudoaneurysm showed post-contrast enhancement of its wall, indicating that it consisted of the pericardium.
LV pseudoaneurysm is formed if cardiac rupture is contained by the pericardium (as in our case), organizing thrombus, and hematoma [1]. Left ventricular pseudoaneurysms are most commonly caused by myocardial infarction secondary to atherosclerotic coronary artery disease [2]. Cardiac catheterization performed on this patient showed 99% mid right coronary artery stenosis. Surgical repair is recommended as the treatment of choice in suitable patients with LV pseudoaneurysms as the risk of fatal rupture is believed to outweigh the risk of surgery [3]. Later, the patient underwent CABG and pseudoaneurysm was repaired surgically.