Urinary Sediment Interpretation: The Clinical Role of Spheroplasts
- 1. Department of Medicine and Surgery, University of Milan Bicocca, Italy
- 2. Laboratory of Clinical Pathology and Toxicology, Hospital Pio XI of Desio, ASST-Brianza, Italy
Abstract
Urinary Tract Infection (UTI) is among the most common bacterial infections and is considered a public health threat given the increasing rate of antibiotic resistance. Bacteria may change from their normal shape to spheroplasts when exposed to antibiotics at inappropriate dosages. Here, we discuss the case of a patient whose urine sediment examination revealed the development of these abnormal components. Appropriate training of laboratory professionals on the identification of spheroplasts and their clinical significance is important to support the medical specialist in choosing an appropriate antibiotic therapy. Thus, microscopic examination of urinary sediment, offers results beyond the screening level.
KEYWORDS
- Urinary infection; Spheroplasts; Antibiotic resistance; Urinalysis; Misclassification
CITATION
Cosentino P, Tripodi D, Spiti S, Falbo R, Leoni V. (2024) Urinary Sediment Interpretation: The Clinical Role of Spheroplasts. JSM Med Case Rep 6(1): 1015.
ABBREVIATIONS
UTI: Urinary Tract Infection; PBPs: Penicillin Binding Proteins; KPC: Carbapenem-resistant Klebsiella pneumoniae
INTRODUCTION
Urinary Tract Infection (UTI) is one of the most common bacterial infections and is a threat for public health, due to the increasing resistance to antibiotics among the uropathogens, of which Escherichia coli and Klebsiella pneumoniae are the most frequent [1].
The β-lactam antibiotics inhibit peptidoglycan formation by binding to Penicillin Binding Proteins (PBPs) determining rapid lysis and cell death when the antibiotic reaches its optimal concentration. When antibiotics have concentrations significantly below those necessary to stop bacterial multiplication, they can induce changes in bacterial shape, resulting in the formation of abnormal, spherical forms such as those observed in the urine of our patient [2]. These peculiar bacterial morphologies are known as spheroplasts. Here we describe the case of a patient who developed spheroplasts in urine, during antibiotic treatment. Spheroplasts were identified in the course of urinalysis with an automated urine sediment analyzer (Atellica UAS 800, Siemens Healthcare Diagnostics, Tarrytown, NY, USA).
CASE PRESENTATION
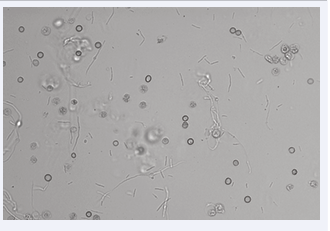
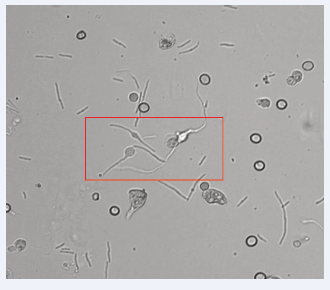
A 91-year-old man presented on June 17, 2024, to the Emergency Department of Pio XI Hospital of Desio, Italy, with fever and hematuria. Laboratory tests revealed a flogistic/septic condition: WBC were 60,5 x 109/L (Reference Interval (RI) 4-11 x 109/L), PCR 246 mg/L (RI< 5 mg/L), PCT 158.80 ng/mL (RI <0,5 ng/mL). A chest x-ray showed a large right basal parenchymal thickening and a bibasilar pleural effusion. The patient was admitted to the Internal Medicine Department and was diagnosed as having pneumonia with mild respiratory failure. He was immediately treated with ceftriaxone disodium and azithromycin dihydrate. Urinalysis was performed during hospitalization and showed the following results: pH = 5.5 (RI 4.5–9.0); relative density = 1.010 (RI 1.005–1.040); hemoglobin (+3) (RI: +/- to + 3); leukocyte esterase = 500 leu/μL (RI < 25 leu/μL); nitrites = negative. Microscopic examination of the urine sediment, with an automated analyzer, revealed the presence of erythrocytes (90/ μL), leukocytes (267/μL), and bacteria (267/μL). These findings suggested the possibility of a UTI. Additionally, we observed some uncommon elements known as spheroplasts. Spheroplasts are bacteria that develop the shape shown in figures 1,2 when exposed to sub-inhibitory levels of ß-lactam antibiotics.
Figure 1: Patient’s urine sediment with particles indicative of UTI. The image was obtained by the automated analyser Atellica UAS 800 (Siemens Healthcare Diagnostics, Tarrytown, NY, USA) in bright field microscopy
Figure 2: Spheroplasts shown in the red box.
This atypical bacterium is indicative of ineffective antibiotic therapy. The urine and blood culture resulted positive to Carbapenem-resistant Klebsiella pneumoniae (KPC).
DISCUSSION AND CONCLUSION
Spheroplasts are unique bacterial forms that have not yet been fully investigated and comprehended. They are Gram negative and can vary in size and length. This unusual form develops when sub-inhibitory antibiotic doses are present. These antibiotics cause partial damage to the peptidoglycan layer, a component of the bacterial cell wall, without causing cell lysis, which leads to the formation of filamentous or spherical forms that are typical of spheroplasts [3,4]. The peptidoglycan layer is synthesized by enzymes known as PBPs which belong to the family of serine transferase proteins and are involved in the formation of a cross-link between two peptidoglycan filaments. The peptidoglycan layer controls the bacterium’s shape, protects the wall from lysant substances, and prevents changes due to intracellular osmotic pressure. Binding to PBPs, β-lactam antibiotics prevent the production of peptidoglycans. When the antibiotic concentration reaches the optimal level, rapid lysis and cell death occur. The structural changes in the bacterial cell wall represent a mechanism that allows the bacteria to survive in the presence of antibiotics. After the antibiotic is removed, they may regain their natural shape and begin to start growing again. This suggests that these elements may promote reinfection, after discontinuation of therapy [5]. These aberrant forms grow well in low osmolarity media with a low pH. Since urine has an acid pH and typically is hypertonic, the urinary system provides favorable conditions for the survival of spheroplasts and related cells.
As already mentioned, in our patient, urine culture revealed the presence of Klebsiella pneumoniae KPC, a strain that produces carbapenemase and consequently is resistant to carbapenem. The observed spheroplast formation could be related to the presence of this strain. The bacteria were resistant to most of the antibiotics tested with the antimicrobial susceptibility test. However, it was susceptible to the ceftazidime/avibactam combination and the clinicians modified the treatment accordingly. Thereafter, a steady improvement in the patient’s overall health and a decline in inflammatory markers (WBC 13,8 x 109/L (RI 4-11 x 10³/mmc), PCR 73,6 mg/L (RI< 5 mg/L), PCT 0,25 ng/mL (RI <0,5 ng/mL) was observed.
These abnormal bacterial forms are not well known because there are so few reports regarding their presence in urine. According to Nikler A, et al. [2], these components could therefore be incorrectly classified as yeasts or erythrocytes. As a result, misclassification could lead to a patient receiving the incorrect diagnosis and treatment.
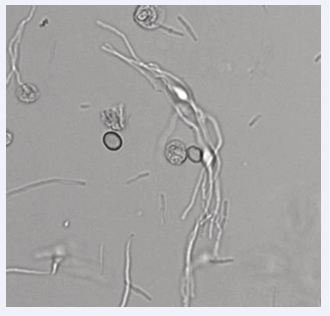
Automated urine sediment analyzers, widely employed in most laboratories today, are not always able to identify and classify all particles. The software usually adopted, incorporates information on the size, morphology, appearance, and intracellular characteristics of the elements due to a neural network. Therefore, elements with similar size and morphology can be confused. This highlights the importance of the laboratory operator’s role despite the use of automated tools, in identifying some more peculiar elements that can often be misclassified (Figures 3,4).
Figure 3: The figure shows that spheroplasts (indicated by red arrow) and red blood cells (indicated by black arrow) can have similar morphology and size.
Figure 4: The Spheroplasts can have similar morphology to hyphae leading to the misclassification as yeasts.
Moreover, laboratory personnel must have sufficient training on the identification of spheroplasts and their clinical importance.
Additionally bacterial forms such as spheroplasts may not grow immediately in the culture medium and the urine culture may initially result negative. A longer urine culture incubation period may be required to prevent false negative results. Therefore, timely communication and collaboration with the microbiology laboratory is necessary when these particles are detected in the patient’s urine.
Finally, the correct identification and classification of these elements can support the medical specialist in selecting an appropriate antibiotic treatment.
In conclusion, urine sediment analysis performed by well-trained operators can play a more significant role and provide results that go beyond the screening level.
Conflicts of Interest
None declared.
REFERENCES
- Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ. Urinary tract infections: Epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol. 2015; 13: 269-284.
- Nikler A, Radiši? Biljak V, ?i?ak H, Mari? N, Bejuk D, Poloni JAT, et al. Escherichia coli spheroplasts in a Croatian patient misclassified by two urine sediment analysers as erythrocytes: Case report. Biochem Med (Zagreb). 2019; 29: 030801.
- Fogazzi GB, Garigali G. Spheroplasts in the urinary sediment. Kidney Int. 2023; 103: 799.
- Falbo R, Fogazzi GB, Sala MR, Garigali G, Sulejmani A, Brambilla P, et al. Spheroplasts, poorly known but clinically relevant particles of urinary sediment. Clin Chim Acta. 2021; 515: 13-15.
- Cross T, Ransegnola B, Shin JH, Weaver A, Fauntleroy K, VanNieuwenhze MS, et al. Spheroplast-mediated carbapenem tolerance in gram-negative pathogens. Antimicrob Agents Chemother. 2019; 63: e00756-19.