Use of the Frova
- 1. Department of ENT, Deenanath Mangeshkar Hospital, India
Abstract
Difficult airway is a clinical situation in which a conventionally trained anaesthesiologisthas trouble with either facemask ventilation of the upper airway, difficulty with tracheal intubation, or both. The Frova® intubating introducer (Cook Medical, Bloomington, USA) is anintubating bougie with a high success rate for tracheal intubation. In this article, we describe the successful use of the Frova® intubating introducer for interval ventilation and debulking with laser in a patient with a difficult airway. A 37-year-old male patient presented to the Emergency Department with a severely compromised airway due to Recurrent Respiratory Papillomatosis (RRP). Inability to intubate with an endotracheal tube, the Frova® was introduced and kept in situ. This provided us enough time to debulk the lesion and secure the airway with an Endo-Tracheal tube thus tiding over the difficult situation. This case report is the first of its kind describing the use of an intubating bougie for interval ventilation during laser debulking.
Citation
Bapat S, Bidaye R, Gandhi S (2018) Use of the Frova® Intubating Introducer for Interval Ventilation and Debulking with Laser in a Difficult Airway. JSM Head Face Med 3(1): 1010.
Keywords
- Frova® intubating bougie
- Difficult airway
- Respiratory papillomatosis
ABBREVIATIONS
RRP: Recurrent Respiratory Papillomatosis
INTRODUCTION
According to the American Society of Anaesthesiologists, “difficult airway” is defined as a clinical situation in which a conventionally trained anaesthesiologist has trouble with facemask ventilation of the upper airway, difficulty with tracheal intubation, or both. The guidelines further describe the types of difficult airway as difficult face mask ventilation, difficult supraglottic airway placement, difficult laryngoscopy or tracheal intubation [1]. Several options are available for the management of difficult airway after induction of Anaesthesia. These include blind or fibreoptic intubation - oral and nasal intubation, retrograde intubation, and the use of a light wand (e.g., Trachlight®, Rusch Inc., and Duluth, GA, USA) or a gum-elastic bougie [2-5]. The Frova® intubating introducer (Cook Medical, Bloomington, USA) is a commonly used example of a bougie with a high success rate for tracheal intubation [6-8]. In this article, we describe the successful use of the Frova® intubating introducer for interval ventilation and debulking with laser in a difficult airway.
CASE PRESENTATION
A 37-year-old male patient presented to the Emergency Department with the chief complaint of difficulty in breathing which was progressively worsening over the last 3 days. He was a diagnosed case of Recurrent Respiratory Papillomatosis (RRP) with laryngeal involvement. Having undergone multiple surgeries previously in the same hospital, his case history was well recorded. The last surgery for debulking was performed 9 months back after which the patient was symptom-free for 7 months. Previous surgical notes revealed an uneventful intubation with a 6.0 laser flex tube followed by Microlaryngoscopic Carbon-di-oxide (CO2 ) laser debulking of the lesion. On presentation, the patient was stabilized in the emergency department and a consent for flexible laryngoscopic examination was taken with due preparedness for an emergency. On flexible laryngoscopy, the glottic aperture was severely compromised and the supraglottis was studded with multiple papillomae. Surgical consent was obtained for Microlaryngoscopic CO2 laser debulking after endotracheal intubation. A possible need for tracheostomy was explained to the patient in case of difficulty to secure the airway. Anticipating a difficult intubation, all the necessary measures were taken, and the staff was prepped for an emergency.
After three minutes of pre-oxygenation the peripheral oxygen saturation on pulse oximetry showed an increase from 95% to 99% SpO2 . The anaesthesia was induced with fentanyl 2 microgram/kg i.v. followed by inhalation induction by sevoflurane 7% concentration mixed with Oxygen. Once the patient was anaesthetised deep enough, a quick gentle laryngoscopy was performed, and the larynx was sprayed with 10% lignocaine. Direct laryngoscopy revealed multiple papillomae obstructing the airway with a very small glottic chink in the posterior half. Cricoid manipulation was not of much help. The patient could be adequately ventilated with a face mask; therefore, Succinylcholine was given intravenously at a dose of 2 mg/kg. An attempt was made to pass a 5.5 number Laser flex tube after direct laryngoscopy but could not be manipulated. A 2nd attempt was made with a 5.0 number tube, but the airway could not be secured. Around 90 seconds were lost in this procedure, but the patient’s saturation was maintained at 94%. We had reached a “cannot intubate, cannot ventilate” situation. As per our established protocol, the lead anaesthetist (Author 1) introduced a 14 french gauge Frova® intubating bougie through the narrow aperture under direct laryngoscopic guidance. The introducer was advanced without excessive force and there was a hold up at approximately 27 cms. An attempt was made to rail road a size 5.5 number laser flex tube, but it could not be manipulated. 100% oxygen was delivered through the Frova® as the saturation came up from 92 to 96%. Successful tracheal placement was confirmed by capnography, bilateral chest wall movement and auscultation of both lung fields. A decision was made to debulk the lesion with CO2 laser while maintaining the ventilation with the Frova® (Figure 1).
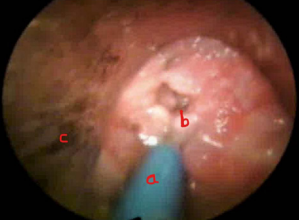
Figure 1 Severely compromised airway with Frova in place. a. Frova intubating catheter b. Glottis covered with multiple papillomae c. Direct Laryngoscope.
Tracheostomy was the next step in case of deterioration of the situation. Anaesthesia was maintained with Sevoflurane, Nitrous oxide and Oxygen and additional doses of Propofol were given intravenously. Microlaryngoscopy setup was assembled and the lesion debulked with an Ultrapulse CO2 laser in scanner mode by the Lead surgeon (Author 3). The Frova® was covered with saline soaked patte to prevent laser strikes and the delivered Oxygen concentration was maintained below 40%. This entire procedure took about 4 minutes in which the patient’s saturation was maintained above the 94% mark. After adequate debulking, a second attempt was made to pass a size 5.5 number cuffed laser flex tube which was successful introduced up to the 22 centimeters at the teeth, the rest of the Laser debulking was performed as routine. There were no complications during or after the surgery.
DISCUSSION
The use of Frova® in difficult airway management has been described by various authors as case reports [9]. International guidelines for [2,3,10] difficult airway management guidelines suggest the use of a tracheal tube introducer early on in cases of unanticipated difficulty. The Eschmann® multiple-use introducer (Reusable guide ‘bougie’, Smiths Medical International, Hythe, Kent, UK) was the first choice for many anaesthetists, faced with unexpected difficult laryngoscopy [11-13]. However, as per the recommendations of the Association of Anaesthesiologists of Great Britain and Ireland on the use of ‘single-use intubation aids’ the clinical practice has evolved towards single-use devices [14]. There were no significant differences between the rates of successful intubation for the Frova® (65%) and the Eschmann® introducers (60%), but it was significantly better than the Portex® single use introducer (8%). The Frova® introducer does come with its own concerns. A separate experiment revealed that owing to their rigidity, the peak force exerted by the Frova® and Portex® introducers was two to three times greater than that exerted by the Eschmann® introducer [6]. It has been reported to cause airway trauma, especially if the ‘distal hold up’ sign is elicited to confirm placement. Also, the proximal end of the Frova® introducer tends to catch the Endo-tracheal tube universal adapter while railroading [15].
The use of Frova® for ventilation provided us adequate time to carry out the debulking with a CO2 laser. The debulking can be carried out with cold instruments but it has a risk of bleeding from the lesion. As the airway was not secured with a cuffed tube, there was an eminent risk of aspiration of blood. The intubating catheter should always be covered with saline soaked cotton patte to reduce the risk of damage and a potential airway fire. After adequate debulking, a Laser flex tube was passed with a relative ease.
We do acknowledge the availability of other devices and techniques to manage a difficult airway situation namely Cricothyrotomy, Mini Tracheotomy. But Respiratory papillomatosis tends to recur at the tracheotomy site due to seeding at the damaged mucosa. The use of infra-glottic jet ventilation was ruled out as there was no passage for egress of expired air and a risk of pneumothorax. The Airway team followed the established guidelines and with their expertise, managed to successfully secure the airway in a difficult situation.
CONCLUSION
Ventilating Bougies are an essential part of the difficult airway protocol and they can buy some time till a definitive airway is established. They can also be used for interval ventilation during CO2 laser debulking of an airway compromising lesion. This case report is unique as it is the first published case in which laser debulking was performed during interval ventilation with an Intubating catheter in situ.








































































































































