Dental Compression Syndrome
- 1. American Academy of Implant Dentistry, USA
Abstract
Ironically, the controversies and confusion regarding occlusion have not influenced the way dentists restore the mastication system, but they have been a major distraction to focusing on the most insidious threat to the health and integrity of the system itself, vertical parafunction.
Vertical parafunction, aka; clenching, dental compression syndrome or DCS, averages 200 pounds per square inch, capable of 1,000 pounds per square inch, lasts twice as long as bruxism, has a multitude of etiological agents, and specifically focuses on the temporomandibular joint (TMJ). Clenching, unlike bruxism, cannot be managed by the practitioner.
KEYWORDS
- Dental Compression Syndrome
- Occlusion
- Vertical parafunction
- Temporomandibular joint
CITATION
Gene McCoy DDS (2024) Dental Compression Syndrome. JSM Dent Surg 6(2): 1044.
INTRODUCTION
Ironically, the controversies and confusion regarding occlusion have not influenced the way dentists restore the mastication system, but they have been a major distraction to focusing on the most insidious threat to the health and integrity of the system itself, vertical parafunction.
Vertical parafunction, aka; clenching, dental compression syndrome or DCS, averages 200 pounds per square inch, capable of 1,000 pounds per square inch, lasts twice as long as bruxism, has a multitude of etiological agents, and specifically focuses on the temporomandibular joint (TMJ) [1]. Clenching, unlike bruxism, cannot be managed by the practitioner.
While the condyles of bruxers seem to slide past the menisci, the condyles of DCS patients target them directly resulting in trauma and displacement. Early intervention was to replace these cartilaginous discs with Teflon coated implants. The results were disastrous resulting in the recall of 25,000 TMJ implants. The horror stories detailed patients who were suicidal, barely functional, under heavy pain medication with one implant ending up in the brain: the cause-clenching [2].
Clenching however, does not always result in TMD. Susceptibility might be compared to Carpal Tunnel Syndrome; not everyone who types is affected. It depends on the patient’s biological resistance and resiliency. Imagine patients compressing their teeth every single day with a force of 200 pounds per square inch; it’s going to take its toll. Since it occurs while awake it is the patient’s responsibility; however, it is our mandate to recognize the signs and consul each affected patient.
DCS is classified as a syndrome because of the unique deformations that it creates:
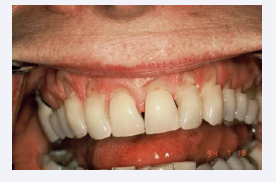
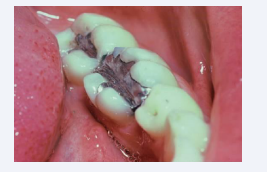
Non-Carious Lesions (NCLs)
These deformations, aka sets, are multi-shaped examples of hard tissue fatigue due to compression failure. Fatigue applies to changes in the properties of a material due to repeated applications of stress or strain-in this case, compression failure from DCS. If an object, such as a tennis ball, rebounds to its original shape after repeated compressions, it is said to be elastic in nature. However, if an object exhibits residual defects after repeated compression, it is said to be plastic in nature. Biological structures, such teeth and bone are termed viscoelastic and are subject to deformation. Engineers refer to this type of fatigue as corrosion fatigue (Figure 1) [3].
Figure 1: Non-Carious Lesions (NCLs)
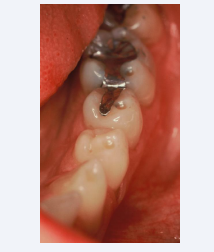
The Cupola
The most common compression NCL is a perfectly rounded depression Aka; occlusal dimples, found at the tips of functional cusps (Figure 2).
Figure 2: Occlusal dimples, found at the tips of functional cusps
Nothing of significance has been written about them except that they are associated with compression. Although the cupola contrasts dramatically in geometric design with the wedge shaped NCL, there are two striking similarities, i.e., they are both site specific in that they are found at sites of high stress on teeth, and they exhibit a glassy sheen.
Kornfeld wrote about this phenomenon in 1932 when he observed that these defects were hard, smooth, and glasslike in appearance [4]. The author suggests that this glassy effect is due to the exit of positive ions produced by the compression of appetite crystals in the dentition and the alveolar bone [5], due to a piezoelectric effect. The result is a mechanical deformation due to positive ions being emitted through these focal points of high stress which explains the glassy effect and the loss of tooth structure as well. It is not unusual to find these glassy concavities on the first molars only as they appear first in the transgression from deciduous to secondary dentition and receive the full force of compression which is reduced with the emergence of the remaining dentition.
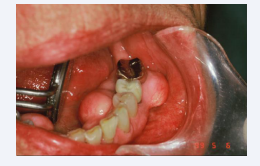
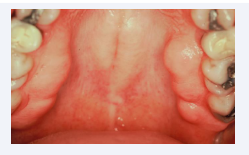
Deformation of Bone – Exostosis
Articles on torus palatinus and torus mandibularis have appeared since 1814 [6]. Although there is no consensus as to their etiology, many associate their occurrence with TMDs and masticatory hyperfunction [7]. Specifically, the negative ions generated from the compression of appetite crystals are responsible for the aggregates of new bone growth. This may well explain the metallic taste that people experience from time to time (Figure 3,4).
Figure 3: Deformation of Bone – Exostosis
Figure 4: Deformation of Bone – Exostosis
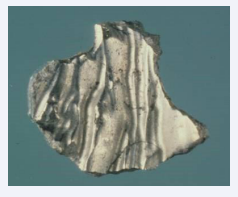
Deformations of Restorative Materials
Fatigue easily manifests itself in prostheses and restorative materials such as amalgam and acrylic. Termed Luder Lines or molecular slip bands, the molecules in the alloy are rearranging themselves under the influence of compressive strain (Figures 5 and 6). One can demonstrate the effect by bending a metal coat hanger back and forth and examining the stress configuration that is produced [8].
Figure 5: Deformations in acrylic
Figure 6: Deformations in acrylic
Fatigue in Acrylic appears as wavy lines or sets (Figures 7 and 8).
Figure 7: Fatigue in Acrylic appears as wavy lines or sets
Figure 8: Fatigue in Acrylic appears as wavy lines or sets
The deformations in the oral environment are important diagnostic tools, but their appearance does not mean that the patient is currently affected with DCS, as it may have been from a prior stressful period in their lives.
CONCLUSIONS
Disorders of the TMJ affect 61 million Americans; the most likely etiological factor aside from trauma, parafunctional forces generated from grinding (bruxism) and clenching (DCS) of teeth. While bruxism can be managed with a guard; DCS cannot. Dentists can only monitor for its signs and advise patients as to the many etiological factors that may initiate its onset.
DCS is a formidable threat to implant reconstructions due to the reduced volume of alveolar bone which is beneficial in dispersing parafunctional forces when clenching does occur. Reactively relying on occlusal schemes to minimize these forces is secondary to proactively elevating patient’s awareness.
REFERENCES
- Paesani DA. Bruxism, Theory and Practice, Quintessence Publishing Co. Ltd. 2010, United Kingdom.
- Medical Mess, Implant in Jaw Joint Fails, Leaving Patients in Pain and Disfigured. Wall Street J. 1993.
- Gordon JE. Structures or Why Things Don’t Fall Down, New York: Da Capo Press. 1978; 333-334.
- Kornfeld B. Preliminary Report of Clinical Observation of Cervical Erosions. Dental Items of Interest. 1932; 54: 905-909.
- McCoy G. Dental Compression Syndrome and TMD, Examining the Relationship. Dent Today. 2007; 7: 118-123.
- Seah YH. Torus Palatinus and Torus Mandibularis: A Review of the Literature. Aust Dent J. 1995; 40: 318-321.
- Sirirungrojying S, Songkhin DKH. Relationship between Oral Tori and Mandibular Disorders. Int Dent J. 1999; 49: 101-149.
- McCoy G. Occlusion Confusion, A lecture presented at Peking University School of Stomatology, Beijing, China. 2010.