Lumbar Disc Erniation L4-L5; L5-S1: An Original Study
- 1. Department Orthopaedic and Trauma Surgery
Abstract
Objectives or purpose or study design: To evaluate the Functional & Neurological outcome of Lumbar Microdiscectomy at L4/5 and L5/S1.
Background: Lumbar disc herniation (LDH) is the most common specific cause for low back pain (LBP). It is a degenerative process causing annular tear with extrusion of the nucleus pulposus through posterior midline or posterolateral aspect of the disc leading to compression of the thecal sac and nerve roots with radicular symptoms. Surgery is reserved for only those who are refractory for a fair trial of nonsurgical management for at least 6 weeks, need of decompression for conus and cauda equina compression, needing immediate attention. There have been various modalities of treatment that have evolved over the years. Micro-lumbar discectomy is one of the latest additions of surgical management modality.
Materials & Method: Retrospectively we reviewed 30 cases from january 2010 to december 2012 in hospital in ALTAMURA ITALY. All the patients had back pain & some neurological deficit with positive MRI findings, underwent lumbar microdiscectomy al L4/5 & L5/S1. Functional improvement was assessed by the ODI Score & categorized into excellent, good, fair & poor, Neurological improvement was assessed by the Nurick Score improvement of pain control by VAS score & overall functional assessment by modified Odom’s score.
Results: Total number of patients was 30. Average age was 36 years (range 22-50). Average follow-up period was 9 months. Pre-operative ODI score was 54.6±12.8 & Post-operative score was improved to 10.2±3.3. In our series we have no chair bound or bedridden patients after surgery. The Pre-operative & Postoperative nurick score was 2.9 & 0.8 respectively. There was no difference in neurological outcomes comparing patients older and younger than 40 years. There was significant improvement in Pre-operative & Post- operative VAS score for leg pain was 6.90 ± 1.9 & 2.0 ± 0.8 respectively & for low back pain was 5.8±1.2 & 2.2±0.8 respectively.
Conclusion: Lumbar Microdiscectomy is a safe & effective method to treat the patients with lumbar disc prolapse with shorter hospital stay & better prognosis with minimum & considerable complications.
Keywords
Lumbar Disc; Original study
Citation
Bernardino S (2022) Lumbar Disc Erniation L4-L5; L5-S1: An Original Study. JSM Neurosurg Spine 9(2): 1109
INTRODUCTION
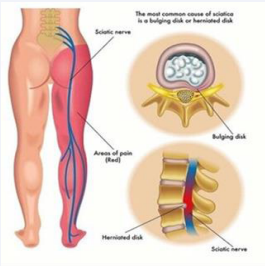
Backache resulting from Lumbago-sciatica is one of the oldest diseases of history. For decades lumbar disc disease is a commonly encountered spine problem for the spine surgeons. Disc herniation causing radicular pain with or without neuro-deficit and those do not respond to conservative management for at least 6 weeks, having their activities of daily living affected are managed surgically (Figure 1).
Figure 1: Pathology of lumbar disc.
Discectomy for symptomatic lumbar disc herniation is performed commonly performed surgical spinal procedure [1]. The first lumbar discectomy was done by a laminectomy and transdural approach was performed by Mixter and Barr in 1934. Semmes first described the hemi-laminectomy approach with retraction of the dura to decompress the neural elements. Discectomy by laminectomy was the common approach for prolapsed disc for a very long time. However, this involved removal of a large amount of normal bone, ligamentum flava, muscle tissue and sometimes facet joints which resulted in iatrogenic instabilities to the spine and failed back syndromes. Hence, conventional laminectomy and discectomy has been replaced by soft tissue techniques.
With the devolopment of better retractor systems, illumination and magnification, discectomies are performed by a more conservative route of interlaminar approaches. Love described his interlaminar fenestration technique as early as 1939. Surgeons have modified Love’s technique to make it minimally invasive [2].
Conventional fenestration technique used paraspinal muscular elevation bilaterally, and larger incisions and retractor systems.
Interlaminar approach was used to enter the epidural space, with aggressive discectomy.
Patient selection and/or preoperative evaluation of the patients should be carefully done to increase patient’s outcome after the microdiscectomy. In young and athletic patients, we prefer microdiscectomy, because strong paravertebral muscles will share the loading with spinal column.
In minimally invasive techniques, paraspinal muscular elevation is done for only 2 to 3 cm using specialised retractor systems.
Caspar in 1977 and Williams in 1978 described microlumbar discectomy technique [3,4]. Due to the postulated advantages of reduced tissue invasiveness, limited blood loss, a shorter duration of surgery, and a faster postoperative recovery, minimally invasive microdiscectomy is very popular now a days. Adequate illumination and magnification of the opetative field are achieved by the use of microscopes, operating loupes and head lamps or endoscopes. Minimally invasive techniques have the overall advantage of less tissue scarring and better visualization of the dura, roots and disc spaces and hence are expected to have better postoperative outcomes [5]. The added advantage of of this procedure is minimum tissue damage & less chance of fibrosis.
Perineural and epidural fibrosis was reported in the subsequent study. Epidural fibrosis/ perineural fibrosis is a nightmare to any managing physician and a major bane for the affected patient.
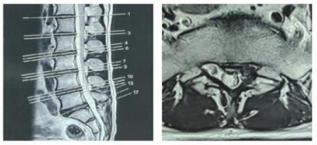
There have been various modalities of treatment for this disease condition that have evolved over the years. The objective of our study is to analyze safety, efficacy, and complications following Micro-lumbar discectomy (Figures 2,3).
Figure 2: Sagittal MRI of L/S Spine
Figure 3: Axial MRI of L/S Spine with pilot film.
MATERIALS & METHOD
Retrospectively we reviewed 30 cases from 2010 to 2012 of Lumbar disc herniation. All patients presented with the various symptoms and signs with the positive magnetic resonance imaging (MRI) and underwent decompression by microlumbar discectomy. Functional improvement was assessed by the ODI Score, Neurological improvement was assessed by the Nurick Score, improvement of pain control by VAS score & overall functional assessment done by modified Odom’s score. IBMSPSS V26 software was used for statistical analysis.
SELECTION OF THE PATIENTS FOR SURGERY
Inclusion criteria
Patients with low back pain who are diagnosed as PLID at L4/5 &/or L5/S1 & not responding to conservative treatment or progressive neurological deficit.
Exclusion criteria
Patients with lumbar disc prolapse other than L4/5 &/or L5/ S1, malignancy, tuberculosis & patients with severe co-morbidity for which he/she is unfit for surgery.
Operative Procedure
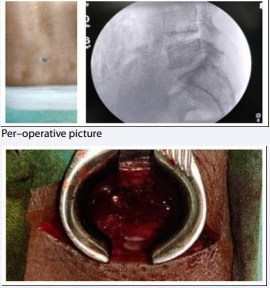
The patient should have prone position. Careful inspection should Functional & Neurological outcome of Lumbar Microdiscectomy at L4/5 and L5/S1 be done to the eyes, ulnar nerves, and genitalia for the males, and breast for the females to ensure that excessive pressure does not exist. Abdominal viscera and vessels should be checked to hang free. The surgical area is propped with an antiseptic solution and covered with sterile clothes. The discectomy level should be identified with C-arm before the operation and incision line is marked.
The length of the incision line changes between 1.5 -2 cm, the lower point of incision should be the upper point of lower spinal process. While performing incision, subcutaneous tissue should not be destroyed to avoid fat tissue necroses. Fascia should be opened just lateral border of spinous process to keep supraspinous ligament intact.
After dissection of the muscle tissue on the spinous process and lamina, it should be cared to the two important points. First of them is to save the capsular ligament and second is to leave intact the interspinous ligament; therefore retractor should not be forced against interspinous ligament. The next step is to save ligamentum flavum. In L5-S1 level, the ligamentum flavum is opened from the medial side to lateral as a flap like C and fixed with a spinal needle to the lateral wall. Under the microscope magnification, epidural fat tissue retracted medially with nerve root. This procedure should be performed gently, because there is a very thin layer to keep the fat tissue. If this layer is opened, the dispersed fat tissue can prevent to see the nerve root. The thin layer should be opened just under the nerve root. Some epidural veins can be seen and coagulated with bipolar. After these procedures, disc annulus can easily be found under the nerve root and discectomy is performed. After the discectomy, ligamentum flavum is placed on the epidural fat tissue. The fascia is sutured and skin is closed with subcutaneous intradermal sutures (Figure 4).
Figure 4: Percutaneous identification of L5/S1 space by guide pin with C-Arm image.
RESULTS
The retrospective analytical study includes 30 patients who fulfilled the inclusion criteria, were operated by microlumbar discectomy for PLID at L4/5 &/or L5/S1. All patients were followed up from 6 months to 1 year (average 9 months) post-operatively (Tables 1-6).
Table 1: Demographic Distribution of Patients (n=30).
| Gender (Male/Female) |
Age (years) |
Hospital Stay (days) |
Surgery Time (min) |
Blood Loss (ml) |
Follow-up (mouths) | L4/5 | L5/S1 |
|---|---|---|---|---|---|---|---|
| 17/13 | 40.3 ± 10.1 | 3.60 ± 1.26 | 32.80 ± 10.47 | 28 ± 12.67 | 15 ± 9 | 17 | 13 |
Table 2: Pre-operative and post-operative comparison of pain.
| After 12 months (n=30), According to VAS score | |||
|---|---|---|---|
| Score (VAS) | Pre Operative (Mean ± SD) | Final Follow-up (Mean ± SD) | p value |
| Back Pain | 6.90 ± 1.9 | 1.8 ± 0.8 | <0.001 |
| Leg Pain | 5.8±1.2 | 2.2±0.8 | <0.001 |
Table 3: Pre-operative and post-operative Nurick Score (n=30).
|
Score |
Pre Operative |
Post Operative |
|
Nurick |
2.9 |
0.8 |
Table 4: Pre-operative and post-operative ODI Score.
|
Score |
Pre Operative |
Post Operative |
|
ODI |
54.6 ± 12.8 |
10.0 2± 3.3 |
Table 5: Distribution of patients according to post-operative.
|
Clinical Outcome (n=30) |
||
|
According to Modified Odom’s Criteria (Odom et al, 1958) |
||
|
Comprehensive |
Frequency (n) Percentage |
Outcome |
|
Excellent |
21 |
70 |
|
Percutaneous identification of L5/S1 space by guide pin |
||
|
Good |
7 |
23 |
|
With C-Arm image |
||
|
Fair |
2 |
7 |
|
Poor |
0 |
0 |
Table 6: Distribution of patients according to post-operative.
|
Complications |
Complications No. Of patients |
|
Wound dehiscence |
0 |
|
Radicular pain |
3 |
|
Granuloma |
0 |
|
Wound Infection |
1 |
|
Seroma |
0 |
|
Dural leakage |
1 |
|
Discitis |
0 |
DISCUSSION
Patients treated by micro lumbar discectomy were followed up for the period of 12 months. Overall clinical outcome categorized as excellent, good, fair, and poor according to modified Odom’s criteria. For statistical analysis good and excellent were grouped as satisfactory and fair and poor as unsatisfactory.
n this study, age range of the patients were 27 – 55 years, mean age was 40.3 ±10.1 years and the male to female ratio was 1.3:1 which are comparable to the study of Fabres A et al, who found mean age 43.1 ± 13.6 [6].
ll 30 (100%) patients had low back pain & radicular pain, motor deficit in 6 (20%) patients, sensory deficit in 5 (16.67%) patients, foot drop in 1(3%) patient, bowel & bladder involvement in 2 (6.6%). This is also comparable to study of Raghu et al. All were improved significantly (P<.001) in postoperative group [7].
Regarding the leg pain control according to VAS was 6.90± 1.90 preoperatively and significantly decreased to 1.6 ± 0.8 at the last follow-up (P< 0.001). This corresponds to the study of Jaiswal et al. In our series the, pre & post-operative Nurick score was 2.9 & 0.8 which was satisfactory for the patients [8].
The mean ODI score was 54.6±12.8 & 10.2±3.3 respectively which is compitable to the study of Jaiswal et al. The differences in the ODI scores were statistically significant between the pre and postoperative follow-ups (p<0.001). ODI scores below 40% were graded as good outcomes (success), whereas higher scores were considered partial or total failures.
Post-operative superficial wound infection was in 2 (6.7%) Wound infection was managed conservatively by antibiotics according to culture and sensitivity report, improvement of nutritional status, removal of stitch, regular dressing & secondary wound closure. The average peri-operative blood loss was 28±12.67 ml. Per-operative dural leakage occurred in 1 patient,
who was managed by dural repair & placement of a drain tube with early removal of drain. The average post-operative hospital stay was 2-4 days. In our study, 21 (70%) patients got satisfactory results and 7 (23%) patients got Good result, in 2 (7%) case had fair outcome according to the Modified Odom’s Criteria. In our series, there was no radio-logical progression after surgery [9- 15].
CONCLUSION
Lumbar Microdiscectomy is a safe & effective method to treat the patients with lumbar disc prolapse with shorter hospital stay & better prognosis with minimum & considerable complications.
REFERENCES
9. Hoppenfeld S, DeBoer P, Buckley R. Surgical exposures in orthopaedics: the anatomic approach. Lippincott Williams & Wilkins 2012 Mar 28.