An Exploration of Ultrasound-Guided Therapeutic Injection of the Dorsal Interosseous Ligaments of the Sacroiliac Joint for Mechanical Dysfunction of the Joint
- 1. Sydney School of Medicine, University of Notre Dame, Australia
- 2. Orthopaedic Research Institute, University of NSW, Australia
- 3. Concord Nuclear Imaging & Sydney School of Medicine, University of Notre Dame Sydney, Australia
Abstract
Mechanical dysfunction of the sacroiliac joint is a common cause of lateralising low back pain in young patients in either the peri-partum period or after trauma. Diagnosis is based on evidence-based clinical guidelines and fused scintigraphic tomographic and x-ray computed tomography studies (SPECT/ CT). Accurate diagnosis is important as up to 80% of these patients respond to directed physiotherapy. The remainder can respond to prolotherapy with injection into the dorsal interosseous ligament of the sacroiliac joint. We describe a technique for injection of this structure under ultrasound guidance. Injections into this structure using simple landmarks, allow reproduction of the typical symptoms and pain maps indicating good accuracy in the 36 patients studied.
Keywords
• Ultrasound
• Dorsal interosseous ligament
• Sacroiliac joint
• Sacroiliac joint incompetence
• SPECT/ CT
Citation
Saunders J, Cusi M, Hackett L, Van der Wall H (2016) An Exploration of Ultrasound-Guided Therapeutic Injection of the Dorsal Interosseous Ligaments of the Sacroiliac Joint for Mechanical Dysfunction of the Joint. JSM Pain Manag 1(1): 1003
INTRODUCTION
The lifetime prevalence of low back pain has been reported to be as high as 84% with the prevalence of chronic low back pain being approximately 23% [1]. Between 11-12% of the population will be disabled by chronic low back pain [2]. Non-specific low back pain (NSLBP) is thought to be responsible for 85% of all cases of low back pain with approximately 15% being due to intervertebral disc disease and other causes [2,3]. Thus the vast majority of cases of low back pain will have no identifiable cause. This is supported by the literature which indicates that routine imaging of the lumbar spine utilising plain x-ray, CT or MRI does not add significantly to either functional or pain outcomes in patients with acute or subacute lower back pain [4].
The northern European literature has identified that approximately 15 to 21% of NSLBP may be due to mechanical dysfunction of the sacroiliac joint (SIJ) [5-7]. Prevalence of this diagnosis has been common enough for publication of evidence-based guidelines for the diagnosis and management of such patients [8]. The importance of identification of these cases is that with specific therapy, approximately 80% will regain good functional and pain outcomes [8-11]. A proportion that does not respond to physiotherapy appears to respond to image-guided prolotherapy with hypertonic dextrose [10] or platelet-enriched plasma. We hypothesised that ultrasound-guided injection into the dorsal interosseous ligamentous (DIOL) complex could provide a similar response while avoiding the radiation exposure from either x-ray computed tomography or screening. Reproduction of clinical symptoms by entry of the needle into the dorsal interosseous ligament was utilised as a reference standard for the procedure as part of a prospective outcome-driven trial.
MATERIALS AND METHODS
Clinical group
Patients with an established diagnosis of mechanical dysfunction of the sacroiliac joint (sacroiliac joint incompetence) by careful clinical examination and single photon emission computed tomography/ x-ray computed tomography (SPECT/ CT) of the bone scan comprised the study group [9,10]. Patients were referred for ultrasound-guided therapy by injection into the DIOL of the SIJ with randomly assigned (open label) hypertonic dextrose (30%) or platelet-enriched plasma. The study was approved by the Institutional Ethics Committee of the University of Notre Dame Australia (Sydney Campus). Written informed consent was obtained from all participants in the study (Approval number: 015002S).
Ultrasound technique
The ultrasound injection technique was based on a modification of the work of Hartung et al. [12]. The major difference was that group targeted the synovial portion of the SIJ for intra-articular injection while this group aimed to inject into and around the dorsal interosseous ligament (DIOL), avoiding the synovial portion of the joint. A Sonosite Edge ultrasound machine (Fujifilm Sonosite, Washington, USA) was utilised with a 5-16 MHz linear probe.
The patient is positioned in the prone position with a pillow under the pelvis. The feet are positioned in internal rotation and inversion to provide better access to the sacroiliac joints [12].
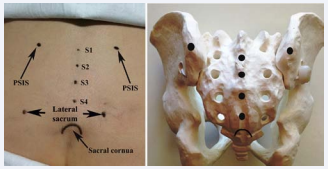
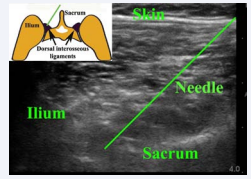
Both posterior superior iliac crests (PSIS) and the sacral cornua are identified by palpation and marked on the skin (Figure 1). The ultrasound transducer is placed on the skin in a transverse orientation to the sacrum (Figure 2). Movement of the probe to the lateral edge of the sacrum now makes the bony structures more conspicuous. Moving the probe in a cephalad direction allows identification of the contour of the ilium. The cleft between the two bony contours is the location of the sacroiliac joint. Drawing a line between the PSIS and the inferior joint will delineate the joint line.
Figure 1 Marking of skin landmarks. The posterior superior iliac spines (PSIS) are palpated and marked. Sacral spinous processes (s1-S4), lateral sacral edges and sacral cornua are marked
Figure 2 Ultrasound landmarks. The ilium and sacrum are identified as echogenic structures with the ilium being cephalad and lateral and the sacrum being central and curved. The cleft between the two is the location of the SIJ. The needle is angulated to reach the DIOL with reproduction of the typical symptoms. The inset graphical illustration shows the relevant anatomy with the needle as a green line.
The component of the joint injected in this procedure is the dorsal interosseous ligament. This is found at the S1/S2 level. The S1 and S2 spinous processes are identified and marked (Figure 1). The transducer is placed in a lateral orientation between these two points. Therapeutic injection is placed at this level. As the angle of the SIJ changes in individuals, the angulation of the needle will change, but generally lies from 45 to 65 degrees.
An initial injection to the skin and along the track of the eventual injection is performed using Lignocaine 1%. This initial track is then followed when performing the therapeutic injection into the DIOL of the SIJ.
RESULTS
Thirty six patients were referred for injection of hypertonic dextrose (20%) or platelet-enriched plasma into the DIOL of the SIJ. This group comprised 30 females and 6 males with a mean age of 32.7 years (Range: 18-44 years).
The symptoms profile were of lateralising buttock pain (n=34), overlapping lateralising buttock and leg pain (n=18), leg pain (n=1), groin pain (n=1), overlapping buttock and groin pain (n=7) and overlapping buttock, leg and groin pain (n=2). Central lower lumbar spine pain was reported in 3 patients with overlapping buttock, leg and groin pain in 2 and overlapping buttock and groin pain in 1.
Patients were positioned prone for the injections. All patients experienced their typical pain distribution when the ultrasound-guided needle entered the DIOL of the symptomatic SIJ. Pain-referral maps were generated for each patient as described elsewhere and were consistent with the nociceptive maps in normal volunteers[14] and patients with mechanical dysfunction of the SIJ [15]. Pain map analysis demonstrated reproduction of buttock pain in 100%, ipsilateral groin pain in 25%, leg pain in 35% and lumbar pain in 15%.
DISCUSSION
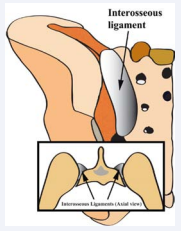
The anatomy of the sacroiliac joint is quite complex and out of reach of clinical palpation, further complicating matters. Attempts to inject the SIJ by palpation have yielded unacceptably poor results that have been reported at 22% [16]. There is clearly a need for image-guidance in this circumstance. In a comparison with fluoroscopy, ultrasound achieved an accuracy of 87% in sacroiliac joint injection, yet had a similar result in achieving pain-relief in patients with mechanical dysfunction of the joint [17]. It indicates the importance of peri-articular injection which clearly anesthetises the DIOL. Furthermore, the ultrasound landmarks for the SIJ contain enough anatomical information to permit image fusion with CT scans as validated in cadavers and patients [18]. The sacroiliac joint is an “L” shaped structure that interlocks with the adjacent iliac bones by virtue of the irregular contours in the joint surfaces which prevent slippage [13]. While the joint is stabilised by a number of anterior ligaments and a joint capsule, the major posterior stabilisers are the long (oblique to the joint) and short (perpendicular to the joint) dorsal sacroiliac ligaments [13]. There is no posterior joint capsule which allows injectate to diffuse freely around the ligamentous and soft-tissue structures at the back of the joint (Figure 3).
Figure 3 Graphical illustration of the anatomy of the dorsal sacroiliac ligaments with the deeper interosseous component that is structurally important.
The two bony landmarks used in the initial joint localisation are the lateral edge of the sacrum and the more cephalad ilium. The SIJ is located in the cleft between these two structures. As the S1 and S2 spinous processes are marked on the skin, it allows the level for the joint injection to be identified in the cleft with the only other variable being the angulation of the joint which generally varies from 45 to 65 degrees, depending on the individual. Reproduction of symptoms by changing the needle angulation will determine this variable.
The modification of the technique of Hartung et al. [12], shows good utility in the therapy of sacroiliac joint incompetence. This is an important issue, as the majority of the population suffering from the disease is either females of childbearing age or young males experiencing trauma to the pelvis or lower back. It avoids the necessity of therapeutic intervention under the control of either CT imaging or fluoroscopic screening, so avoiding an additional radiation burden to the pelvis and gonadal tissues.
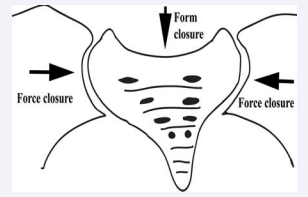
An important distinction between the utility of the technique of Hartung et al. [12], is that the therapeutic injection is into the ligamentous tissues which lie posterior to the synovial portion of the sacroiliac joint and not into the joint itself. The reasoning for the injection of either hypertonic dextrose or platelet enriched plasma (PRP) into the dorsal interosseous ligaments of the sacroiliac joint is based on the integrated model of function of Lee and Vleeming [19]. Their integrated model of the biomechanics of the sacroiliac joint postulates “Form closure” of the sacrum by the two iliac bones and related ligaments, and “Force closure” of the resultant pelvic ring by the abdominal and pelvic floor musculature (Figure 4).
Figure 4 The integrated biomechanical model of sacroiliac joint function with form and force closure. Form closure is the fit of the sacrum between the two iliac bones with the normal circumstance, where the sacrum buries itself into the pelvic ring in a stable configuration. The pelvic ring is also compressed shut by the abdominal musculature (Force closure).
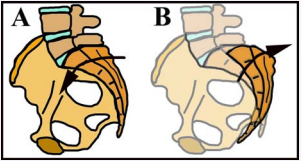
Figure 5 Nutation (A) and counter-nutation (B) of the sacrum. A. Under normal circumstances the sacrum nutates or buries itself into the pelvic ring in a stable configuration. B. When the dorsal sacroiliac ligament is injured, the support for the sacrum is compromised and allows it to rotate backwards (counter-nutation) leading to further pain and loss of the sequence of abdominal muscle contraction with resultant failure of Form closure of the pelvic ring. This worsens the situation and allows unsupported counter-nutation. The purpose of physiotherapy is to re-sequence the abdominal muscle and re-establish Force closure which prevents counter-nutation.
Injury to the dorsal interosseous ligament of the sacroiliac joint results in counter-nutation (Figure 5) of the sacrum (posterior rotation) rather than the normal nutation (Figure 5) which essentially buries the sacrum into the pelvic ring in a stable configuration. The resultant persistent traction on the ligaments leads to pain, which alters the synchronous pattern of contraction of the abdominal musculature in a disadvantageous pattern that leads to a failure of force closure of the pelvic ring. The loss of the compressive force on the pelvic ring enhances the counter-nutation of the sacrum, worsening the condition in an additive manner. The support for this postulated mechanism is that intervention with directed physiotherapy, which re-synchronises the abdominal muscle contractions leads to a significant improvement in pain relief and function in approximately 80% of patients. There is also evidence that prolotherapy with hypertonic dextrose being injected into the dorsal interosseous sacroiliac joint ligaments leads to a significant improvement in function and pain relief [9]. The pathophysiology is commensurate with reduction or abolition of counter-nutation of the sacrum by the resultant improvement in the integrity of the dorsal interosseous ligaments. Outcome of therapeutic intervention based on the force/form closure model of the sacroiliac joint dysfunction has been supported by numerous interventional trials, such that a body of evidence-based clinical guidelines for the diagnosis of the condition have been established and validated [8]. A significant body of evidence also supports the concept that the dorsal interosseous ligaments of the sacroiliac joint are an important pain generator, and may in fact be more important than the sacroiliac joint itself. This was elegantly demonstrated by Murakami et al. [20], in a study of 50 patients with clinical evidence of sacroiliac joint pain. The 25 patients who had local anaesthetic injections into the posterior peri-articular tissues of the involved joint had complete responses with abolition of the pain. Patients injected into the sacroiliac joint itself had a much poorer response, with 9 of 25 patients obtaining adequate pain relief. Importantly, the 16 patients who did not respond to intra-articular injection were subsequently rendered pain-free by peri-articular injection of local anaesthetic. It is compelling evidence for the importance of the dorsal ligamentous structures as a significant pain generator and also supports the functional model of Lee and Vleeming [19].
This simple ultrasound-guided technique provides an additional therapeutic option for a condition that may in fact be more prevalent than intervertebral disc disease as a cause of lower back pain. Non-specific lower back pain is a blanket term for a number of unknown diseases that have evaded a specific diagnosis, thereby excluding the application of specific therapies. It is in fact a short-hand for both diagnostic and therapeutic nihilism. On the other hand, the Northern European literature is replete with studies of a specific diagnosis of mechanical dysfunction of the SIJ for up to 20% of this vast group of patients labelled as NSLBP [5-7]. Treatment of these patients can provide pain relief and functional recovery in over 80% of cases [9]. The utility of ultrasound-guided injection of either hypertonic dextrose or platelet-enriched plasma has the potential to improve the condition in up to a further 15 to 20% of cases, which remains to be proven. Promising evidence from this study is the reproduction of typical symptoms and pain mapping by entry of the needle into the DIOL complex posterior to the SIJ. The ultimate utility of the technique remains to be assessed by the longitudinal study that is currently under way.
CONCLUSION
We have described a simple ultrasound-guided technique for therapeutic injection into the dorsal interosseous ligaments of the sacroiliac joint. The technique can reproduce the typical pain and pain-mapping commensurate with mechanical dysfunction of the joint and has the potential to provided permanent pain relief in the 20% of patients who do not respond to specific physiotherapy.