Recurrent UCNT Revealed by an Orbital Metastasis: Case Report
- 1. Department of Otorhinolaryngology and Maxillofacial surgery, HASSAN II University Hospital, Morocco
INTRODUCTION
In Morocco, as is the case with other Maghreb countries, the incidence of cavum cancer is high [1]. Unlike other head and neck tumors, nasopharyngeal cancer is characterized by a high rate of metastatic dissemination that sometimes reveals the disease [2].
Orbital involvement occurs very rarely by metastatic spread and is often the preserve of recurrent forms [3].
CASE PRESENTATION
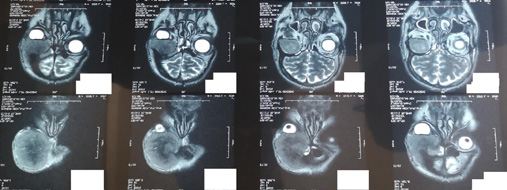
Mr R.M aged 48 years, having benefited 2 years ago from a radio-chemotherapy for a UCNT of the cavum with end of treatment in summer 2018. During the follow-up, Mr R.M presented a fronto-palpebral mass evolving for 3 months, fixed, hard, painless, and responsible for a non-axial exophthalmos, without visual acuity decrease. Mr. R.M. initially underwent a nasofibroscopy without any abnormality and a biopsy showing an undifferentiated carcinomatous proliferation of nasopharyngeal origin. A bone scan showed hyperfixation in the right frontal bone. An orbitofacial MRI was performed and showed a right intraorbital mass measuring 60x64x56 mm, extraconical and extending to the frontal sinus and the homolateral frontal soft tissues. Mr R.M was referred for additional radio-chemotherapy.
DISCUSSION
Orbital invasion in the setting of nasopharyngeal cancer is most often by direct extension through the pterygo-palatine fissure, or the paranasal sinuses. Metastatic dissemination is much rarer. Metastatic recurrence is thought to occur preferentially in the anterior and nasal parts of the orbit. The clinical manifestations associated with these orbital metastases are not very specific: exophthalmos, binocular diplopia, edema or periorbital swelling [4,5].
Magnetic resonance imaging (MRI) has demonstrated its superiority over computed tomography (CT) in demonstrating soft tissue and cranial pair invasion. The value of MRI is even greater when the tumor is large or extends into the brain and parapharyngeal spaces [3]. In case of initial orbital invasion, or a fortiori, metastatic invasion, treatment is always based on radiotherapy with constraints related to the need to protect healthy tissues in the vicinity and to respect radiation doses [6].
CONCLUSION
Orbital metastasis of UCNT of the cavum, revealing or in the context of a recurrence, remains an exceptional entity. Despite its rarity, it must always be in the back of the practitioner’s mind. The difficulty lies in differentiating between metastasis and extension. The therapeutic panel is essentially represented by radio-chemotherapy, and must be adapted on a case by case basis during multidisciplinary consultation meetings [7].
REFERENCES
- Arfaoui A, Soulaymani A, Quyou A, Habib F, Choulli MK. Cavum cancer in Morocco. Epidemiological study on the sample: Al Azhar Oncology Center in Rabat, Antropo. 2007; 14: 75-82.
- Djemaa-Bendjazia A, Sahli B, Bali MS, Djemaa-Bendjazia A, Sahli B, Bali MS. Induction chemotherapy with docetaxel, cisplatin and 5-fluorouracil (TPF) followed by concomitant chemoradiotherapy in locally advanced non-metastatic carcinoma of the cavum, about 25 cases. Cancer/Radiotherapy. 2012; 16: 524-81.
- Senda Turki, Ali Mardassi, Maher Abouda, Amani Hachicha, Wady Ben Jallel. Orbital metastasis revealing an undifferenciated Carcinoma of nasopharyngeal type: a case report. Tunis Med. 2016; 94: 148-51.
- Klauss V, Chana H. Ocular tumors in Africa. Sot Sci Med. 1983; 17: 1743-50.
- Zhang H, Yan JH, Wu ZY, Li YP. Clinical analysis of orbital metastasis from nasopharyngeal carcinoma. Zhonghua Yan Ke Za Zhi. 2006; 42: 318-22.
- Sanguineti G, Geara FB, Garden AS, Tucker SL, Ang KK, Morrison WH, et al. Carcinoma of the nasopharynx treated by radiotherapy alone: determinants of local and regional control. Int J Radiat Oncol Biol Phys. 1997; 37: 985-96.
- Sarra Ouni, Samia Belajouza Kanoun, Abir Ben Neffeti, Wassim Kermani, Mohamed Abdelkefi, Noureddine Bouaouina. Cancer of the cavum from the outset metastatic: clinical and prognostic study (about 51 cases). PAMJ. 2018; 29.