Digitally Designed Zirconia Hardy Cutters
- 1. US Army Prosthodontics Residency, US Army, USA
Abstract
This case report demonstrates the conversion of a traditional hardy cutter denture into a new milled denture with a more esthetic zirconia hardy cutter. Hardy cutter denture teeth provide increase-chewing capability for denture wearers but are considered non-esthetic by many due to the show of metal. By utilizing digital dentistry and zirconia to fabricate denture teeth with a Hardy Cutter chewing surface a more esthetic option can be offered to the patient who desires increased functional capability with a removable prosthesis.Conclusion: Pre-operatory tridimensional radiological diagnosis is essential to safely insert an implant in fresh extraction sockets of maxillary premolars and molars in order to avoid complications such as sinus floor perforation.
Keywords
• Dentures
• Hardy Cutter
• Occlusion
• Removable Prosthodontics
• Zirconia
CITATION
Ryser AS, Sabol J, Walworth P (2024) Digitally Designed Zirconia Hardy Cutters. JSM Dent Surg 6(1): 1037.
INTRODUCTION
Complete dentures may be designed with a variety of occlusal schemes and denture teeth to include anatomic, semi-anatomic, and non-anatomic forms. Denture teeth have been made from porcelain, acrylic, or with metal components incorporated into the occlusal surfaces. The first documented example of a metal occlusal denture tooth was in 1938 with Dr. Charles Wharton’s metal Chewers (Engelmier) [1].This design promoted improved cutting efficiency, allowed for unrestricted movement of the mandible in all directions, and reduced food entrapment. In 1942, Dr. Charles Prange patented a metal insert for acrylic teeth in order to have a lighter product with better penetration of food and resistance to wear. The Hardy Cutter tooth form incorporates metal on the occlusal surface to improve cutting efficiency but may not be desired in patients with high esthetic demands due to the unsightly grey metal occlusal surface. According to a literature review by Waliszewski in 2005, esthetics is the predominant factor in complete denture success and patients are more likely to be happy with their dentures when esthetic decisions were made by the patient [2].
Monoplane occlusion is often used in complete dentures when the patient presents with a severely resorbed alveolar ridge or when there is difficulty obtaining an accurate centric relation record. However, according to Clough et al., there is a reduced chewing efficiency with monoplane occlusion and 67% of patients prefer a lingualized occlusal scheme when compared to a monoplane occlusion [3]. Wear of acrylic denture teeth is common and can result in loss of the vertical dimension of occlusion, loss of masticatory efficiency, defective tooth relationships, andmasticatory muscle fatigue [4]. In a study by Cha et al., it was shown that PMMA denture teeth opposing a zirconia antagonist provided adequate wear resistance and maintained a relatively smooth service [4]. Weighted mandibular dentures have been utilized in patients with severely resorbed alveolar ridges to aid in retention of the denture and internal weights can be used when the alveolar mucosa cannot support a metal base [5].This case report illustrates the use of an esthetic alternative to metal occlusal cutting surfaces on complete dentures and the additional weight of the zirconia brings improved stability to the mandibular denture, contributing to meeting the patient’s esthetic and functional concerns.
MATERIALS AND METHODS
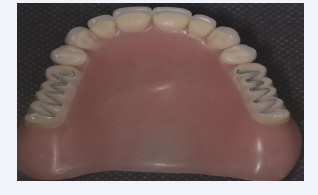
A 93-year-old patient presented with a chief complaint of, “I don’t like how these dentures look and I would like white teeth.” The patient’s current prosthesis had recently been fabricated using the neutral zone technique and cameo surface impressions in order to improve denture stability on the minimally existing residual ridge. The patient was satisfied with the fit of the current prosthesis and had a long history of using Hardy Cutter teeth but was interested in a more esthetic option. In order to facilitate the fabrication of a new prosthesis using the existing prosthesis as a guide, the maxillary and mandibular complete dentures were scanned using 3shape Digital Denture Designs to capture the intaglio, cameo, and occlusal surfaces. New maxillary and mandibular complete dentures were fabricated using milled polymethyl methacrylate (Ivoclar Ivotion, Ivoclar Vivadent) and finished to completion. The patient previously had a maxillary complete denture fabricated with Hardy Cutter teeth (Figure 1).
Figure 1: Pre op complete denture with hardy cutter
To add additional weight to the mandibular denture to aid in retention, zirconia Hardy Cutter teeth were fabricated for the new prosthesis.
The occlusal surface of the mandibular denture was altered to remove all posterior teeth and a trough of 3 mm by 5 mm was made into the denture base (Figure 2).
Figure 2: Modified complete denture.
A new occlusal surface was designed (Imagine Exocad Digital Dental Software) incorporating a flat occlusal plane and a ribbon of elevated zirconia across the occlusal surface approximately 1mm in width and height. The intaglio surface of the zirconia was extended approximately 5 mm as a retentive element for placement into the acrylic denture base. The zirconia restorations (Katana Zirconia HT) were milled, sintered, and polished (Figures 3 and 4).
Figure 3: Green state zirconia Hardy Cutters.
Figure 4: Sintered, polished, and glazed zirconia Hardy Cutters.
Areas to be cemented were air abraded with aluminum oxide (50mm particle size at 2 bar), steam cleaned, primed using Monobond Plus (Ivoclar Vivadent) and cemented to the mandibular denture using auto cure Multilink hybrid abutment cement under pressure for 7 minutes (Ivoclar Vivadent) (Figures 5 and 6).
Figure 5: Pre-cementation.
Figure 6: Cemented zirconia Hardy Cutters.
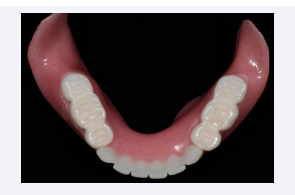
A clinical remount was performed to refine the occlusion. As this new prosthesis was a duplicate of her existing successful prosthesis except for the new mandibular occlusal surface, minimal adjustments were necessary upon delivery and recall (Figure 7).
Figure 7: Final Dentures
The patient reported satisfaction with the esthetics of the dentures and function and stated she was able to successfully chew caramel and eat steak with her new dentures.
DISCUSSION
Extensive mandibular ridge resorption has a significant effect on the retention, resistance, and stability of a complete denture. Considerable time for the patient and dentist is consumed using the neutral zone and cameo surface impressions to improve masticatory function of the prosthesis. Use of Hardy Cutter denture teeth in patients is another means to improve the success of a complete denture due to the lack of lateral forces during mastication or parafunction. However, the metal occlusal surface may be considered unesthetic. An advantage of the CAD/ CAM zirconia denture teeth with occlusal cutting ribbons is that it maintains the unique cutting surface but without the grey metal on the occlusal surface. The additional weight of the zirconia restorations further improves of the retention of the mandibular prosthesis. Potential disadvantages include the time needed to design the zirconia restorations, additional processing of the prostheses, possible delamination of the zirconia restoration from the denture base, and complexity of adjusting the zirconia occlusal surface. Contraindications for this type of restoration would include using a prosthesis that was not successfully worn by the patient and therefore, a new denture would need to be initiated instead of using a previously successful prosthesis.
CONCLUSION
Excessive resorption of the residual ridge in completely edentulous patients creates a significant functional problem for the complete denture patient. Esthetic concerns should not be discarded when improved function is desired. Classic denture tooth designs such as that of the Hardy Cutter and utilizing the cutting blade philosophy with contemporary materials can result in a successful esthetic and functional result. This case reports demonstrates converting a traditional denture technique into a more esthetic outcome using digital dentistry and zirconia.
ACKNOWLEDGEMENTS
Study supported by US Army Prosthodontics Residency Fort Eisenhower, GA