3D Relationship of Maxillary Posterior Teeth and Sinus Floor for Immediate Extraction Implant Placement
- 1. Department of Bioengineering, Università degli Studi di Napoli Federico, Italy
Abstract
The objective of the study was to analyze the anatomical relationship between the sinus floor and the root apexes of maxillary premolars and molars to evaluate the amount of basal bone available for immediate extraction implant placement.
Study Design: Maxillary arches Cone-Beam Computerized Tomographic (CBCT) scans taken at one dental clinic were analyzed. The sub-sinusal bone height (SBH) in the premolar region was measured, in the first and second molar area the inter-radicular septum bone height (ISBH) was also measured.
Results: Six hundred (600) CBCT scans were examined. In the first premolar region the findings were: 1.5% root apex inside the sinus; in 4.9% it approximated the sinus floor; in 17.5% distance varied between 1 and 3mm; 36.4% distance between 3 and 7mm; and 39.6% >7mm. In the second premolar region the findings were: 13.9% inside the sinus; 11.8% approximating the sinus floor; 30.8% distance 1-3mm; 28.3% distance 3-7 mm; 15.1% >7mm. The first molar area showed 26.2% ISBH 7 mm. The second molar area showed 14.3% ISBH 7 mm.
Conclusion: Pre-operatory tridimensional radiological diagnosis is essential to safely insert an implant in fresh extraction sockets of maxillary premolars and molars in order to avoid complications such as sinus floor perforation.
Keywords
• Subsinus basal bone
• Immediate placement
• Maxillary sinus
• Cone-beam CT
• Membrane perforation
CITATION
Amato F (2023) 3D Relationship of Maxillary Posterior Teeth and Sinus Floor for Immediate Extraction Implant Placement. JSM Dent Surg 5(1): 1036.
INTRODUCTION
Although the use of osseointegrated implants to replace missing teeth has become a predictable procedure with high implant survival rates [1,2], success rates in the posterior maxilla are lower due to the poor quality and inadequate height of bone [3]. Furthermore, after tooth loss, the periosteum of the maxillary sinus can exhibit increased osteoclastic activity, which can cause bone resorption 4 and a resumption of the physiological sinus- floor pneumatization process [5,6].The result is a progressive reduction of the bone height. Subsinus alveolar bone height (SBH) has been defined as the distance between the floor of the maxillary sinus and the alveolar crest [7]. A lack of SBH may be treated in different ways depending on the degree of atrophy. Options include sinus lift augmentation, vertical bone regeneration of the alveolar ridge, interpositional grafting, short implants, or use of alternative sites (tuberal, pterygoid, zygoma, or tilted) [8-10]. A valid alternative to prevent post-extraction sinus-floor pneumatization and avoid the need for grafting procedures can be immediate extraction implant placement.
Several authors have advocated that one of the main criteria for achieving good primary stability with implants immediately placed in extraction sites is to engage the implant in the bone apical to the root apex [11-13].When taking this approach, however, it is essential to be aware of the amount of basal bone and the relationship between the root apex and the anatomical landmarks apical to it: the anterior part of the sinus floor for the premolars and the posterior portion of the sinus floor for the molars.
SBH has been investigated by several authors [7,14-16], using panoramic radiographs of edentulous maxillae. Other authors have used three-dimensional diagnostic tools to gather anatomical information about this area [17-21].
The aim of this CBCT study was to further investigate the relationship between the sinus floor and the root apexes in the maxillary premolar and molar area, to the interradicular bone septum height (IBSH) in the molar area, and to determine the amount of bone apical to the root apexes available for implant insertion in the posterior region.
MATERIAL AND METHODS
All the cone-beam computerized tomographic (CBCT) scans of patients with fully or partially dentate maxillary arches that were taken at a private dental. The 3D radiographical examination were obtained using a Gendex CB-500 machine. The software system was periodically calibrated and controlled. The same operator, three times for each landmark, took all the measurements and repeated each operation two times to achieve a more accurate precision. A mean value of the two measurements was carried out. Depending on the obtained bone height, the findings were distributed in five Groups for the premolars and four Groups for the molars. A percentage value of the distribution of the teeth in the corresponding Group was carried out.
Patients inclusion criteria were the following: the patients scanned had to be 20 years or older, at least two maxillary premolars and/or molars had to be present on each side, no impacted teeth or other pathology could be present in the posterior maxillary alveolar bone. Smoking was not considered an exclusion criteria.
On each scan, the measures were carried out using each the dedicated software I-Cat Vision. For the premolars the distance between the root apex and the closest point of the sinus floor was recorded: Sub-sinus Bone Height (SBH). In the molars the distance between the roof of the forcation and the closest point of the sinus floor: inter-radicular septum bone height (ISBH) was measured.
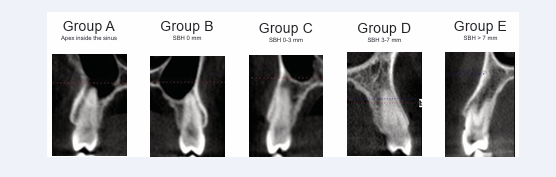
Findings for the premolars were classified into five groups: The root apex was located inside the sinus (Group A); The root apex was in contact with the sinus floor, but not penetrating in the sinus (Group B); The SBH was < 3 mm (Group C); The SBH was more than 3 mm but less than 7 mm (Group D); The SBH was more than 7 mm (Group E). Figure 1 presents examples of each of the five categories.
Figure 1: Classification in five different categories for premolars based on sub-sinusal bone height (SBH).
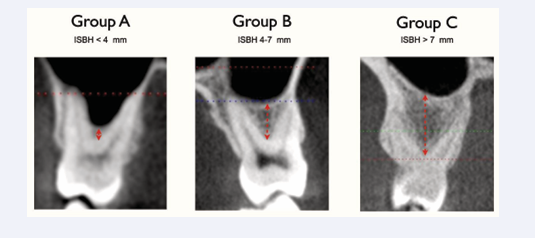
The findings for the inter-radicular septum bone height (ISBH) in the molar region were classified into three groups: ISBH < 4 mm (Group A); ISBH >4-7 mm Group B; ISBH > 7 mm Group C. Figure 2 presents examples of each of the three categories.
Figure 2: Classification in three different categories for molars, based on interradicular septum bone height (ISBH).
RESULTS
A total of 600 CBCT scans from 325 female and 275 male patients were analyzed. The patients mean age was 46. The scans included 977 first premolars. Fifteen of these belong to Group A (1.5%); 48 were in Group B (4.9 %); 171 in Group C (17.5%); 356 in Group D (36.4%), Group D); 387 in Group E (39.6%).
A total of 939 second premolars were analyzed. One hundred thirty-one of these belong to Group A (13.9%); 111 were in Group B (11.8%); 289 in Group C (30.8%); 266 in Group D (28.3%); 142 in Group E (15.1%).
Table 1 summarizes the findings for all premolars. In the molar area, a total of 1.231 first molars were analyzed, 323 (26.2%) had an ISBH of less than 4mm (Group A), 472 (38.3%) had an ISBH of 4 - 7 mm (Group B), 436 (35.4%) had an ISBH of more than 7 mm (Group C).
A total of 1.250 second molars were analyzed, 179 (14.3%) had an ISBH of less than 4mm (Group A), 578 (46.2%) had an ISBH of 4 - 7 mm (Group B), 493 (39.4%) had an ISBH of more than 7 mm (Group C). Table 2 summarizes the molar findings.
DISCUSSION
The anatomical relationship between the premolar and molar roots and the sinus floor in the posterior maxilla area is articulated and has a high individual variability [22]. Various factors influence the dimension of the sinus, including growth, function, and pneumatization. The alveolar dental process, breathing physiology, and functional changes all further contribute to the high differentiation of the maxillary sinus [23].
The position of the sinus floor is a limiting factor that influences surgical treatment and implant insertion in the posterior maxilla. The post-extraction bone remodeling and the consequent sinus pneumatization that often takes place after tooth loss can reduce the available bone crest to the level where bone augmentation procedures are necessary prior to implant placement [24].
When the vertical bone atrophy is related to the pneumatization of the maxillary sinus, elevation of the sinus floor has been suggested to enable implant placement [25]. Depending on the amount of residual bone, different bone-augmentation techniques have been proposed, including the lateral window approach described by Boyne and James (1980) and Tatum (1986) [26,27].The crestal approach, in which the Schneiderian membrane is lifted using an osteotome, was first described by Summers (1994) [28]. In both techniques, the simultaneous insertion of implants is recommended if the initial bone height is a minimum of 4 to 6 mm [29]. Otherwise, a delayed insertion is preferred [30].
While sinus augmentation has been demonstrated to be a predictable technique for increasing bone height in deficient posterior maxillary ridges prior to implant placement, the mean survival rates of implants placed in sinus-grafted areas are lower than those of implants placed in native bone after functional loading [31-33]. Some recent studies have compared the survival rates of standard length implants (more than 8mm) in lifted sinus versus the use of short implants (≤8mm). These studies have clearly demonstrated comparable survival rates between longer implants in grafted sinus and extra short implants, but higher biological complications when a sinus lift was performed, sinus membrane perforation can occur more frequently in the augmented sinus than for extra short implants [34,35]. In order to reduce the complications, the surgical time, the costs and the morbidity the use of extra short implants can represent a valid surgical treatment if a correct and scrupulous cases selection is performed [36,37].
A valid alternative to prevent post-extraction alveolar bone atrophy and thus avoid the need for grafting can be immediate extraction placement [38]. The immediate extraction placement technique has become a common procedure for replacing hopeless teeth. Its major advantage is to reduce the duration and invasiveness of the treatment [39-41], yielding higher patient-satisfaction levels than delayed implant placement [42]. Immediate implant placement in the esthetic zone has become a therapeutic first choice for clinicians [43], while in molar regions,some difficulties must be overcome. The predictability of the post-extraction implant surgery in such sites depends upon the close approximation of the bone walls to the implant surface as well as the bone density, quality, and availability [44]. Some have argued that in order to achieve good primary stability at the time of immediate extraction placement, the bone apical to the root apex or the interradicular bone in case of multi-rooted teeth should be engaged by the implant threads [11-14].
The crestal extension of the maxillary antrum and its relationship with premolar and molar roots can be a limiting factor for immediate extraction implant placement. The available basal bone between the roots apexes and floor of the sinus can only be precisely measured after a three-dimensional diagnostic examination [45]. The present study demonstrates that in the first premolar area in about 25% of the cases there is little (< 3mm) or no bone apical to the root apex to engage with the implant to achieve primary stability. In the second premolar area, this percentage increases to more than 60% of the cases. Thus, care should be taken when immediate extraction placement is performed not to extend the osteotomy beyond the root apex in order to avoid sinus perforation. As a consequence selecting an implant with a diameter coherent or larger than the actual mesio-distal size of the alveolus could be a valid choice to achieve immediate mechanical stability after tooth extraction.
In the molar area the inter-radicular septum has been indicated as the ideal site for implant insertion both for mechanical stability and for the prosthetic axis [46].Thus the dimension of the septum represent a key factor for successful immediate implant placement.
The results of this study indicate that more than 60% of the first and second molars had an ISBH of less than 7mm, as a consequence immediate extraction placement in the inter radicular bone septum of molars in most of the cases should be performed applying a sinus elevation with the crestal approach (osteotome technique) or using ultra-short implants in order to minimize the risks of sinus-membrane perforation.
In all the CBCT scans that were analyzed, the distance between root apexes and maxillary sinuses was least for all the second premolars and first molars. This finding was not uniform, however, because of the anatomical variability of sinus growth.
One of the notable anatomical characteristics was the symmetry of the anatomical conditions in either side of each patient’s mouth, both in the premolar and in the molar areas. This can probably be explained by the equivalent development of sinus pneumatization on both sides of the mouth and the fact that the premolar and molar roots on each side of any person’s mouth tend to be the same shape and length.
CONCLUSION
The results of this study show that in about 25% of the first premolar cases there is a close proximity between the root apexes and the inferior border of the sinus floor that would not allow for apical stabilization in the basal bone of an immediate extraction implant. The same condition was found in more than 55% of the cases in the second premolar region. A valid alternative to achieve immediate implant primary stability could be to use a wide diameter implant to engage the mesial and distal walls of the alveolar socket. In the molar area both the first and second molar showed in more than 60% of the cases an inter-radicular septum bone height inadequate to insert a standard length implant. Alternatively, when immediate extraction implant placement is being carried out, the use of short implants or the use of osteotomes, rather than burs, to deepen the apical part of the osteotomy and elevate the sinus floor may be indicated to minimize the risk of membrane perforation and allow for standard length implant placement.