Osteoma in the Maxillary Sinus: Report of Two Cases
- 1. Department of Otolaryngology, Keio University, Japan
- 2. Department of Orthopaedic Surgery, Yamada Dental Clinic, Japan
Abstract
Two cases of osteoma arising in the maxillary sinus are reported. Both of the tumors were found incidentally during the evaluation of unrelated diseases.
In a 55-year-old female patient, a bone tumor was found on CT, which was taken to rule out paranasal sinusitis. CT showed a pedunculated tumor arising from the inferomedial angle of the maxillary sinus. It was resected intramurally through the canine fossa en bloc. However, a cyst developed under the nasal floor, which was considered to have arisen from the remnant of the maxillary sinus mucosa. The cyst was endoscopically opened to the nasal floor.
In a second patient, the tumor was found during the preoperative roentgenological evaluation for dental implantation. The tumor, with its base wide-based, arose from the lower part of the lateral maxillary sinus wall in the vicinity of the alveolar recess. As with the first patient, the tumor was resected through the canine fossa. After this surgery, dental implantation by the all-on-4 method was performed successfully. After dental implantation, however, a thickening of bone, indicative of recurrence, was identified near the entrance of the alveolar ridge on CT. Long-term follow-up is required.
Citation
Kunihiro T, Yamada K (2017) Osteoma in the Maxillary Sinus: Report of Two Cases. JSM Head Face Med 2(1): 1005.
Keywords
• Osteoma
• Maxillary sinus
• Bone tumor
INTRODUCTION
Osteomas are benign tumors characterized by proliferation of compact or cancellous bone. The reported incidence has varied from 0.01% to 0.43% in large series of patients who underwent neurosurgical evaluation for nontraumatic reasons [1]. The most common site is the mandible, followed by the sinuses, of which the frontal is involved in 96%, the ethmoid in 2%, and the maxillary in 2% of cases [1,2]. The sphenoid sinus is rarely affected. These tumors are slow-growing, usually asymptomatic, and are generally discovered incidentally during radiographic evaluation of unrelated problems such as minor head trauma [2- 4].
We report two cases of osteoma in the maxillary sinus. The first case was discovered during the evaluation of the patient’s nasal pain and the second case during the preoperative radiographic assessment for dental implantation in the maxilla.
CASE PRESENTATION
Case 1
A 55-year-old female patient presented to the senior author’s outpatient clinic in October, 2009, complaining of nasal pain. The patient had had a fever (37.5-38.0 °C) and watery nasal discharge for three weeks. Her medical history was unremarkable except that she had been diagnosed with ulcerative colitis 10 months before and had been taking mesalazine.
At her presentation to the senior author’s clinic, she had no fever (36.7 °C) and anterior rhinoscopy revealed no abnormalities. However, a computed tomography (CT) performed to rule out paranasal sinusitis showed a pedunculated bony mass arising from the medio-inferior corner of the left maxillary sinus (Figure 1).
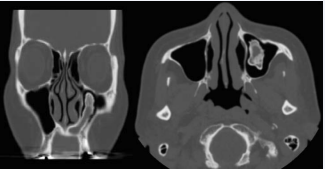
Figure 1 CT images at the time of presentation. A. Coronal view. B. Axial view. The tumor is pedunculated and its base is located at the inferomedial angle of the maxillary sinus. The inside of the tumor seems to be encapsulated by maxillary sinus mucosa.
In November that year, surgery was performed from the oral cavity through the canine fossa. Opening of the anterior wall of the maxillary sinus revealed a white bony balloon-shaped mass with the root at the medial edge in the alveolar fossa. The tumor was extracted en bloc. The space under the floor of the nasal cavity, which was lined with mucosa, was left intact. No material was placed on the raw surface at the end of the operation. Postoperative course was uneventful and the patient returned home one week after surgery. Histopathological findings of the tumor were consistent with osteoma, with no evidence of dysplasia or malignancy (Figure 2).
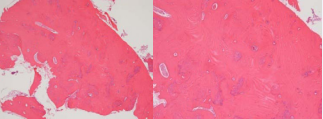
Figure 2 Photograph showing dense bone (H&E). A. Low magnification. B. High magnification. The surface of the tumor is not covered with mucosa.
The patient returned to our clinic 10 days later, when the patient’s left cheek was slightly swollen and the skin was reddish. The lower eyelid on the left side was also edematous. Cellulitis associated with maxillary sinusitis was strongly suggested. Cefcapene pivoxil hydrochloride hydrate at 100 mg × 3 daily was initiated. When the patient returned again one week later, the swelling and the injection of the cheek had disappeared.
However, CT scan performed periodically revealed a growing soft tissue area in the inferomedial portion of the left maxillary sinus extending into the floor of the nasal cavity (Figure 3).
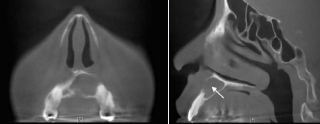
Figure 3 CT images two weeks before the second surgery. A. Coronal view. B. Sagittal view. The anterior wall of the alveolar ridge is destructed partially. The hard palate is also erosive.
That was considered a cyst originating from the mucosa injured during the excision of the osteoma. Although the patient was asymptomatic, the cyst was presumed to continue growing and not only damage the roots of the incisors but protrude to the floor of the nasal cavity. Therefore the cyst was endoscopically opened to the nasal floor in July, 2011 (Figure 4).
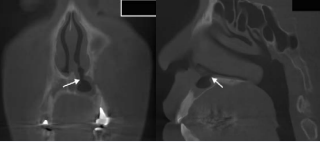
Figure 4 CT images three months after the second surgery. A. Coronal view. B. Sagittal view. The cyst is widely opened to the nasal floor (white arrows)
One year later, the floor of the patient’s nasal cavity had become almost flat due to the proliferation of soft tissue around the original cyst capsule. This was confirmed by CT findings (Figure 5).
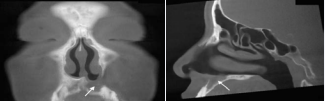
Figure 5 CT images one year after the second surgery. A. Coronal view. B. Sagittal view. The opened window had disappeared. Puncture of the nasal floor confirmed that this was not due to the occlusion of the cyst window but to the proliferation of the surrounding soft tissue.
Case 2
In April, 2011, a 50-year-old, almost totally edentulous, male patient was referred to the senior author’s clinic by a dentist for the evaluation and treatment of an osseous tumor in the right maxillary sinus (Figure 6).

Figure 6 Panoramic photograph taken at the referring dental clinic. A bony mass is seen in the right maxillary sinus (arrows).
The tumor was incidentally found during the radiographical assessment for oral implantation (allon-4) in the maxilla on the tumor (right) side.
Computed tomography (CT) at the time of his presentation to our clinic revealed a cauliflower-like osseous tumor arising from the inferolateral wall of the right maxillary sinus (Figure 7).
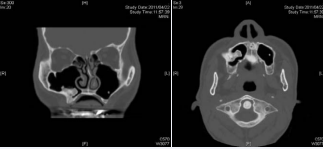
Figure 7 CT images at the time of the patient’s presentation to the senior author’s clinic. A. Coronal view. B. Axial view. A cauliflower-like, osseous tumor is seen. Its base is wide and located at the lower lateral wall of the right maxillary sinus in the vicinity of the alveolar ridge
Although the patient was asymptomatic, it was considered that the tumor would continue to grow and might occupy the whole maxillary sinus cavity and cause maxillary sinusitis. Therefore a survey was performed in October, 2011, using the Caldwell-Luc procedure.
Macroscopically the tumor seemed to be covered with a thin mucosa. The osseous base of the tumor was cut easily with a chisel and a hammer. The remaining tumor tissue, including the surrounding normal bone tissue, was drilled away. In this patient too, no material was placed on the raw surface in the maxillary sinus at the end of the operation. Histological findings were consistent with osteoma (Figure 8).
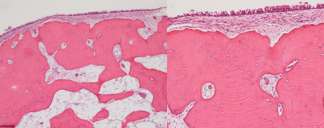
Figure 8 Photograph showing dense bone (H&E). A. Low magnification. B. High magnification. The surface of the tumor is covered with mucosa and submucosal tissue
The patient returned home 5 days after surgery.
When the patient visited the senior author’s clinic two weeks postoperatively, the patient was asymptomatic. However, CT performed on that day revealed pooling of fluid and mucosal swelling in the maxillary sinus (Figure 9).
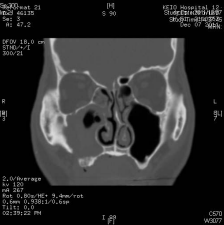
Figure 9 CT images two weeks after surgery. The mucosa in the right maxillary sinus is markedly swollen. It is not possible to identify what occupies the lower part of that soft tissue density area
The lateral wall of the inferior meatus was punctured and irrigated with a saline fluid, which demonstrated that the fluid was a blood clot. Antibiotics were not prescribed. When the patient returned 6 weeks later, swelling of the maxillary sinus mucosa was diminished and fluid was not pooled anymore (Figure 10).

Figure 10 CT images 6 weeks after irrigation of the maxillary sinus
Three months after surgery, the patient underwent dental implantation in the upper jaw by the all-on-4 method at the referring dental clinic. CT taken two weeks later confirmed that the fixtures were placed securely (Figure 11a). However, it also revealed a lesion at the lowermost lateral wall of the right maxillary sinus indicative of recurrence of the tumor (Figure 11b).
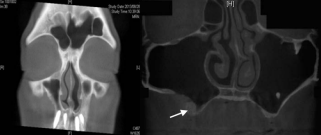
Figure 11 CT image after dental implantation by the all-on-4 method (coronal view). A. A section through the anterior part. B. A section through a more posterior part. The thickened bone (arrow) may be a recurrence of the tumor
DISCUSSION
Osteomas are rare, benign, bony neoplasms that grow slowly and present different clinical presentations. The exact incidence is unknown because most osteomas remain undetected due to an absence of symptoms. In fact, they are generally diagnosed after radiologic evaluations performed for other reasons [4].
In both of our patients, too, the tumor was discovered incidentally. Although the first patient (case 1) presented to the senior author’s clinic complaining of nasal symptoms, CT was performed to rule out upper respiratory infection of the nasal and paranasal areas. Neither of the patients complained of symptoms directly attributable to a tumor in the maxillary sinus. In addition, CT in both patients showed no evidence of inflammation in the maxillary sinus and that the tumors were protruded inwards. The natural osmium of the maxillary sinus was also patent.
However, if the tumors were to continue to grow in size, it was highly probable that the maxillary sinus osmium would be obstructed, resulting in recurrent maxillary sinusitis refractory to medical treatment. Particularly in the second patient (case 2), provided that dental implantation was performed with the tumor left intact, maxillary sinusitis might have caused displacement of the dental implants. Additionally, although the tumor was expected to continue to grow inwards, the tumor might have protruded the anterior wall of the maxillary sinus and caused facial deformity.
During the surgery, the tumor was easily resected through the canine fossa in both of the patients. In the first patient, however, a cyst developed in the floor of the nasal cavity. This was considered to originate from the residual mucosa in this area of the maxillary sinus. The mucosa in that space should have been resected totally during the first operation.
Postoperative cheek swelling on the operated side in the first patient was due presumably to maxillary sinusitis. Although CT was not performed, it was suspected that the maxillary sinus mucosa had swollen, resulting in the occlusion of the natural maxillary osmium. Postoperative bleeding might also have been responsible.
In the second patient, postoperative course was uneventful but CT performed two weeks after surgery demonstrated a pooling of fluid in the maxillary sinus with edematous maxillary sinus mucosa. Irrigation of the maxillary sinus revealed that the fluid was a blood clot, which indicated that a small amount of bleeding or oozing had occurred postoperatively. Maxillary sinusitis did not developed in this patient (case 2). Our experience with these two patients suggests that even for surgery that manipulates the mucosa in or near the maxillary sinus floor only, it is preferable to enlarge the maxillary sinus osmium. An experienced otorhinolaryngologist can enlarge the osmium endoscopically very easily. In our patients, placement of some resorbable material might have reduced postoperative bleeding.
Osteomas are essentially benign and, to the best of our knowledge, their conversion to malignancy is quite rare [2]. However, it is not necessarily easy to macroscopically determine the boundary between the tumor and the normal bone tissue during surgery, particularly if the tumor is wide-based, as in case 2. Therefore, a long-term follow-up for several years is recommended.








































































































































