Application of Low Level Laser Therapy in Dentistry: Laser Biostimulation
- 1. Department of Life, Health and Environmental Sciences, University of L’Aquila, Italy
Abstract
Laser devices are powerful instruments and are fully integrated in a dentist’s life working. They are mostly known for the thermal cutting properties, therapeutic lasers find a wide application in the regenerative and adjuvant medicine. The aim of this short review is to provide the definition of Laser Biostimulation, its last updates and applications in dentistry. Employing the photochemical interactions, Laser Biostimulation is widely used to improve the patient comfort, treatment and life quality. Among clinicians, though, this topic can result confusing and not fully understandable. This is because this kind of therapy is relative new and because the exact mechanism of light-tissue interaction is not clarified yet. Even though more randomized clinical trials are needed to verify the real benefit of Laser Biostimulation, understanding the photochemical interactions is fundamental for a more conscious use of therapeutic lasers in dentistry.
Keywords
• Laser irradiation
• Low-power
• Laser biostimulation
• Laser surgery
Citation
Bernardi S, Zeka K, Continenza MA (2016) Application of Low Level Laser Therapy in Dentistry: Laser Biostimulation. JSM Oro Facial Surg 1(1): 1002.
INTRODUCTION
Biostimulation is one fundamental event of the photochemical interactions between laser light energy and the target tissues. Biostimulation affects the biochemistry of cells. The photochemical process bases its efficiency on the theory that chromophores absorb light energy by biochemical-cellular reactions. These substances can be external (photo sensitizers) or internal. The photochemical process is at the basis of Laser Biostimulation, Photodynamic Therapy and Fluorescence diagnostic [1]. Since their effects are widely reported in clinical case reports and in invitro experiments, these three medical applications are currently considered reliable as valid therapeutic choices in dentistry. The aim of this paper is to review and discuss the principles, the current applications and protocols of biostimulation in dentistry.
LASER BIOSTIMULATION
“Laser Biostimulation” is a specialized field of photodynamic therapy using the low energy light to stimulate the organism metabolism [2]. Lasers with analgesic, anti-inflammatory and biostimulation properties are Helium-Neon laser (He-Ne), Diode laser and Nd-yag lasers [3]. Indeed, photochemical processes act within the wavelength from 623 nm to 1064 nm (Figure 1).
Figure 1: Light wavelength spectra.
This specialized field was firstly applied in dermatology, for skin wounds. Soon after, it was suggested to accelerate the healing of wounds in the mouth. Then, it became largely used in cases of aphthous ulcer, herpes labialis, paresthesia, oral mucositis, and as Bisphosphonate-Related Osteonecrosis of the Jaw (BRONJ) therapy [4-10].
INFLAMMATORY AND REPAIR PROCESSES
In order to understand the mechanism of laser biostimulation, the target of this application needs to be explained: the inflammatory and repair processes.
Inflammation is the reaction of living tissues to a local injury and aims at destroying, diluting or immobilizing the injurious agent by a series of biological processes able to reconstruct the injured tissue as much as possible.
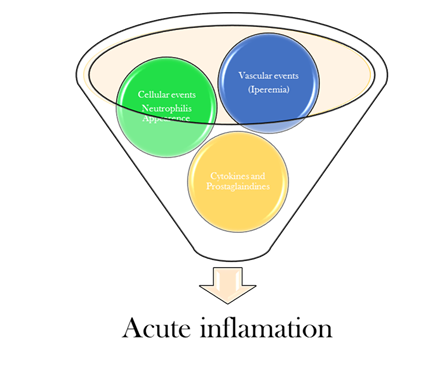
Acute Inflammation can be summarized in the following stages (Figure 2):
Figure 2: Acute inflammation stages.
- ascular events: vasodilatation, permeability of vessels walls
- Cellular changes: Leucocytes migrations
- Chemotactic events: release of factors and proteins in the damage site.
Soon after the damage, the vessels increase their diameter and consequently the blood flows. At the same time, the permeability of the vessels increases in order to allow white cells to reach the damaged site.
Neutrophil granulocytes are the first cells to appear in the injured tissue, they move by chemotaxis. The cytokines active then the white cells [11].
In the healing process, the role of neutrophil granulocytes is the enzymatic destruction of fibrin.
Subsequently, monocytes appear, turning into macrophages. These defense cells, which are the major producers of proteolytic enzymes, are phagocytic par excellence. They are also responsible for the formation and migration of fibroblasts and they stimulate formation of new blood vessels. Fibroblasts, in turn, are stimulated by macrophages in relation to formation and maturation of collagen.
Synthesis of collagen fibers is a continuous event that lasts until the end of the repair process, as tissue remodeling occurs. As for elastic fibers, they allow the tissue to stretch during the healing process without being destructed. Long collagen fibrils are interspersed with elastic fibers in order to limit tissue expansion, preventing tearing of tissue during the repair process [6].
LASER INTERACTIONS
When laser light interacts with cells and tissues in an appropriate dosage, certain cell functions can be stimulated such as mast cell activation and increase of mitochondrial ATP production, so to promote anti-inflammatory effects [12].
This means that low-power laser causes biochemical, bioelectric and bioenergetic changes, leading to increased metabolism, cell proliferation, and reduction of inflammatory mediators, improving the healing process. Molecular absorption of laser light allows an increase in cellular metabolism characterized by stimulation of chromophores in the mitochondrial respiratory chain, changes in cellular ATP levels, release of growth factors, and collagen synthesis.
The anti-inflammatory and anti-edema effects exerted by laser occur through acceleration of microcirculation, resulting in changes in capillary hydrostatic pressure with edema reabsorption and disposal of the accumulation of intermediary metabolites. In addition, biostimulation has been proved to influence positively the proteins and the structures of cell membrane.
Some main biostimulation effects of low-power laser in the process of tissue repair include induction of mitotic activity of epithelial cells and fibroblasts, stimulation of collagen production by those cells, inhibition of secretion of some chemical mediators, changes in capillary density and stimulation of local microcirculation [13,14]. This type of laser stimulates the production of basic fibroblast growth factor (bFGF), which is a multifunctional polypeptide secreted by fibroblasts. It is not only able to induce fibroblast proliferation but also differentiation and it affects the immune cells that secrete cytokines and other regulatory growth factors of fibroblasts.
LOW LEVEL LASER THERAPY APPLICATIONS
Low-level laser therapy (LLLT) has been found to be a valid alternative therapy in aphthous ulcers.
The lesions are typically characterized by recurrent bouts of single or multiple rounded, flat, painful oral ulcers [15]. These ulcers result in oral epithelium wounds, presenting exposed nerve terminations and consequently associated with pain [16]. The etiology is still not clear; however, a series of factors are known to predispose an individual to the occurrence of the lesions. We can distinguish primary predisposal factors, such as genetic factors, alpha-hemolytic streptococcal infections, a decreased immune system integrity, and deficiencies in folic acid, iron, or vitamin B12 , and additional predisposing factors such as stress, trauma, allergies to certain foods, and endocrine imbalances [16–19].
Immune alterations such as cytokine secretion, including tumor necrosis factor-alpha (TNF-a), and leukocyte chemotaxis have been observed; they begin with an unknown antigenic stimulation of the keratinocytes and then result in the activation of T lymphocytes. Current treatment options include topical analgesic and anesthetic agents, corticosteroids, antibiotics, multivitamins, cauterization, and a variety of combined therapies [20]. Most of the treatments are associated with side effects or other disadvantages that make their usage clinically questionable. A challenge to patient management is to significantly stimulate the healing process and minimize patient discomfort, without side effects [10]. Since LLLT affects the inflammatory responses and the vascular microcirculation with a reduction in oedema and pain and cellular biostimulation, this therapy is supposed to be reliable as an alternative treatment for aphotous ulcers.
The most recent protocol used as treatment included the use of a Diode laser (wavelength of 809 nm), with a power set at, 60mW, frequency of 1800Hz, a duration of 80 seconds per treatment, and a dose of 6.3 J/cm2 [21]. Another wound injures type that benefits from LLLT are the herpes labialis lesion. Herpes Simplex Virus (HSV) is a chronic human guest and lasts for life. Several types of exposing factors both physical (UV light, immune suppression) or emotional (stress) are known to cause the virus reactivation and migration through sensory nerves to skin and mucosa, localizing particularly on the basal epithelium of the lips and the perioral area [22]. Immune responses to HSV infection involve macrophages, Langerhans cells, natural killer cells, lymphocyte mediated delayed-type hypersensitivity, and cytotoxicity [7].
The current therapy includes the use of anti-viral drugs to control the recurrent occurrence, but they result temporarily. LLLT has been suggested for accelerated healing, reducing symptoms and influencing the length of the recurrence period [22–24]. The 2012 updated protocol included the use of a 670- nm laser, setting the power at 51 mW/cm2 daily applied for two weeks [24].
Even though mechanism of action is still not clear, an indirect effect of LLLT on cellular and humoral components of the immune system involved in antiviral responses rather than a direct virus-inactivating effect was proposed [25]. Activation and proliferation of lymphocytes and macrophages as well as the synthesis and expression of cytokines following low intensities of red and near infra-red light have been reported by several investigators. The question of whether these effects of LLLT have any influence on HSV infection remains to be determined [7]. Due to these “improve healing” properties, LLLT has been employed also in neuro-damage symptoms such as the paresthesia. The most common reasons of neurosensory damage are dentoalveolar surgery practices such as the removal of mandibular third molars [26–29], orthognatic surgery, cystic lesions removal, implant treatment, and injection of a local anesthetic nerve block [9]. Although most cases of nerve damages are transient and spontaneously resolve with minimal sequelae, some of them can persist.
Possible mechanisms of nerve injury in patients, who sustain sensory deficits after third molar surgery, include compression injury or crush injury. The process of nerve regeneration after compression or less severe crush injuries usually requires from several weeks to 6 months. If there is no sensory recovery during this time, permanent loss of continuity in the nerve trunk should be expected [30]. In Madiba study, LLLT has been shown to both reduce the production of inflammatory mediators of the arachidonic acid family from injured nerves, and to promote regeneration following injury [31].
- Last updated protocol used [32] for this application included following parameters: Diode laser ( 810+/- 20nm)
- Punctual way application
- 32J/cm2 , 9J per site.
Another clinical application of LLLT is the oral mucositis treatment. Oral mucositis usually occurs in patients treated for head and neck cancer. Oral mucositis occurs as side effect of chemo and radiotherapy.
In their randomized clinical trial, Oten Leite et al., [33] tried to establish the effective benefit of LLLT and the gold standard in term of protocol in oral mucositis treatment, checking the level of saliva inflammatory mediators.
Their successful protocol (25% of the laser group Vs the 75% of control group) included:
- Use of In GaAlP diode laser, 660 nm
- 25mW output power
- in a continuous wave
- at a fluence of 6.2 J/cm2
- Energy per point of 0.24 J
- Irradiation time was 10 seconds in each point based on the laser spot size of 0.04 cm2
- Laser energy was applied punctually and perpendicular in contact with the tissue
- Laser irradiation was performed three times a week on alternate days over 7 weeks (35 sessions)
In cancer and osteoporosis treatments, the use of biphosfonates leads to the occurrence of the BRONJ.
This severe clinical condition, which adversely affects the life of the patients, represents one of the oral and maxillofacial surgeon challenges. This is because the ideal approach remains to be debated. LLLT stands out among supportive approaches because of its favorable effects on tissue healing [34].
The last successful protocol reported by Altay et al., [35] provided the following parameters:
- Use of GaAlAs diode laser (808 nm wavelength)
- 0.5 W power
- Continuous wave
- Noncontact mode at 0.5-1 cm distance from the oral mucosa
- Spot size 0.28 cm(2) (R=6 mm)
- Time 3 sec per point (10 sec per cm2 )
- Energy density of 5 J/cm2 (energy per point-1.4 J)
Surgical removal of the lesion and antibiotic therapy were used together with the LLLT. By means of this protocol, all the patients reached the healing of the previously recorded symptoms and the stable mucosal closure.
DISCUSSION AND CONCLUSION
Laser devices are well known to be effective and accurate blades due to their cutting, vaporization and hemostasis properties [36]. In the last 30 years, they have been also used for their therapeutic effects, such as analgesia and the properties to influence cells proliferations (biostimulation) or selective cells destruction (photodynamic therapy) due to the photochemical interaction. In this short review we attempted to summarize the last update protocols available in literature (Table 1).Understanding the mechanisms of light interaction with internal and external chromophores leads to a more conscious use of these therapies and consequently to a high benefit for the patients.
Table 1: Application in dental medicine and related protocols.
| Clinical Application | Last Protocol Suggested |
| Aphthous ulcers | Wavelength: 809 nm Power: 60mW Pulsing frequency:1800Hz Time: 80 s Dose of 6.3 J/cm2 |
| Herpes labialis lesion | Length wave: 670-nm Dose: 51 mW/cm2 Frequency Application: daily applied for two weeks |
| Paresthesia | Diode laser ( 810+/-20nm); Punctual way application; Dose: 32J/cm2, 9J per site. |
| Mucositis | Wavelenght: 660 nm Power: 25mW; output power Mode: in a continuous wave Fluence: 6.2 J/cm2 Time: 10 seconds Frequency application: three times a week on alternate days over 7 weeks |
| Biphosphonate Related Osteo Necrosis of the Jaws | Wavelength: 808 nm Power: 0.5 W Mode: continuous wave Time: 10 sec per cm2 Dose: 5 J/cm2 |
REFERENCES
1. Tunér J, Beck-Kristensen PH. Principles and Practice of Laser Dentistry. Elsevier. 2011; 263-286
4. Bernardi S, Continenza MA. Bone Laser Biostimulation Applied to Implant Dentistry: a case report in Abstracts of the PreCongress Courses from the 12th International Congress on Implant Prosthodontics. June 6– 8, 2013. Padova, Palazzo della Ragione, Italy. Clinical oral implants research. 2013; 1–29.
11. Li J, Chen J, Kirsner R. Pathophysiology of acute wound healing. Clin Dermatol. 2007; 25: 9–18.
17. Rajendran R. Shafer’S Textbook of Oral Pathology. 6th edn. India: Elsevier; 2009; 963.