Ameloblastoma in Black Africans the Need for Multi-National Collaborative Research
- 0. Department of Oral and Maxillofacial Surgery, Faculty of Dental Sciences, University of Lagos, Lagos, Nigeria
- 0. Department of Oral and Maxillofacial Pathology, Faculty of Dentistry, University of the Western Cape, Cape Town, South Africa
- 0. Department of Oral and Maxillofacial Surgery Pathology and Radiology, Faculty of Dental Sciences, University of Nairobi, Nairobi, Kenya
Abstract
This paper highlighted the peculiar clinical presentation of ameloblastoma in Black Africans. The recent reports of mutations associated with this tumour were highlighted. The authors proposed the formation of an African Ameloblastoma Research Network (AARN) to further explore mutations that may be peculiar to this population and may have diagnostic or therapeutic applications.
Keywords
• Unicystic
• Peripheral
• Malignant and cassic intraosseous (solid-multicystic)
Citation
Arotiba GT, Hille J, Guthua SW, Adeola H, Odhiambo W, et al. (2017) Ameloblastoma in Black Africans the Need for Multi-National Collaborative Research. JSM Dent Surg 2(2): 1014.
INTRODUCTION
Ameloblastoma is a relatively uncommon locally infiltrative benign odontogenic tumour with a rare capacity to metastasize. [1-4]. It is the most common odontogenic tumour in Black Africans [5-8]. From a prognostic view point, four clinical types of this tumour are recognized [9].
unicystic,
peripheral,
malignant and
classic intraosseous
The various histologic patterns of the classic intraosseous ameloblastoma (follicular, plexiform, acanthomatous, granular cell, basal cell, squamous metaplastic, clear cell) have not been conclusively proven to influence its biologic behavior [7-12]. The World Health Organization (WHO) classified Ameloblastoma into solid/multicystic, peripheral, desmoplastic and unicystic types with implications for treatment [13].
Early studies of these tumors in Black Africans suggested that it may be more common in this population than in Caucasians [14-16]. This was initially doubted by Mosadomi because of lack of statistically valid calculations [17]. However, Shear and Singh [18], and Sawyer et al. [19], have since provided statistical evidence that this tumour is more common in Black Africans. However, this was again refuted by Oginni et al. [18], in a multicentre Nigerian study in 2015. It is debatable if Oginni et al., conclusion can be regarded as valid in view of the poor health care infrastructure in Nigeria. This is because for every patient that presents in a tertiary referral center for treatment there are many who remain untreated in the rural areas as a result of poverty and poor health insurance coverage.Peculiar presentations of this tumor in Black Africans include [19-21].
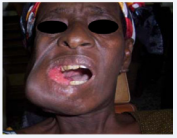
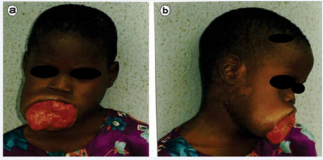
Late presentation with massive tumors [19-21] (Figures 1-4).
Figure 1: Late presentation with massive tumors in 2 young Nigerian ladies.
Figure 2: Late presentation with massive tumors in 2 young Nigerian ladies.
The high proportion of patients who are below 20 years at diagnosis [19-21] (Figures 1-4).
The high predilection for involvement of the symphysial region of the mandible [19-21] (Figsures 3 and 4) and The low proportion of the unicystic morphologic type [19- 21].
Figure 3: Ameloblastoma involving the central part of the mandible in a young Nigerian Note the thinned out mucosa over lying the tumour.
Figure 4: Recurrent mandibular classic intra osseous ameloblastoma invading the temporal fossa region about to burst through the skin. Note the pustule-like presentation. Is any tissue immune to the expansive and invasive growth of this tumour?
OBJECTIVE
The objective of this paper is to highlight the peculiar clinical presentation of ameloblastoma in a resource challenged economy (Nigeria) and propose new directions for collaborative research.
Growth Characteristics and Biologic Behavior of Ameloblastoma: Ameloblastoma has a high capacity to infiltrate the inter-trabecular spaces of cancellous bone without immediate resorption of the bony trabeculae. 22 Therefore, cancellous bone that appears clinically and radio graphically normal may contain tumour cells. 22 Marx et al. [22], demonstrated tumour cells 2.3 -8.0mm beyond apparently normal radiographic margin. However, Gortzak et al. [23], reported the maximum invasive depth in cancellous bone for large mandibular ameloblastomas to be 5mm. Marx et al 22 also reported that ameloblastoma cells can seed during surgery; an unusual attribute of a histologically benign neoplasm. He reported a case of infra temporal recurrence 10 years post enucleation and curettage of a mandibular tumor. Remarkably there was no recurrence in the posterior mandible from which the tumor was enucleated previously.
Gold [24], highlighted the following similarities in the growth characteristics and biologic behavior of this tumour and basal cell carcinoma:
1. A slow infiltrative growth
2. A high capacity for destruction of bone and soft tissues
3. Recurrence when incompletely removed
4. Ability to metastasize
5. A variety of histologic patterns
6. An epithelial origin
Late presentation of patients because of poverty/lack of health insurance/poorly developed health infrastructures gives practitioners in poor developing countries a unique insight into the growth characteristics and biologic behavior of this benign tumour [14-19] (Figures 5-8).
Figure 5: Recurrent mandibular ameloblastoma in a 27 year old Nigerian lady invading the skin along the old scar line. Post mandibulectomy, post iliac crest reconstruction. (recurrent interval= 14 years).
Figure 6: Recurrent classic intraosseous ameloblastoma Presenting as an intra oral mass 6 years post mandibulectomy with reconstruction plate fixation (note the granular, non-bleeding surface
Figure 7: Late presentation of mandibular classicintra osseous ameloblastoma in a child presenting as oralmass after breaking through its periosteal barrier –note the granular, non-bleeding surface.
Figure 8: Anatomic classification of Classic Intraosseous Ameloblastoma as a guide to management.
What is the optimal treatment modality for Ameloblastoma?
Despite extensive literature on the site prevalence, histologic and radiologic features, the optimal surgical management of this tumour is still being debated [25,26]. While conservative surgical treatment is associated with high recurrence rates (75-90%), radical surgical treatment is associated with increased morbidity, functional and aesthetic impairments [27,28]. Different approaches to surgical management have been advocated based on the growth characteristics and biologic behavior of this tumour [25-28].
Arotiba et al. [29], highlighted the Biologic, Anatomic and Clinical considerations that may influence the surgeon’s selection of conservative or radical treatment modalities. The authors also proposed an anatomic classification system for this locally aggressive tumour (Figure 9).
Figure 9: Mandible to maxilla recurrence of the classic intraosseous ameloblastoma in two Nigerians with intracranial involvement.
Late presentation and poor follow up: As a result of poor health facilities, poverty/lack of universal health insurance poor healthcare infrastructure, patients usually present late with massive tumours necessitation extensive resections, reconstruction and rehabilitation [14-19] (Figures. 1-4). It is this late presentation that gives practitioners in poor developing countries unique insights into the biologic behaviour of this tumour [14-19] (Figures 5-8). Several authors have also reported the poor compliance with postoperative follow up appointments15, 16. This may also be partly responsible for the long recurrence intervals reported in the literature from SubSaharan Africa [30].
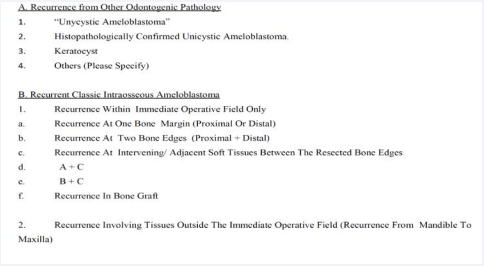
RECURRENCE
Recurrences can occur several years after primary surgery. The longest interval in the literature is 49 years [31]. Arotiba et al. [30], reported a clinico-pathologic analysis of 30 recurrent ameloblastoma managed by different surgeons at 3 tertiary referral centers in Nigeria. Based on the clinico-pathologic analysis of the cases, the authors proposed a classification system for “recurrent” ameloblastomas (Figures 9). This report also highlighted the following unique features of recurrent ameloblastoma in a healthcare resource-challenged environment [31]. The major significant findings of this study include:
1. Most primary jaw sites corresponded to the recurrent sites using Arotiba et al. [29], anatomic classification system. This is a reflection of inadequate primary surgery taking into consideration the growth characteristics and biologic behavior of this tumour
2. Most recurrences were in patients aged 20-29 years. The average age reported for ameloblastoma in Nigerians is 30 -39 years. This is a pointer to the fact that these patients probably had their tumors at a relatively young age.
3. Enucleation resulted in a 30% recurrence rate while Hemi-mandibulectomy resulted in a 20% recurrence rate. This may be a reflection of inadequate inclusion of safe margins of adjacent normal tissues (bone, periosteum, mucosa and skin) in the resection. It may also be due to seeding of tumor cells during surgery for massive ameloblastoma as frequently encountered in Nigerian patients as a result of poor healthcare infrastructure. The authors advocated the development of frozen section control in bone.
4. Majority of the recurrences occurred within 5-9 years postoperatively. Frequent (6 monthly) postoperative reviews are recommended within the first 10 years. Thereafter, follow-up reviews should be instituted at 1-2 years interval for a further 10-30 years.
5. Mandible to Maxilla recurrence (with no evidence of recurrence at the previously operated mandibular site- usually c4 tumors) is an ominous clinical progression with potentially fatal end result as a result of invasion of orbit, skull and brain (Figures 9-11).
Figure 10: Mandible to maxilla recurrence of the classic intraosseous ameloblastoma in two Nigerians with intracranial involvement.
Figure 11: Inaugural meeting of African Ameloblastoma Research Network (AARN)
Left to right: Dr Henry Adeola (Capetown, South Africa), Prof Godwin T Arotiba (Lagos, Nigeria) and Prof Jos Hille (Capetown, South Africa) 30th June, 2014.
6. This study validated Arotiba et al. [29], anatomic classification system for “primary” ameloblastoma. The most common anatomic location for primary ameloblastoma that recurred was c4 (disarticulation resections).
FURTHER RESEARCH
It is known that inherited polymorphisms of key genes may affect function and contribute to increased risk of tumour formation [32]. Identifying genes that are up or down regulated in tumour may provide important insights into key molecular changes involved in the pathogenesis of the tumour [33,34].
Knowledge gained through tumour gene expression profiling may facilitate early detection of aggressive tumours, identification of prognostic markers and targeted therapeutic interventions [35,36].
The molecular landscape of ameloblastoma has remained largely unexplored until recently probably because of its benign presentation and its low prevalence. In 2014, insights into the molecular genetics of this tumour was simultaneously reported by Kurppa et al. [37], Sweeney et al. [38], and Brown et al. [39], and could be classified into 3 groups:
1. Mitogen Kinase Activating Pathway (MAPK) activationBRAF, KRAS, NRAS AND HRAS
2. HEDGEHOG pathway activation-FGFR2 and SMO
3. Rare mutations –PIK3CA, SMARCBI, CTNNBI
It is also noteworthy that Sweeney et al. [38], reported that both Ameloblastoma and basal cell carcinoma have activating SMO mutations (Hedge-Hog pathway). This is in consonance with the previous clinical similarities highlighted by Gold [24], and may be an indication that the biologic behavior of tumors may be partly influenced by the type of mutations that initiated the tumor.
Heikinhemo et al. [40], highlighted novel molecular targets and the pathways to the development of personalized medicine for the treatment of ameloblastoma. However, the efficacy of these novel drugs is still suboptimal as a result of a combination of factors [41].
1. intra-tumor heterogeneity
2. difficulty in accurately reproducing the tumour microenvironment in vitro
3. cell culture dependent effects
Multi-center, multinational collaborative research into this tumor in Sub-Saharan Africa is desirable to explore the molecular landscape of this tumour in Black Africans. This may lead to the discovery of unique mutations which may be useful in the development of population based preventive interventions and targeted therapeutic interventions for massive tumors whose treatment may require multi-staged surgeries and reconstructions with residual facial deformity. The African Ameloblastoma Research Network (AARN) is being proposed between Lagos, Nigeria, Cape Town South Africa and Nairobi, Kenya.
AFRICAN AMELOBLASTOMA RESEARCH NETWORK (AARN)
At an Inaugural professorial lecture on 4th January, 2012 at the University of Lagos, Lagos, Nigeria it was proposed that the Ameloblastoma and Facial Deformity Foundation (AFDF) be inaugurated as a vehicle to harness funds for the management and rehabilitation of indigent patients affected by this tumor in Sub-Saharan Africa [42]. The foundation will also seek to support research into gene mutations in this tumor Black Africans. The inaugural meeting of African Ameloblastoma Research Network (AARN¬) took place in Cape Town, South Africa in June 2014after the International Association for Dental Research meeting in Cape Town South Africa (Figure 11). This will be a collaborative effort between Lagos Nigeria, Cape Town, South Africa and Nairobi Kenya. The websites for both AFDF and AARN will be active soon. International collaborations with researchers from advanced economies and other continents are most welcome.
AARN will be a network of Oral & Maxillofacial Surgeons, Oral and Maxillofacial Pathologists, Bio-Statisticians and Molecular biology/genetics experts in each of the constituent centers / countries. The minimum team number will be 5.
Objectives of AARN
1. To investigate gene mutations associated with Ameloblastoma in Black Africans
2. To identify possible diagnostic, prognostic and therapeutic targets.
3. To initiate an Ameloblastoma and Facial Deformity Foundation (AMELOFADEFO) to improve diagnosis, treatment and rehabilitation of patients with this tumor.
CONCLUSION
There is need for further research into the mutational landscape of this benign but locally aggressive tumor in Black Africans and other racial groups in different parts of the globe. Multinational, multicenter collaborations in Sub-Saharan Africa is required. International collaborations will be highly welcomed.
REFERENCES
1. Robinson HBG: Ameloblastoma: A survey of 379 cases from the literature. Arch Path. 1937; 13: 831-843.
6. Odukoya O. Odontogenic tumors: analysis of 289 Nigerian cases. J Oral Pathol Med. 1995; 24: 454-457.
19. Sawyer DR, Mosadomi A, Page DG, Svirsky JA, Kekere-Ekun AT. Racial predilection of ameloblastoma? A probable answer from Lagos (Nigeria) and Richmond, Virginia (U.S.A.). J Oral Med. 1985; 40: 27-31.
20. Arotiba GT, Ladeinde AL, Arotiba JT, Ajike SO, Ugboko VI, Ajayi OF. Ameloblastoma in Nigerian children and adolescents: a review of 79 cases. J Oral Maxillofac Surg. 2005; 63: 747-751.
23. Gold L: Biologic behaviour of ameloblastoma Oral Maxillofac Surg Clin N Amer1992; 3: 21-71.
41. Arotiba GT. The Society, Ivory Tower, Mouth and Jaw and Face Surgery in a Developing Economy. University of Lagos Inaugural Lecture Series. University of Lagos Press 2012; 63.