A Rare Case of Inflammatory Retrograde Peri-Implantitis Caused By Foreign Bodies
- 1. School of Dentistry, Federal University of Bahia, Avenida Araújo Pinho, Salvador/Bahia, Brazil
- 2. School of Dentistry, Uninassau, Estrada do côco, Lauro de Freitas/Bahia, Brazil
- 3. Clínica Infinity Odontologia e Medicina Estética, Rua Alceu Amoroso Lima, Salvador/Bahia, Brazil
Abstract
The aim of this study was to report a rare case of inflammatory retrograde peri-implantitis caused synergistically by two foreign bodies and associated with implant malposition. Inflammatory retrograde peri-implantitis is manifests as a clinically symptomatic periapical lesion that develops shortly after implant insertion and is characterized by bone loss around the apex of the implant caused by microbial activity, while the coronal portion shows normal osseointegration. To elucidate the presence of a bluish nodular lesion with a central pink dot located at the apex of a dental implant in the right maxilla of a female patient, clinical assessment and tomographic and histological analysis examinations were performed. The tests revealed the presence of exogenous material compatible with gutta percha and rubber mold material inside the lesion. The lesion exhibited an aggressive appearance and rapid progression that caused the loss of bone support around the implant within approximately 6 months. These findings indicated an exacerbated inflammatory lesion with a high potential for bone destruction and resorption around the dental implant, which led to the diagnosis of inflammatory retrograde peri-implantitis caused by foreign bodies. The treatment of choice was reverse torque removal of the dental implant. We highlight the need for shorter follow-up programs and periodic imaging examinations of patients with dental implants, which will permit to identify and manage the bone loss caused by inflammatory retrograde peri-implantitis in its early stages, increasing the success rate of implants and avoiding the need for explantation.
KEYWORDS
- Case report; Retrograde peri-implantitis; Apical peri- implantitis; Periapical diseases; Periapical implant bone loss
CITATION
Costa DD, de Araújo Oliveira MVC, Paty DSP, Cerqueira LS, dos Santos JN, et al. (2024) A Rare Case of Inflammatory Retrograde Peri- Implantitis Caused By Foreign Bodies. JSM Dent 11(1): 1141.
INTRODUCTION
Dental implants are the rehabilitation treatment of choice in cases of partial and complete edentulism because of their efficacy and high overall survival rate of 97.1% [1]. However, this fact does not rule out the occurrence of failures, particularly biological failures such as Inflammatory Retrograde Peri-Implantitis (RPI). The condition manifests as a clinically symptomatic periapical lesion that develops shortly after implant insertion and is characterized by bone loss around the apex of the implant caused by microbial activity [2-5], while the coronal portion shows normal osseointegration [6]. Although its etiology is still unknown, RPI might be associated with root canal infection or the presence of a periapical pathology in neighboring teeth; implant placement in areas previously submitted to endodontic treatment and with residual infection; bone necrosis caused by overheating during implant placement; installation of the implant at an infected site where residual foreign bodies or root fragments are present, and implant malposition [2-5].
Retrograde peri-implantitis develops within the first weeks after implant placement and the clinical manifestations include swelling, suppuration, or presence of a fistula [5]. The condition is classified as mild, moderate or advanced based on the amount of bone loss [6]. The treatment of RPI is defined based on its etiology (endodontic, local bacteria, osteonecrosis, or implant malposition) and on the severity and extent of the lesion [5]. Interventions are aimed at stopping disease progression and bone loss and include pharmacological (antibiotic therapy), direct mechanical (curettage and removal of the lesion), chemical (decontamination of the implant apex), and regenerative (bone grafts) approaches [7]. Explantation is performed in cases of malpositioned implants [8].
The aim of this study was to report a rare case of RPI caused synergistically by two foreign bodies.
CASE PRESENTATION
A 54-year-old female patient with controlled hypertension (50 mg losartan), with complaints of a swelling in the right maxilla that developed 6 months after immediate placement of a dental implant replacing tooth 1.3, which had been treated endodontically without success.
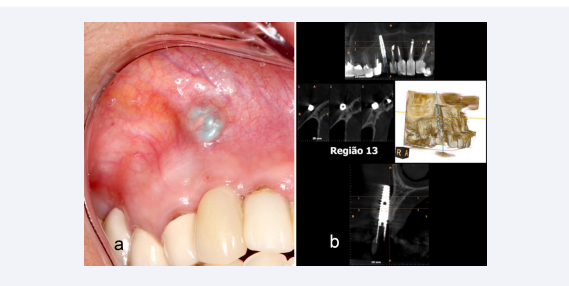
Clinical examination showed the presence of a nodular lesion of firm consistency on palpation that measured approximately 8 mm in its major diameter. The lesion was located in the mucosal layer in the apical portion of the dental implant (1.3). It had a bluish color and a central pink dot compatible with remnants of gutta percha (Figure 1a).
Figure 1 (a): Image of the nodular lesion at the apex of the dental implant (1.3). (b) Cone beam computed tomography of area 1.3 showing the dental implant without bone support throughout the buccal extension.
Cone beam computed tomography revealed a dental implant without bone support throughout the buccal extension and from the middle to the apical third of the palatal surface. A band of osseointegration was observed only in the middle to cervical third of the implant on the palatal surface (Figure 1b). Based on the clinical and imaging findings, the diagnostic hypothesis was RPI caused by foreign bodies and associated with malposition of the implant.
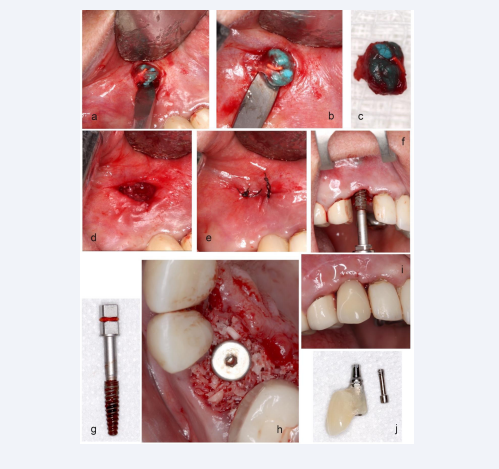
An excisional biopsy of the nodular lesion was performed, which revealed the presence of gutta percha and rubber mold material compatible with blue addition silicone (Figure 2a-2e). After exeresis of the lesion, the dental implant was removed by reverse torque (Figure 2f, 2g), followed by curettage of the surgical site and washing with saline. A new implant (Drive CM, Neodent®, Curitiba-PR, Brazil) was then placed and the remnant bone defect was reconstructed with a xenogenous graft (Bio- Oss®, Geistlich Pharma®, Switzerland) in the alveolar buccal wall (Figure 2h) and immediate installation of a temporary prosthesis. (Figure 2i, 2j).
Figure 2: (a, b, d, e) Excisional biopsy of the nodular lesion. Macroscopic examination revealed the presence of gutta percha (pink) and addition silicone (blue). (c) Collected specimen stored in 10% formaldehyde and sent for anatomopathological analysis. (f) Reverse torque explantation with retrível (g) Removed implant coupled to retrível. (h) Placement of a new implant and alveolar reconstruction with biomaterial. (i, j) Fabrication of a provisional tooth and immediate provisioning
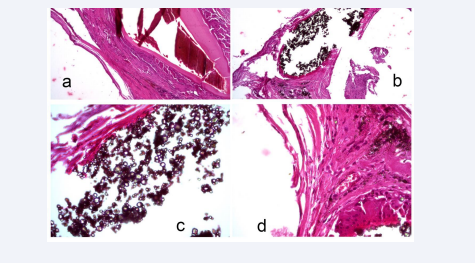
Histological analysis (Hematoxylin-Eosin, HE stain at 20x magnification) was conclusive and revealed a mucosal fragment without atypia showing a foreign body-type giant cell reaction and exogenous material (Figure 3a-3d).
Figure 3: HE stain at 20x magnification - (a) Sections containing gutta percha: mucosal fragments lined with stratified squamous epithelium without atypia whose lamina propria shows vascularized fibrous connective tissue with a foreign body-type reaction involving exogenous material. (b, c, d) Sections containing molding material: multiple empty spaces, sometimes with an irregular contour, and spaces with bluish black lumpy content surrounded by foreign body-type multinucleated giant cells, sometimes with brown central granular content surrounded by eosinophilic material also showing a foreign body-like reaction involving the exogenous material.
The association of these findings with the clinical and tomographic results indicates an exacerbated inflammatory reaction with a high potential for bone destruction and resorption around the dental implant, confirming the diagnostic hypothesis of RPI caused by foreign bodies.
DISCUSSION
To our knowledge, this is the first case report indicating the simultaneous presence of two foreign bodies and implant malposition as the probable cause of RPI, reinforcing that it is a rare condition. In contrast, previous studies have reported endodontically treated teeth and the presence of periapical pathologies in neighboring teeth as the main etiological factors of RPI [2-4,9]. Although residual foreign bodies are cited as the source of disease-causing microorganisms [2,5], none of the studies mentioned the presence of molding material or gutta percha fragments as examples of foreign bodies associated with RPI, as observed in the present case.
Furthermore, implant placement in areas submitted to endodontic treatment and at infected sites is reported to be a risk factor for RPI [2-5,10]; however, this treatment modality can be successful when curettage and washing of the socket are performed after tooth extraction, followed by immediate implant placement [11]. These maneuvers were not performed or were not successful in the present case as demonstrated by the presence of foreign body remnants at the peri-implant site that may have caused the lesion.
The prevalence of RPI is controversial but is relatively low, ranging from 0.34% to 3.8% [3,5]. However, a higher prevalence (20%) has been reported when implants are placed at sites previously submitted to apicectomy [12]. However, prevalence data are limited since only few studies are available that have used different methodologies and involved different etiologies of RPI [3,5,12] and a small sample [12]. It is believed that there is a predilection for the maxilla over the mandible [13], in agreement with the present report in which area 1.3 was affected.
In the present study, RPI clinically manifested as a nodular lesion/swelling, an appearance previously described in the literature [5], but diverged by its blue color with a central pink dot, compatible with the color of the exogenous materials transcending through the mucosa. Tomography revealed an aggressive lesion of rapid progression as indicated by the fact that it promoted resorption of the entire buccal alveolar bone wall and of the middle to apical third of the palatal surface. This radiological finding differs from the pattern described in the literature of a radiolucency surrounding the apex of the implant [2-4] but is compatible with advanced bone loss (class III), defined as bone resorption > 50% of the implant length from the implant apex [6].
Several therapeutic modalities have been adopted to treat RPI based on etiological factors. In the present case, the lesion and foreign bodies were removed; however, the aggressive evolution of the disease resulted in the loss of bone support and maintenance of only a small band of osseointegration, which justified the removal of the dental implant. These findings agree with previous studies [8,9] and with a systematic review indicating that 35.7% of cases of RPI require explantation [13]. On the other hand, in the case of smaller lesions, curettage of the lesion followed by regenerative treatment with bone grafts has been widely used [13], with reports of 100% implant survival [5] and a success rate of 75 to 90% [14]. These findings indicate that this approach is a predictable and successful treatment.
The main limitation of the present study was the fact that it was not possible to compare the findings with other studies. The literature only cites the possibility of RPI being caused by foreign bodies and scientific evidence is limited.
We highlight, in the present study, the need for shorter follow- up programs and periodic imaging examinations of patients with dental implants, which will permit to identify and manage the bone loss caused by RPI in its early stages, increasing the success rate of implants and avoiding the need for explantation.
DATA AVAILABILITY
Due to the patient’s confidentiality, only anonymous data can be shared upon reasonable request from the corresponding authors.
ETHICAL APPROVAL
The authors certify that they have obtained all appropriate patient consent forms according to the Helsinki declaration. The patient gave informed consent for his images, radiographic examinations, and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
CONFLICTS OF INTEREST
The author(s) declare(s) that they have no conflicts of interest.
FUNDING STATEMENT
This study received no funding.
REFERENCES
- Clark D, Barbu H, Lorean A, Mijiritsky E, Levin L. Incidental findings of implant complications on CBCTs: A cross-sectional study. Clin Implant Dent Relat Res. 2019; 21: 13.
- Sarmast ND, Wang HH, Sajadi AS, Angelov N, Dorn SO. Classification and clinical management of retrograde peri-implantitis associated with apical periodontitis: A proposed classification system and case report. J Endod. 2017; 43: 1921-1924.
- Burdurlu MÇ, Dagasan VÇ, Tunç O, Güler N. Retrograde peri- implantitis: Evaluation and treatment protocols of a rare lesion. Quintessence Int. 2021; 52: 112-121.
- Wiedemann TG. A clinical approach to treatment of retrograde peri- implantitis. Compend Contin Educ Dent. 2021; 42: e5-e9.
- Di Murro B, Pranno N, Raco A, Pistilli R, Pompa G, Papi P. Knowledge and attitude towards retrograde peri-implantitis among Italian implantologists: A cross-sectional survey. Int J Environ Res Public Health. 2020; 17: 8356.
- Shah R, Thomas R, Kumar AB, Mehta DS. A radiographic classification for retrograde peri-implantitis. J Contemp Dent Pract. 2016; 17: 313- 321.
- Manfro R, Garcia GF, Bortoluzzi MC, Fabris V, Bacchi A, Elias CN. Apicoectomy and scanning electron microscopy analysis of an implant infected by apical (Retrograde) peri-implantitis: A Case Letter. J Oral Implantol. 2018; 44: 287-291.
- Roy M, Loutan L, Garavaglia G, Hashim D. Removal of osseointegrated dental implants: A systematic review of explantation techniques. Clin Oral Investig. 2020; 24: 47-60.
- Lefever D, Van Assche N, Temmerman A, Teughels W, Quirynen M. Aetiology, microbiology and therapy of periapical lesions around oral implants: A retrospective analysis. J Clin Periodontol. 2013; 40: 296- 302.
- Peñarrocha-Oltra D, Blaya-Tárraga JA, Menéndez-Nieto I, Peñarrocha- Diago M, Peñarrocha-Diago M. Factors associated with early apical peri-implantitis: A retrospective study covering a 20-year period. Int J Oral Implantol (Berl). 2020; 13: 65-73.
- Muñoz-Cámara D, Gilbel-Del Águila O, Pardo-Zamora G, Camacho- Alonso F. Immediate post-extraction implants placed in acute periapical infected sites with immediate prosthetic provisionalization: A 1-year prospective cohort study. Med Oral Patol Oral Cir Bucal. 2020; 25: e720-e727.
- Saleh MHA, Khurshid H, Travan S, Sinjab K, Bushahri A, Wang HL. Incidence of retrograde peri-implantitis in sites with previous apical surgeries: A retrospective study. J Periodontol. 2021; 92: 54-61.
- Ramanauskaite A, Juodzbalys G, Tözüm TF. Apical/Retrograde Periimplantitis/Implant periapical lesion: Etiology, risk factors, and treatment options: A systematic review. Implant Dent. 2016; 25: 684- 697.
- Balshi SF, Wolfinger GJ, Balshi TJ. A retrospective evaluation of a treatment protocol for dental implant periapical lesions: Long-term results of 39 implant apicoectomies. Int J Oral Maxillofac Implants. 2007; 22: 267-272.