Multidisciplinary Approach in Managing Recurrent Adenoid Cystic Carcinoma of Bartholin
- 1. Department of Medical Oncology, Fondazione Policlinico Universitario Campus Bio-Medico, Rome, Italy
Abstract
Bartholin Gland (BG) carcinoma is an uncommon malignancy, comprising less than 5% of all vulvar cancers [1]. Adenoid Cystic Carcinoma (ACC) makes up 10-30% of these cases, following squamous cell carcinoma and adenocarcinoma in prevalence [2]. While ACC is most frequently observed in the minor and major salivary glands, it can also manifest in other secretory glands, such as the tracheobronchial tree, esophagus, breast, and BG. ACC is marked by a slow progression and low tendency for lymph node involvement, but it has a significant potential for hematogenous metastasis, which can occur long after the primary tumor is diagnosed [3]. Because of its rarity, there are no specific recommendations for the management of ACC of BG (ACCBG) and the treatment must be decided in multidisciplinary staff and following the guidelines of the vulvar cancer
Keywords
• Adenoidcystic Carcinoma of Bartholin’s Gland
• Cryoablation
CITATION
Zeppola T, Scafetta R, Speziale E, Vincenzi B, Pantano F, et al. (2024) Multidisciplinary Approach in Managing Recurrent Adenoid Cystic Carcinoma of Bartholin’s Gland: A Case Report. JSM Med Case Rep 6(1): 1014.
CASE REPORT
Initial Diagnosis and Treatment
In August 2003, a 47-year-old female patient underwent a radical hemivulvectomy and systematic left inguinal and pelvic lymphadenectomy for an infiltrative ACCBG, which displayed perineural and muscular invasion. The posterior margin was positive, but no lymph node involvement was observed (0/15 nodes positive). Postoperatively, the patient received three cycles of carboplatin AUC 5 and taxol 175 mg /mq, followed by an additional three cycles of carboplatin alone for an allergic reaction to taxol.
Recurrence and Subsequent Treatments
In July 2017, the patient experienced another recurrence in the left vulvar region with involvement of the elevator any muscle. An MRI on July 9, 2018, revealed a 33 mm solid mass infiltrating surrounding tissues and partially ulcerating, with apparent invasion of the anterior aspect of the left elevator any muscle (Figure 1)..
Figure 1: Giugno 2007.
Systemic Therapy and Disease Management A multidisciplinary team decided to initiate monotherapy with weekly cisplatin 20mg/mq from February 2019, until June 2020, followed by a follow-up period. Cisplatin therapy resumed from October 2020 to March 2021. Despite stable disease on
imaging in March 2021, the patient experienced severe local pain due to nerve and muscle infiltration, poorly managed by opioids. In April 2021, she started treatment with capecitabine (1500 mg/ day), but after two cycles, she discontinued due to poor tolerance and worsening mucosal burning in the anal and vaginal areas.
From July 11 to July 15, 2022, she received RT to the vulvar lesion (total dose of 20 Gy, fractionation of 400 cGy/day). The pelvic RMI of March 2023 showed progression disease so she received carboplatin AUC 2 on days 1, 8, of a 21-day cycle schedule until June 2023. An MRI performed on May 2023 revealed a stable 3 cm lesion in the left vulvar region, infiltrating the vaginal orifice and the distal third of the left lateral vaginal wall, as well as the left ischiocavernosus and bulbospongiosus muscles, reaching the medial cortical profile of the left ischiopubic ramus (Figure 3). Due to the onset of hearing loss, the patient was switched to follow-up care. A biopsy of the left vaginal neoplasm confirmed recurrent ACC.
In November 2023, for worsening pain, she started gemcitabine (800 mg/m² on days 1, 8, and 15 of a 28-day cycle) but only completed one month of treatment before discontinuing due to increased pain and decreased quality of life. Consequently, she started oral cyclophosphamide (50 mg/day). This treatment was stopped on January 2024 due to worsening vaginal discharge and pain.
Recent Developments and Current Status
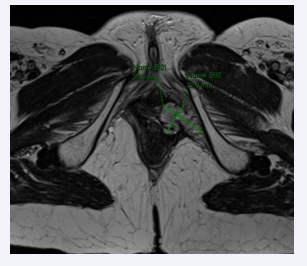
Following a multidisciplinary discussion, considering the significant pain symptoms severely affecting the patient’s quality of life, she was selected for cryoablation of the pelvic lesion (Figure 2-4), which was subsequently performed in January 2024. MRIs performed in February and April 2024 showed stable disease. Currently, the patient is under oncological follow-up, with significant pain relief managed by paracetamol and codeine.
Figure 2: Pelvic MRI with constrast showing ovoidal lesion 33 x 16 mm.
Figure 3: Pelvic MRI with constrast showing 3 cm lesion in the left vulvar region, infiltrating the vaginal orifice and the distal third of the left lateral vaginal wall, as well as the left ischiocavernosus and bulbospongiosus muscles, reaching the medial cortical profile of the left ischiopubic ramus.
Figure 4: Procedure of cryoablation of the pelvic lesion, with the formation at an Iceball measuring 51 x 34 x 35 mm.
CONCLUSION AND DISCUSSION
BG is a small gland located within the labia minora3. Lesions affecting the BG include a variety of benign and malignant tumours, premalignant lesions, mesenchymal lesions, lymphomas, and inflammatory conditions, with cysts and abscesses being the most prevalent. Malignancies of BG include several histological subtypes, such as adenocarcinoma, squamous cell carcinoma, transitional cell carcinoma, ACC, and undifferentiated adenocarcinoma [4]. ACC is a rare tumor that more commonly affects the head and neck region, especially the minor salivary glands, parotid, and sublingual glands, as well as the glandular tissues of the nasal passages and tracheobronchial tree. In the context of Bartholin’s gland, ACC accounts for only 10-15% of BG malignancies, 2-7% of vulvar carcinomas, and less than 1% of genital tumours [4]. ACC is characterized by slow growth, perineural and lymphatic invasion, and a propensity for local recurrence rather than distant metastasis. Symptoms are often nonspecific, including pain, burning sensations, a palpable mass, dyspareunia, or pruritus, with a painful nodule being the most common presentation [5,6]. Distant metastases, when they occur, typically involve the bones and lungs and can arise long after initial diagnosis [7]. In our patient’s, a local recurrence occurred four years post-diagnosis, with further progression after an additional ten years. There are no established guidelines for the surgical or systemic treatment of ACCBG, often following the protocols for vulvar neoplasms. Recommended surgical interventions include simple or radical vulvectomy, with or without lymph node dissection [8]. Studies, such as that by Yang, et al, indicate higher recurrence rates following simple excision compared to radical vulvectomy (68.9% vs. 42.8%). Recurrence rates were similar for patients with both negative (52.1%) and positive (52.9%) surgical margins, although half of the patients with positive margins received adjuvant radiotherapy, suggesting that surgical margin status is crucial in determining recurrence risk [9]. Chemotherapy is recommended for advanced or inoperable ACCBG, though standard regimens are not well established. A large retrospective study highlighted the benefit of chemoradiotherapy over radiotherapy alone for unrespectable tumours, with higher overall survival rates in the chemoradiotherapy group [10]. While there are no standard systemic therapies for advanced or recurrent/metastatic ACC, studies in cervical cancer suggest the potential use of platinum- based treatments. Enrolment in clinical trials and molecular investigations for targeted therapies are recommended. In our patient NGS analysis revealed no gene rearrangements or alterations, despite focal cytoplasmic and membrane positivity for pan-TRK in the neoplastic cells. Despite the limited literature on systemic treatments for ACCBG, these tumours pose significant challenges due to frequent pelvic recurrences and associated pain, severely impacting quality of life. Given the complexity and rarity of this tumor, a multidisciplinary approach is essential for optimal management. This collaborative strategy should involve oncologists, radiologists, surgeons, pathologists, and pain management specialists to tailor a comprehensive and personalized treatment plan. Cryoablation, a minimally invasive procedure that uses extreme cold to destroy abnormal tissue, emerges as a valuable option in this multidisciplinary framework. It is particularly advantageous for patients with recurrent or inoperable tumours, where conventional surgical methods may not be feasible or have been previously exhausted. Cryoablation works by inducing ice formation within the tumor, inducing tissue necrosis and cell death with minimal damage to normal tissues beyond the tumor margin [11]. The technique offers several benefits such the possibility to alleviate pain with the distruption of tumor cells directly responsible for nerve irritation. It is usually associated with shorter recovery periods compared to traditional surgery and it can be used in conjunction with other therapies, such as chemotherapy. This multimodal approach can enhance overall treatment efficacy. In our patient’s case, the decision to use cryoablation followed a multidisciplinary discussion, acknowledging the significant and debilitating pain that compromised her quality of life. Despite multiple systemic treatments, including chemotherapy and radiotherapy, the patient’s pain persisted, underscoring the need for a more targeted intervention. The cryoablation procedure, performed in January 2024, aimed not only to control the local recurrence but also to provide symptomatic relief. The outcomes were promising, with the patient reporting significant pain reduction and stabilization of the disease as confirmed by follow-up imaging in February and April 2024. In summary, a multidisciplinary approach integrating local treatments offers a robust framework for managing ACCBG, particularly for recurrent or inoperable cases. Further research is needed to optimize treatment strategies and improve quality of life for patients with this rare cancer.
REFERENCES
- Evin C, Just PA, Borghese B, Fabiano E, Bennani S, Canny E, et al. Adenoid cystic carcinoma of Bartholin’s gland, a case report with genomic data and literature review. Cancer Radiother. 2023; 27: 328-336. doi: 10.1016/j.canrad.2023.01.001. Epub 2023 Feb 8. PMID:36759241.
- Johnson LR, Nair RP, Sambasivan S, Mony RP, Gangadharan J, Kumar A, et al. Adenoid Cystic Carcinoma of Vulva-11 Years’ Single- Institution Experience. J Obstet Gynaecol India. 2017; 67: 196-201. doi: 10.1007/s13224-016-0935-6. Epub 2016 Sep 19. PMID:28546667; PMCID: PMC5425633.
- Ouldamer L, Chraibi Z, Arbion F, Barillot I, Body G. Bartholin’s gland carcinoma: epidemiology and therapeutic management. Surg Oncol. 2013; 22: 117-122. doi: 10.1016/j.suronc.2013.02.004. Epub 2013 Mar 14. PMID: 23499140.
- Heller DS, Bean S. Lesions of the Bartholin gland: a review. J Low Genit Tract Dis. 2014; 18: 351-357. doi: 10.1097/LGT.0000000000000016. PMID: 24914884.
- Sahincio?lu O, Berker B, Güngör M, Kankaya D, Sertçelik A. Adenoid cystic carcinoma of the Bartholin’s gland: a rare tumor unmarked by persistent vulvar pain in a postmenopausal woman. Arch Gynecol Obstet. 2008; 278: 473-476. doi: 10.1007/s00404-008-0601-z. Epub 2008 Feb 19. PMID: 18283472.
- Woida FM, Ribeiro-Silva A. Adenoid cystic carcinoma of the Bartholin gland: an overview. Arch Pathol Lab Med. 2007; 131: 796-798. doi: 10.5858/2007-131-796-ACCOTB. PMID: 17488169.
- Kumar R, Singhal M, Acharya R, Kudesia S, Chawla N. Adenoid cystic carcinoma of Bartholin’s gland—A rare entity likely to be misdiagnosed. Rev Esp Patolo. 2011; 44: 213-215.
- Oonk MHM, Planchamp F, Baldwin P, Mahner S, Mirza MR, Fischerová D, et al. European Society of Gynecological Oncology Guidelines for the Management of Patients with Vulvar Cancer - Update 2023. Int J Gynecol Cancer. 2023; 33: 1023-1043. doi: 10.1136/ijgc-2023- 004486. PMID: 37369376; PMCID: PMC10359596.
- Yang SY, Lee JW, Kim WS, Jung KL, Lee SJ, Lee JH, et al. Adenoid cystic carcinoma of the Bartholin’s gland: report of two cases and review of the literature. Gynecol Oncol. 2006; 100: 422-425. doi: 10.1016/j. ygyno.2005.08.030. Epub 2005 Sep 27. PMID: 16194566.
- Rao YJ, Chin RI, Hui C, Mutch DG, Powell MA, Schwarz JK, et al. Improved survival with definitive chemoradiation compared to definitive radiation alone in squamous cell carcinoma of the vulva: A review of the National Cancer Database. Gynecol Oncol. 2017; 146: 572-579. doi: 10.1016/j.ygyno.2017.06.022. Epub 2017 Jun 27. PMID: 28662775.
- Solomon LA, Munkarah AR, Vorugu VR, Deppe G, Adam B, Malone JM Jr, et al. Image-guided percutaneous cryotherapy for the management of gynecologic cancer metastases. Gynecol Oncol. 2008; 111: 202-207. doi: 10.1016/j.ygyno.2008.08.003. Epub 2008 Sep 16. PMID:18799209.