Horizontal Alveolar Dimensional Changes in Single Molar Post-Extracion Sites: A Clinical Study
- 1. Studio Associato Dr. Saverio e Francesco Amato, Viale Alcide De Gasperi, Italy
Abstract
Purpose: The aim of the study is to evaluate the bucco-lingual volumetric tissue change that occurs in the 6 months time frame following flapless single-tooth extraction in the molar area without placing any filler in the alveolus. Materials and
Methods: Patients in need of an extraction of a first or second molar in the mandible or maxilla were consecutively recruited. Immediately before the extraction (Baseline) and two, four, and six months after extraction an alginate impression of the area was taken and immediately poured with orthodontic gypsum. The bucco-palatal dimension (BPD) was measured with an electronic caliper on the study casts at 1 mm, 3 mm, and 5 mm apical to the free gingival margin and the horizontal volumetric changes were compared between baseline and two, four, and six months post-extraction.
Results: A total of 65 patients were examinated. Changes in the mean horizontal ridge dimension were recorded. After 6 months the BPD diminished at 1 mm, 3 mm and 5 mm distance from the free gingival margin respectively of 5.91 ± 0.158 mm (p-value <0.01), ( - 52.13%), 4.68 ± 0. 178 mm (p-value <0.001) (- 47.07%), and 3.75 ± 0.178 mm (p-value <0.001) (- 37.81%).
Conclusions: The observed volumetric soft tissue changes appeared to affect significantly the original bucco-lingual alveolar dimension in the 6 months short term follow-up after single tooth extraction in the molar area.
Keywords
• Molar site; Post-extraction remodeling; Flapless surgery; Dimensional changes
CITATION
Amato F (2024) Horizontal Alveolar Dimensional Changes in Single Molar Post-Extracion Sites: A Clinical Study. JSM Dent Surg 6(2): 1043.
INTRODUCTION
Replacing a single tooth with a dental implant has been demonstrated to be a predictable technique with survival rates up to 99% [1]. The most commonly used technique is the two- staged or delayed technique proposed by Bränemark in 1977. The protocol involves extracting the tooth and waiting a few months for the socket to heal prior to inserting the implant. Once implant osteointegration is achieved, a third surgery is performed to connect the healing abutment [2].
During the healing phase a significant alveolar volumetric tissue changes take place after tooth extraction [3]. The size, the volume, and the shape of the alveolar process are dictated by the roots of the teeth; after tooth extraction the alveolar bone ridge starts to remodel and as a consequence a significant decrease in the vertical and horizontal dimensions takes places. The dimensional changes mostly occur in the first 6 months after tooth extraction4. The aim of this clinical study is to measure the variation of the alveolar contour horizontal dimension at single molar extraction sites.
MATERIAL AND METHODS
Patients in need of an extraction of a first or second molar in the mandible or maxilla were consecutively recruited by one private practice clinical center between January 2021 and December 2023. Tooth extraction was performed as a consequence of decay, fracture, or endodontic failure. The main inclusion criteria was the integrity of the alveolar walls and of the inter-radicular septum. The presence of periapical lesion was not considered an exclusion criteria. Smoking also was not consider an exclusion criteria. Contraindications to surgery such as, uncontrolled diabetes and periodontal disease were considered to be an exclusion criteria. In accordance with the Declaration of Helsinki, each patient signed an informed consent form after being thoroughly informed about the risks and benefits associated with the procedure. Each patient received a complete intraoral examination and impression followed by the development of a study cast that was mounted on an articulator to measure and record the volumetric tissue changes.
Surgical Procedure
Two to three days prior to surgery, each patient was provided a professional tooth cleaning for plaque and calculus removal and prescribed a 0.20% chlorhexidine rinse three times a day for 14 days. Patients began a five-day course of amoxicillin (1 gram tablets, twice daily) starting 12 hours before surgery. Local anesthesia consisting of articaine with adrenaline (1:100.000) was induced in the vestibular and lingual area. Each tooth was extracted atraumatically using a flapless technique to preserve the blood supply of the alveolar bone plates. An odontotomy was created with a diamond burr to separate the roots and elevators were used to luxate each root that were extracted one at the time while taking care to preserve the interradicular septum and the alveolar walls. An alveolar curette was used to thoroughly debride the alveolus after tooth extraction.
The rational for not using any bone graft was to eliminate the confounding factor and to have a better standardization of the protocol among the different clinical cases (Figure 1).
Figure 1: Occlusal view of flapless fresh extraction site showing interradicular septum preservation.
Patients were instructed to stay on a soft diet for the first week following surgery. Smoker patients were instructed not to smoke for a minimum of 2 weeks after the surgery. Recall visits were scheduled every other week for the first month and once a month thereafter for the first six months. At every monthly visit, an alginate impression were taken to monitor the bucco- lingual dimension and photographs to evaluate the presence of recession and for clinical records. Patients were followed-up for a minimum of 6 months to a maximum of 1 year (Figure 2).
Figure 2: Occlusal view of 6 months post-extraction showing horizontal dimension change
Measurements
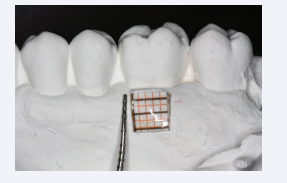
Alginate impressions were taken by the main operator and poured by the same operator within one hour to minimize the alginate distortion trying to reproduce the same conditions in each case. Impression were checked with magnified glasses 2x to verify if stretching mark or bubbles were present in which case the impressions were taken a second time. Study casts were prepared by pouring white orthodontic gypsum (Jeltrate Fast Set, Dentsply International, Milford, DE) in the alginate impressions of each treated site. The obtained study casts were used to evaluate volumetric tissue changes during healing at the following intervals: Baseline just before the extraction (T0); at the 2-month follow-up (T1); at the 4-month follow-up (T2); and at the 6-month follow-up (T3). Extraction sites on the study casts were marked at the 1-, 3-, and 5-mm levels from the free gingival margin of the buccal and lingual/palatal sides using millimeter-calibrated paper stickers (Figure 3).
Figure 3: Study cast marked with millimiter- calibrated paper sticker at the 1-, 3-, and 5-mm levels from the free gingival margin.
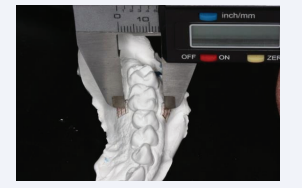
The distance between the buccal and lingual/palatal marks at each of the three levels on the casts was measured to a tenth of a millimeter using an electronic digital caliper (Aura-Dental, Location) (Figure 4).
Figure 4: Distance between the buccal and lingual/palatal marks at each of the three levels measured to a tenth of a millimeter using an electronic digital caliper
An external operator made the cast measurements using optical loupes with a headband and 2.5X magnification per eye (Orascoptic, Location). Measurements were performed by the same operator and errors were minimized by repeating three times for each landmark and time interval.
RESULTS
A total of 65 patients (25 males and 40 females) were recruited to participate in the study.
Each patients received one extraction each. A total of 65 extraction (34 in the maxilla and 31 in the mandible) were performed in single molar sites (47 first molars and 18 second molars).
The horizontal dimensional changes (BPD) at T1, T2 and T3, as measured on the study casts, were analyzed for differences between distances from the free gingival margin.
Results at six months (T3) are as follow:
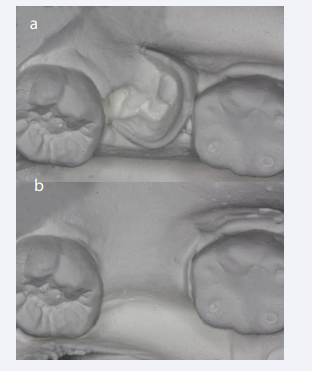
BPD diminished at 1 mm, 3 mm and 5 mm from the free gingival margin respectively of 5.91 ± 0.158 mm (p-value <0.01), 4.68 ± 0. 178 mm (p-value <0.001), and 3.75 ± 0.178 mm (p-value <0.001) (Figure 5a,b).
Figure 5: a,b: Occlusal view of the study casts at Time 0 (Baseline) and Time 3 (6 months) showing horizontal dimension tissue change.
DISCUSSION
Human maxillary bones have a large degree of anatomical variability. Studies have demonstrated that bone-density distribution values show a significant variation within subjects, within the same jaw, and between adjacent positions. In general bone density was significantly lower in women than in men; no significant correlation was found between bone density and the patient age. In conclusion bone density of patients displays significant interindividual variation [5]. When the growth is completed, the presence or the absence of teeth is the most important factor in regulating bone morphology [6]. Bone metabolism is a complex process involving physiological, functional, and structural factors [7]. After tooth extraction, the socket is filled by a blood clot followed one week later by the formation of granulation tissue with blood vessels, fibroblasts, and chronic inflammatory cells. After three weeks, the granulation tissue is replaced by collagen and new woven bone, which starts to form as trabeculae at the base and periphery of the socket that proceeds toward the center and crest [8]. Osteoprogenitor cells, pre-osteoblasts and osteoblasts surround the trabeculae. At five weeks, two thirds of the socket is filled with new bone. The epithelium requires from 24 to 35 days to completely cover the extraction site. In the first phase after tooth extraction the bundle bone is replaced with woven bone leading to a great reduction in height, especially in the buccal crestal aspect, which is constituted by bundle bone [9]. During the second phase, diffuse atrophy, decrease in blood supply, and localized inflammation determines the extent of alveolar bone remodeling with horizontal and vertical tissue reductions [10]. The resorption is more relevant in the first six months, but continues at an average of 0,5-1% per year throughout life. The molar area is the one that suffers the greatest amount of horizontal resorption [11].
Schropp et al., made measurements from a cast model and radiographs of premolar and molar extraction sites that demonstrated a 50% loss of crestal width in the first 12 month period with two thirds occurring in the first three months [12]. The alveolar post-extraction resorption may depend on multiple factors such as, soft and hard tissue biotype, tissue preservation procedures [13], flap or flapless surgery [14,15]. The buccal bone wall thickness has been identified as the most critical risk factor for bone resorption and can thus, serve as a prognostic tool for susceptible sites following tooth extraction [16]. The use of graft material to preserve the tissue volume has been deeply analyzed. Deproteinized bovine bone mineral placed into the implant-socket gap has been reported to maintain bone volume due to its slow resorption [17,18]. Raising a flap may also play a role, in fact the lack of blood supply deriving from a gingival flap elevation will promote reabsorption of bone from the surface [15,19]. Botticelli demonstrated that following flap elevation and immediate implant placement, horizontal reabsorption of the buccal wall amounted to about 56% compared to 30% for the palatal wall at 4 months [14]. Becker demonstrated that with the flapless procedure the loss of crestal width is minimal [20]. The present study compares the horizontal dimensional tissue changes that take place in the first six months in single molar sites after flapless extraction. Within the limitation of the study, the results indicate a significant presence of volumetric tissue changes.
Limitations of this study consist in its limited sample size. A more accurate way to perform measurements would have been digital scanners. Potential distortion of alginate and stone expansion could have some effect on the precision of the measurements. No differenziation between gingival and alveolar biotype was done, and the follow-up was limited to 6 months period.
CONCLUSION
The present study resulted in a significant reduction of the alveolar soft tissue dimension in the horizontal component following single-tooth extraction in the molar area. The techniques employed included flapless and atraumatic tooth removal and no graft was used. Further studies based on larger sample sizes and longer follow-up are required to validate the present findings.
REFERENCES
- Albrektsson T, Brånemark PI, Hansson HA, Lindström J. Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop Scand. 1981; 52: 155-170
- Branemark PI, Hansson BO, Adell R, Breine U, Lindström J, Hallén O, Ohman A. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scandinavian J Plast Reconstr Surg Suppl. 1977; 16: 1-132
- Valentini P, Abensur D, Albertini JF, Rocchesani M. Immediate provisionalization of single extraction-site Implants in Esthetic Zone: a Clinical Evaluation. Int J Perio Rest Dent. 2010; 30: 40-50
- Van der Weijden F, Dell’Acqua F, Slot DE. Alveolar bone dimensional changes of post-extraction sockets in humans: a systematic review. J Clin Periodontol. 2009; 36: 1048-1058.
- Di Stefano DA, Arosio P, Pagnutti S, Vinci R, Gherlone EF. Distribution of Trabecular Bone Density in the Maxilla and Mandible. Implant- Dent. 2019; 28: 340-348
- Tallgren A. The continuing reduction of the residual alveolar ridge in complete dentures wearers: a mixed - longitudinal study covering 25 years. Prosthet Dent. 1972; 27: 120-132
- Atwood DA. Postextraction changes in the adult mandible illustrated by microradiographs of mid-sagittal sections and serial cephalometric rentgenograms J Prosthet Dent. 1963; 13: 810-824
- Amler MH, Johnson PL, Salman I. Histological and histochemical investigation of human alveolar socket healing in indisturbed extraction wounds. J Am Dent Assoc. 1960; 61: 32-44
- Steiner GG, Francis W, Burrell R, Kallet MP, Steiner DM, Macias R. The healing socket and socket regeneration. Compend Contin Educ Dent. 2008; 29: 114-116.
- Araujo and Lindhe. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J Clin Periodontol. 2005; 32: 2015-2018.
- Pagni G, Pellegrini G, Giannobile WV, Giulio Rasperini G. Post extraction alveolar ridge preservation: biologic basis and treatments. Int J Dent. 2012; 2-13
- Schropp L, Wenzel A, Kostopoulos L, Karring T. Bone healing and soft tissue contour changes following single tooth extraction: a clinical and radiographic 12-month prospective study. Int J Perio Rest Dent. 2003; 23: 313-323.
- Botticelli D, Berglundh T, Lindhe J. Resolution of varying dimension and configuration in the marginal portion of the peri-implant bone. An experimental study in the dog. J Clin Periodontol. 2004; 31: 309- 317
- Botticelli D, Berglundh T, Lindhe J. Hard-tissue alterations following immediate implant placement in extraction sites. J Clin Periodontol. 2004; 31: 820-828.
- Pfeifer JS. The reaction of alveolar bone to flap procedures in man. Periodontics. 1965; 20: 135-140
- Monje A, Chappuis V, Monje F, Muñoz F, Wang HL, Urban IA, Daniel Buser. The critical peri-implant buccal bone wall thickness revisited: an Experimental study in the Beagle. Int J Oral Maxillofac Implants. 2019; 34: 1328-1336
- Araujo MG, Linder E, Lindhe J. Bio-Oss collagen in the buccal gap at immediate implants: A 6-month study in the dog. Clin Oral Implants Res. 2011: 1-8
- Sans M, Lindhe J, Alcaraz J, Sanz-Sanchez I, Cecchinato D. The effect of placing a bone replacement graft in the gap at immediately placed implants: a randomized clinical trial. Clin Oral Implants Res. 2017; 28: 902-910
- Araujo MG, Lindhe J. Ridge alterations following tooth extraction with and without flap elevation: an experimental study in the dog. Clin Oral Implant Res. 2009; 20: 545-549.
- Becker W, Goldstein M, Becker B. E, Sennerby L. Minimally invasive flapless implant surgery: A prospective multicenter study. Clin Implant Dent Relat Res. 2005; 7: S21-27