An Optic Nerve Glioma in a 4-Year-Old Child Operated on in the Northem Region of Burkina Faso
- 1. Department of Neurosurgery, Ouahigouya Regional University Hospital Center, Burkina Faso
Abstract
Introduction: Optic nerve gliomas are rare tumors, accounting for around 5% of intracranial tumors in children. They are potentially aggressive both visually and cerebrally, which justifies a neurosurgical approach to their management. We report a case of optic nerve glioma managed at the Persis pediatric medical and surgical center in Ouahigouya.
Methods: We describe a case of optic nerve glioma managed in May 2023 at Persis medical and surgical center of Ouahigouya.
Observation: The patient was a 04-year-old male who presented with right-sided, painless, progressive exophthalmos that had been present for three months, without hyperthermia or headache. The patient had no known pathological history. Clinical examination revealed painless, non-axial exophthalmos, oculomotor nerve paresis and absence of light perception. Cerebral Computed Tomography (CT) revealed an isodense, intraconical tumor-like expansive process in contact with the nerve, with low enhancement on injection of iodinated contrast. Following a right latero-orbital approach with partial removal of the zygoma, the lesion was removed macroscopically in one piece. Macroscopically, the lesion was pearly-white and non-hemorrhagic. The anatomopathological study suggested a pilocytic astrocytoma of the optic nerve. Post-operative evolution after one year showed a decrease in exophthalmos, no light perception in the right eye and no recurrence.
Conclusion: While most optic nerve gliomas are low-grade, their clinical course is unpredictable and highly variable. Indications for surgery are highly variable, and are unlikely to improve the patient’s visual prognosis if surgery has already begun.
Keywords
• Exophthalmos
• Pilocytic astrocytoma
• Child
• Northem Burkina Faso
Citation
BIOGO WJ, COMBOIGO SL, PARE P (2024) An Optic Nerve Glioma in a 4-Year-Old Child Operated on in the Northem Region of Burkina Faso. JSM Oro Facial Surg 7(1): 1018.
INTRODUCTION
Optic nerve gliomas are the most common tumors of the optic nerve. They represent around 1% of all intracranial tumors, and 3-5% of childhood brain tumors. In 90% of cases, they are found in children [1]. The histological type described is generally a well-differentiated grade I or pilocytic astrocytoma, more rarely a fibrillary or grade II astrocytoma [2]. They represent a real challenge for the practitioner, given the variety of clinical manifestations and diagnostic difficulties in the early stages. Indications must be discussed on a case-by-case basis. Here, we report a case of optic nerve glioma managed at the Persis pediatric medical-surgical center in Ouahigouya.
METHODS
We describe a case of optic nerve glioma operated on in May 2023 at Persis medical and surgical center of Ouahigouya.
OBSERVATION
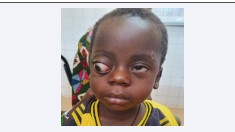
The patient was a 04-year-old male residing in the northern region of Burkina Faso, who consulted us with right-sided, painless, progressive exophthalmos (Figure 1). According to his parents, this symptom had been evolving for three months without hyperthermia or headache. The patient had no known pathological history.
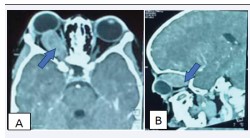
Clinical Examination Noted
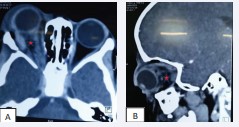
Good general condition, temperature 37°3, blood pressure 130/70mmHg, heart rate 98 beats per minute, pulse 98 beats per minute, respiratory rate 24 cycles per minute and weight 34kg. A painless, non-axial exophthalmos, oculomotor nerve paresis and absence of light perception (Figure 1). Brain Computed Tomography (CT) revealed an isodense, intraconical tumoral expansive process in contact with the optic nerve, with weak enhancement on injection of iodinated contrast medium (Figure 2,3). The preoperative work-up, i.e. rhesus blood grouping, blood count, fasting blood glucose, azotemia, creatininaemia and prothrombin level were all within normal limits.
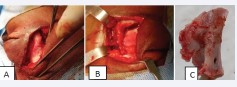
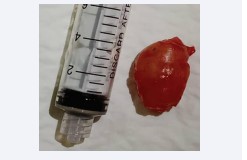
Figure 1: Image showing non-axial right exophthalmos with palpebral malocclusion
After a consultation and pre-anaesthetic visit, surgery was scheduled. Macroscopically, it was a firm, pearly-white tissue mass (Figure 4,5). After achieving satisfactory hemostasis, we redeposited the bone flap and secured it with non-absorbable suture. The skin was closed in two planes using separate stitches. Post-operatively, he received parenteral analgesic (paracetamol 510mg every 06h), antibiotic (ceftriaxone 1700mg every 24h) and corticosteroid (prednisolone 40mg) treatment for 03 days in hospital, followed by oral analgesic (paracetamol 500mg every 8h as required). The postoperative course was straightforward, and the follow-up CT scan performed on the second day after surgery showed macroscopically total excision (Figure 6). Anatomopathological study suggested a grade I WHO pilocytic astrocytoma of the optic nerve. Post-operative evolution after 1 year showed a reduction in exophthalmos, absence of light perception in the right eye, and no recurrence (Figure 7).
Figure 2: Cerebral CT scan in parenchymal window with injection of contrast medium in axial section (A) and sagittal section (B) showing a right intraconical tumor mass indicated by the blue arrow.
Figure 3: Image showing S-shaped skin incision.
Figure 4: Images (A, B, C) showing a right lateral osteotomy.
Figure 5: Image showing monobloc tumor resection.
Figure 6: Parenchymal CT scan of the brain with contrast injection in axial section (A) and sagittal section (B) on D1 post-op, showing an empty tumour bed indicated by the red star.
Figure 7: Image showing a post-operative check-up at 12 months, showing a significant reduction in right exophthalmos.
DISCUSSION
The prevalence of optic nerve gliomas in the general population is 1 per 100,000 inhabitants [3]. Its incidence is 5% of intracranial tumors. Despite this low incidence, they represent the most common optic nerve tumor in children [4], with an average age at diagnosis of four to five years [5]. We have no statistical data available on optic nerve gliomas.
Gliomas of the optic pathways are said to be anterior when they affect one of the two optic nerves, resulting in strabismus, decreased unilateral visual acuity, or exophthalmos in the case of intra-orbital development. In posterior forms, the chiasma is affected. This form is extremely dangerous, as not only is the functional prognosis compromised by the tumor’s extension towards the two optic nerves, but the vital prognosis is also compromised by the tumor’s highly advanced extension upwards towards the third ventricle and the hypothalamus [6].
Exophthalmos and right-sided monocular blindness were the circumstances in which our patient’s optic nerve glioma was discovered. Exophthalmos is a common finding in the literature [7], so much so that it is accepted that “behind an exophthalmos hides a tumor until proven otherwise” [8]. Our patient’s blindness could be explained by the delay in diagnosis of a tumour evolving in a small site. Seventy (70)% of optic nerve gliomas are associated with Neurofibromatosis type 1 (NF1) or Von Recklinghausen disease [9], in fact the diagnosis of NF1 is made in a subject with at least two of the following criteria: At least six café-au-lait spots, at least two neurofibromas of any type, or a plexiform neurofibroma; axillary, inguinal and/or axillary lentigines, an optic tract glioma; at least two Lisch nodules; a characteristic bone lesion (sphenoid dysplasia or thinning of the cortex of the long bones [10]. In our patient, we noted no lesions suggestive of associated NF1, but paediatric follow-up is essential, as certain signs may manifest late in children, as in the case of Lisch nodules, which appear late in children after the age of 06 [11].
Cerebral Computed Tomography (CT) revealed an isodense, intraconical tumor-like expansive process in contact with the optic nerve, with weak enhancement after injection of iodinated contrast medium and no intracranial extension. This lesion is anterior, which explains our patient’s signs. Optic nerve gliomas appear as fairly well-limited lesions, enhancing modestly after contrast injection on CT. Exceptionally, they show calcifications, which differentiates them from intra-orbital meningiomas, which are very rare in children [12]. Magnetic Resonance Imaging (MRI) of the brain, the gold standard in the exploration of intraorbital masses, was not performed in our patient for two reasons; its unavailability in our health region and the patient’s lack of financial means to afford this service in the capital.
The management of optic nerve gliomas requires an individualized approach.Treatment is based on surgery, radiotherapy, chemotherapy and, in some cases, abstention from treatment with simple monitoring. However, some authors [13- 16] have worked to establish clear therapeutic indications. As a matter of priority, oncological treatment should be considered when there is a significant increase in glioma volume on repeated MRI scans with preserved or useful visual acuity. Surgical excision should only be considered in cases of eye-threatening exophthalmos with palpebral malocclusion, raising concerns about trophic, aesthetic and infectious complications, or in cases of extension into the optic canal towards the optic chiasma, with severely impaired visual function or even blindness.
But with moderate exophthalmos and normal visual acuity, or useful in the case of intra-orbital optic nerve glioma, a conservative attitude should be the rule. In our patient, monocular blindness and threatening exophthalmos with palpebral malocclusion were the arguments for the surgical indication. He underwent monobloc tumor resection via a right latero-orbital approach, with partial removal of the zygoma. Because of their topography, optic nerve gliomas sometimes require vascular-neuro-ocular sacrifices of varying importance. For intra-conical tumours, the strict or modified lateral approach is also used, with the primary aim of regressing exophthalmos by means of a lateral orbitotomy [17]. This approach is said to be less aesthetically invasive and less morbid than other approaches [18].
The natural history of optic gliomas is highly variable from one individual to another, based not only on histological criteria but also on the presence or absence of NF 1. Survival in forms strictly localized to the optic nerve is close to 100%. In our patient, the tumour was removed macroscopically in its entirety, and the post-operative course was straightforward, with regression of the exophthalmos and persistence of right-sided monocular blindness. Pathological examination revealed a World Health Organization (WHO) grade I pilocytic astrocytoma.
CONCLUSION
The diagnostic circumstance was exophthalmos and right monocular blindness. Cerebral CT scan with iodinated contrast injection enabled a diagnostic approach and management planning. Complete surgical excision resulted in recurrence-free recovery at one year post-operatively. However, despite surgical excision, we did not observe any recovery of visual acuity.