Utility of a Standardized, Multidisciplinary Rehabilitation Program for Chronic Low Back Pain
- 1. Department of Surgery, University of Minnesota, USA
- 2. Department of Anesthesia and Intensive Care Medicine, University of Basel, Switzerland
- 3. School of Public Health, University of Minnesota, USA
- 4. Department of Health Informatics, University of Minnesota, USA
Abstract
The relative effectiveness of a multidisciplinary outpatient rehabilitation program, designed for patients with chronic lumbar disorders, was assessed. Patient outcome data over two years were collected and associative changes in outcome measurements were analyzed. For 6,340 patients enrolled in this prototype program, satisfaction ratings were 90% at both follow-up evaluations at one and two months. In general, female patients profited more from the intervention as compared to men. Of the patients with return to work data, 90.2% resumed work by four months. After two years, patient usage of prescription and non-prescription medications declined by 47.1% and 33.9%, respectively. Eighty percent of the patients included in the program with the main aim to avoid surgery were successfully treated by conservative measures alone. In conclusion, following the initiation of a multidisciplinary outpatient program, chronic low back pain patients showed improvements in function, reduced pain, and reduced healthcare utilization.
Keywords
• Chronic low back pain
• Rehabilitation
• Outpatient program
• Intervention
Citation
Bandschapp O, Hegge TA, Bhargava EA, Ruppen W, Iaizzo PA (2016) Utility of a Standardized, Multidisciplinary Rehabilitation Program for Chronic Low Back Pain. JSM Pain Manag 1(1): 1001
ABBREVIATIONS
DLIDWM: Displacement of Lumbar Intervertebral Disc without Myelopathy; FAS: Functional Activity Scale; LDDD: Lumbar Degenerative Disc Disease; NRS: Numeric Rating Scale; VAS: Visual Analog Scale
INTRODUCTION
Low back pain is currently the most common musculoskeletal disorder worldwide, with lifetime prevalence estimates ranging from 58-84% [1,2]. Approximately 10 million Americans are disabled by chronic low back pain, and estimates range from 83- 250 million workdays lost annually to this disorder in the United States alone [3]. Almost half of all chronic pain patients (42%) indicate back or low back pain, followed by knee pain (16%) or headaches (15%) [4]. Most low back pain patients return to work within one week and 90% of patients return within two months. However, the remaining individuals require significantly extended leaves which become a major socio-economic burden; e.g., after six months of not working, less than 50% of patients will ever return to work, and after two years the likelihood of returning to work becomes even less[5,6]. Furthermore, in this population recurrence rates for debilitating low back pain are substantial [7,8]. However in more current reports, the recurrence rate is not as high as previously described [9]. Because of such issues, it is considered that the ability to decrease the time between injury and treatment, as well as to improve access to effective education relative to prevention and treatment, would have significant benefits on overall recovery and recurrence rates and/or financial outcomes [10].
Current treatment modalities for low back pain are broad ranging, yet two major categories are easily defined: surgical and non-surgical. The inherent risk of the surgical approach has led to increased interest in minimally invasive and non-surgical procedures [11,12]. However, non-surgical interventions are not without risk either. Indeed, although analgesic medications are widely used in the control of low back pain, their chronic use can be associated with potentially dangerous side-effects. Furthermore, acceptance for chronic analgesia use may decrease with time. In a systematic review, 56% of patients on open level opioid therapy did not take any more opioids after 7 to 24 months [13]; the reasons for this are unclear. In about 90% of patients suffering from low back pain, no clear etiological diagnosis can support the presentation of pain [14]. Moreover, pharmacological and somatic treatments quite often fail to provide prolonged pain relief [15], which may result in misinterpretation and difficulties with reference to medical judgment in the case of chronic pain patients.
Because of the complexity and heterogeneity of the population suffering from low back pain and the lack of clear “best” treatment, focus has shifted to tailored multidisciplinary rehabilitation programs for treating low back pain [16,17]. Guzman and coauthors have systematically reviewed randomized controlled trials using such programs and suggested that intensive multidisciplinary biopsychosocial rehabilitation programs provide functional restoration, reduce pain, and/or improve function in patients with chronic low back pain [18]. In contrast, less intensive interventions did not result in consistent improvements in clinically relevant outcomes.
The aim of the current study was to assess the effect of one such multidisciplinary outpatient rehabilitation program on functional outcomes, pain, patient satisfaction, and healthcare utilization for patients with chronic lumbar disorders. Specifically, we obtained data from the prototype LIFEBACK® Spine Rehabilitation Program, which incorporated exercise/ flexibility training, core stabilization, lifestyle modification, axial spinal unloading therapy, and healthcare coaching at planned intervals, for a 2-year period.
MATERIALS AND METHODS
This research project was approved by the University of Minnesota’s Institutional Review Board Human Subjects Committee; it was determined that the study was exempt from review under federal guidelines 45 CFR Part 46.101(b) category #4, as patient identifiers were not used. The (unrestricted) data used in this project were taken from the most current database of patients participating in the program at the time of analyses, totaling over 6,340 patient records obtained since 1994. Data were analyzed using cross-correlation and ANOVA analyses of demographic and outcomes assessment data.
Of the 6,340 patient entries, 786 were found to have complete data sets including every factor examined in these analyses, i.e., through follow-up evaluations at two years. The data sets were analyzed in entirety based on the information available for each factor or category analyzed (total analysis, n=varied), and then narrowed into the complete data sets for analyses on a fixed number of records (subgroup analysis, n=786). In addition, after statistical significances were determined, the data sets were further subdivided by individual diagnoses to better examine the mean changes and standard deviations in relative outcomes for each subset. Other categories of interest (other than diagnoses) were also studied in a similar manner.
Program clinic staff contacted patients by telephone to assess their progress at predetermined intervals using a standardized format. Specifically, patients were evaluated using outcomes tracking tools to document progress. In addition to participating in telephone surveys, patients returned to the program clinic at four-week intervals for follow-up evaluations until their therapeutic goals were attained. Outcome measures included: 1) modified Oswestry scores; 2) patient satisfaction ratings; 3) relative surgical avoidance; 4) times for return to work; and 5) relative medication usage. For Oswestry and Numeric Rating Scale (NRS) scores, data were collected at initial visits in addition to follow-up visits at one year and two years. Due to lack of information at one and two years, Functional Activity Scale (FAS) scores and return to work data were analyzed based on the longest follow-up times available at three and four months. Patient satisfaction scores were measured at one and two months, the times closest to onsite program involvement
The rehabilitation program
The rehabilitation program, which was previously employed, was an intensive multidisciplinary biopsychosocial rehabilitation program for patients with chronic (>12 weeks) low back pain (this was previously known as the LIFEBACK® Spine Rehabilitation Program). It focused on core strengthening, stabilization, axial spinal unloading therapy using the LTX 3000® (a gravity-dependent axial spinal unloading device to reduce weight bearing on the lumbar spine), flexibility training, lifestyle modification, and training in a cognitive behavioral environment. After patients completed the program, their progress was monitored and patients received coaching for two years (in clinic and/or via the phone or internet). Approximately 2,500 data points per patient were gathered over this 2-year period using standardized measurement methodology.
Statistical analyses
In examining the effectiveness of this prototype program as a standard treatment option for individuals with low back pain, we identified subpopulations that may have gained the greatest benefits. Thus, the data set of 6,340 patient records was subcategorized to search for patterns and relationships amongst various categories. The analyses examined correlations within varying diagnoses and histories from this sample of patient records.
For each outcome variable of interest, correlation analyses were performed with a student’s t-test, ANOVA, or linear regression, utilizing Microsoft Excel to determine the relative significance for each variable before and after correction for gender. A P-value <0.05 was considered significant. These analyses were first performed on the entire data set with varying n values (Total Analysis), and then again for the subgroups, including only those records with information on all the variables examined (n=786) at the follow-up evaluation at one and two years (i.e., Subgroup Analysis). A factor was considered significant if either follow-up evaluation demonstrated its impact, or a single specific follow-up was named if only one was indicated. Once significances with the ANOVA test were identified, Bonferroni post hoc tests and logistical regression analyses were performed to determine correlations between significant variables and the aforementioned outcome measures. Factors determined to be significant when corrected for gender were put into a collective linear regression model in UNIX SAS to determine independent significances.
The following variables were included in the Total and Subgroup Analyses, primarily based on their standard use as factors in evaluations of low back pain programs: 1) binary age of patient (40); 2) gender of patient; 3) relative low back pain duration (in months; binary for both >1 mo and >3 mo); 4) prior low back surgeries; 5) worker’s compensation status; 6) education level; 7) perceived need to lose weight; 8) relative daily alcohol consumption amount; 9) daily smoking habits; 10) expectation of complete and/or moderate pain relief; 11) history of family low back problems; and 12) three most common diagnoses (lumbar degenerative disc disease, unspecific low back pain, and displacement of lumbar intervertebral disc without myelopathy or DLIDWM).
RESULTS
Total analysis
The total data set included 6,340 patient records comprised of 45.5% females and 54.5% males, with an average age of 42.7 years (range 8-86 years). The three most common mentioned causes for pain were lumbar degenerative discs, unspecific back pain, and DLIDWM. The average time from initial injury to pursuit of treatment was 44.6 months, with a range of 0.04-712.8 months.
Subgroup analysis
In the Subgroup Analysis, patients with complete data sets (786 records) were evaluated, of which 43.5% were females and 56.5% were males with an average age of 42.5 years (range 14- 81 years).
Patient satisfaction and surgical avoidance
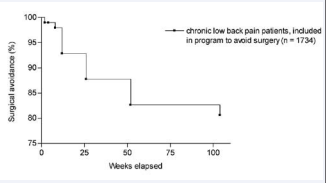
For the total data set of 6,340 patient records, patient satisfaction ratings at one year were 89.1% and 90.9% at two years. Of the 1,734 patients referred to the program to avoid surgery, over 80% were successful at each individual follow-up evaluation (Figure 1)
Figure 1 Resultant degrees of surgical avoidance in patients (n=1,734) that were referred to the program for this purpose. The relative percentage is indicated for each of the monitored follow-up dates.
Return to work and medication usage
Based on 5,972 responses, 11.6 days (range 0-999 days) of normal activity such as work or school were missed, and 90.2% of patients resumed their work by 4 months. In reviewing the population that stopped working due to injury at the beginning of the program, 58.4% returned to work by 4 months (Table 1).
|
Table 1: Return to work data. |
||||||||
|
All Patients (n= various) |
Return to work of patients initially not working due to back pain (n=186) (Number, percentage) |
|||||||
|
Category |
1 month |
2 months |
3 months |
4 months |
1 month |
2 months |
3 months |
4 months |
|
Returned to work full time |
71% |
68% |
71% |
75% |
22 (12%) |
37 (20%) |
61 (33%) |
76 (41%) |
|
Returned to work part time |
18% |
17% |
15% |
16% |
17 (9%) |
22 (12%) |
24 (13%) |
32 (17%) |
|
Not working (back problems) |
5% |
4% |
1% |
0% |
102 (55%) |
76 (41%) |
34 (18%) |
7 (4%) |
|
Not working (no back problems) |
1% |
1% |
0% |
0% |
15 (8%) |
9 (5%) |
4 (2%) |
0 (0%) |
|
Changed position |
3% |
8% |
8% |
8% |
22 (12%) |
34 (18%) |
54 (29%) |
69 (37%) |
|
Retired, homemaker or student |
2% |
2% |
5% |
1% |
8 (4%) |
8 (4%) |
9 (5%) |
2 (1%) |
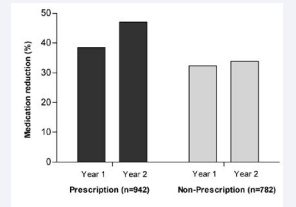
At the follow-up visit at one year, 38.5% of the individuals on initial medication reported reduced prescription medication usage and 32.3% reduced use of non-prescription medications. By two years, 47.1% of the patients reported reduced prescription medication usage, while 33.9% reduced non-prescription medication usage (Figure 2).
Figure 2 Estimated overall medication reduction (both prescription and non-prescription) observed for various subpopulations. At year one, 38.5% of patients reduced prescription medication usage and 32.3% reduced use of non-prescription medications, whereas at year two, 47.1% reduced usage of prescription medication and 33.9% reduced non-prescription use
OSWESTRY OUTCOMES
Complete data sets
Detailed analyses of available Oswestry scores (n=1,618/ various) revealed ten factors that correlated with documented changes. Negative correlations, indicating more negative Oswestry changes and thus improvement of low back pain with presence of the factor, were found for: unspecific low back pain (at year 2 follow-up), DLIDWM (at year 1 follow-up), perceived need for weight loss, and being female (Student t-Test; Table 2).
Table 2: Mean Oswestry score reduction at year 1 and 2 (total data set, n=1,618).
| Factor | Year 1 | Year 2 | ||||
| with factor | without factor | P Value | with factor | without factor | P Value | |
| Workers' compensation | -9.75 | -11.42 | 0.06 | -10.69 | -11.98 | 0.19 |
| LDDD | -9.61 | -11.57 | 0.02 | -10.39 | -12.17 | > 0.05 |
| Unspecific low back pain | -12.73 | -10.69 | > 0.05 | -14.66 | -11.09 | < 0.01 |
| DLIDWM | -13.56 | -10.56 | < 0.01 | -13.04 | -11.42 | 0.16 |
| Surgery | -9.96 | -11.34 | 0.13 | -10.42 | -12.05 | 0.1 |
| Family low back problems | -10.7 | -11.51 | 0.31 | -11.28 | -11.26 | 0.25 |
| Current family problems | -11.54 | -10.85 | 0.44 | -11.22 | -11.82 | 0.53 |
| Feel need to lose weight | -11.97 | -8.97 | <0.01 | -12.68 | -9.5 | <0.01 |
| Drink alcoholic beverages | -10.51 | -11.75 | 0.11 | -11.48 | -11.95 | 0.57 |
| Smoking | -11.33 | -10.92 | 0.64 | -12.24 | -12.48 | 0.42 |
| History of emotional or mental health counseling | -12.51 | -10.56 | 0.03 | -13 | -11.26 | 0.08 |
| Time delay to evaluation > 1 month | -10.99 | -12.23 | 0.62 | -11.58 | -15.33 | 0.16 |
| Time delay to evaluation > 3 months | -10.57 | -13.61 | <0.01 | -11.21 | -14.33 | 0.01 |
| Age > 39 | -10.58 | -11.89 | 0.11 | -11.17 | -12.66 | 0.09 |
| Female Gender | -11.97 | -10.2 | 0.02 | -12.68 | -10.8 | 0.02 |
Average mean Oswestry scores and dependence of various factors at year 1 and 2; P-values for the respective statistical analysis (Student’s t-Test) are shown.
Abbreviations: LDDD: Lumbar Degenerative Disc Disease; DLIDWM: Displacement of Lumbar Intervertebral Disc without Myelopathy.
Additionally, having higher expectations of complete and moderate pain relief, liking one’s job more, and liking one’s supervisor more were also associated with improvement of low back pain over time (ANOVA, Bonferroni-corrected and linear regression without gender correction). In contrast, both lumbar degenerative disc disease (at year 1 follow-up) and a binary time of onset to initial evaluation in the program >3 months were associated with less improvement of low back pain (Student t-Test; Table 2).
Because gender had a significant influence on results, each analysis was corrected for gender as a potential means to determine overall correlations. When corrected for gender, the resultant ANOVA analyses indicated that eight male and six female factors correlated specifically with changes in Oswestry outcomes. For males, perceived need for weight loss, higher education levels, higher expectations of moderate pain relief, liking one’s job more, and liking one’s coworkers and supervisors were correlated with lower Oswestry scores, thus associated with decreased back pain at one of the follow-up evaluations. However, having a diagnosis of unspecific low back pain and an age >39 years negatively impacted pain profiles. For females, a higher expectation of complete pain relief and liking one’s job more were both significantly associated with reduced pain. In contrast, having a diagnosis of lumbar degenerative disc disease or DLIDWM, a binary age >39 years, and an onset time to evaluation >3 months were correlated with less improvement of low back pain (ANOVA, Bonferroni-corrected).
Subgroup analysis
The subgroup analysis with complete data sets (n=786) provided eight factors that correlated well with changes in Oswestry scores. The factors being female (at year 2 follow-up), having a history of emotional or mental health counseling, and a perceived need for weight loss (Student t-Test; Table 3), as well as having a higher expectation of complete and moderate pain relief (ANOVA, Bonferroni-corrected) were all associated with improvement of low back pain. In contrast, the factors time delay of >1 month and >3 months between injury onset and initial evaluation in the program, as well as age >39 years (at year 2 follow-up) were associated with less improvement of low back pain compared to those not having these factors (Student t-Test; Table 3).
|
Table 3: Mean Oswestry score reduction at year 1 and 2 (subgroup data set, n=786). |
||||||
|
Factor |
Year 1 |
Year 2 |
||||
|
|
with factor |
without factor |
P Value |
with factor |
without factor |
P Value |
|
Workers' compensation |
-10.37 |
-12.77 |
0.064 |
-11.35 |
-13.51 |
0.12 |
|
LDDD |
-10.79 |
-12.6 |
0.16 |
-11.35 |
-13.49 |
0.13 |
|
Unspecific low back pain |
-13.2 |
-11.87 |
0.39 |
-14.93 |
-12.48 |
0.14 |
|
DLIDWM |
-13.87 |
-11.78 |
0.19 |
-14.7 |
-12.58 |
0.23 |
|
Surgery |
-10.66 |
-12.53 |
0.18 |
-11.59 |
-13.3 |
0.25 |
|
Family low back problems |
-12.14 |
-12.05 |
0.95 |
12.92 |
12.89 |
0.98 |
|
Current family problems |
-12.04 |
-12.12 |
0.95 |
-11.49 |
-13.28 |
0.25 |
|
Feel need to lose weight |
-13.16 |
-9.55 |
< 0.01 |
-14.22 |
-9.75 |
<0.01 |
|
Drink alcoholic beverages |
-11.62 |
-12.79 |
0.32 |
-12.91 |
-12.91 |
1.00 |
|
Smoking |
-10.48 |
-12.71 |
0.09 |
-12.46 |
-13.08 |
0.66 |
|
History of emotional or mental health counseling |
-14.68 |
-11.29 |
0.01 |
-16.39 |
-11.8 |
<0.01 |
|
Time delay to evaluation > 1 month |
-11.93 |
-19.82 |
<0.05 |
-12.68 |
-23.35 |
0.01 |
|
Time delay to evaluation > 3 months |
-11.33 |
-17.02 |
<0.01 |
-12.14 |
-17.79 |
<0.01 |
|
Age > 39 |
-11.21 |
-13.55 |
>0.05 |
-11.67 |
-14.91 |
0.01 |
|
Female Gender |
-12.95 |
-11.44 |
0.2 |
-14.62 |
-11.57 |
0.02 |
|
Average mean Oswestry scores and dependence of various factors at year 1 and 2; P-values for the respective statistical analysis (Student t-Test) are shown. Abbreviations: LDDD: Lumbar Degenerative Disc Disease; DLIDWM: Displacement of Lumbar Intervertebral Disc without Myelopathy. |
||||||
When corrected for gender, seven male and three female factors were correlated with beneficial changes in Oswestry scores. For males, the factors increased educational level, higher expectation of complete and moderate pain relief, and liking one’s job (at year 1 follow-up) were positively correlated with an improved chronic low back pain. In contrast, binary time of injury onset to initial evaluation in the program >1 month (at year 2 follow-up) and >3 months, and age >39 years were negatively associated with low back pain improvements. For females, the factors that were significantly correlated with improving low back pain included a perceived need for weight loss (at year 1 follow-up) and having previous emotional or mental counseling (at year 2 follow-up). The factor most negatively impacting back pain improvement for females was the binary time of injury onset to initial evaluation in the program >3 months (at year 1 follow-up) (ANOVA, Bonferroni-corrected).
Collective linear regression analyses were also performed on the factors that were determined significant after corrected for gender; this was done to examine potential overlap in the variable effects. Only binary age dropped from the models at 1- and 2-year follow-ups employing this approach. All other factors mentioned previously were found to be significant in their respective follow-ups and gender models.
Oswestry changes by diagnosis or within subpopulations
After initial analyses, means and standard deviations were calculated for the changes in Oswestry score by year 1 and 2, based on diagnosis and other prominent categories. Table 4 is provided for reference as a rough comparison in examining diagnostic categories. Furthermore, some commonly used factors in which these studies determined potential significance and their associated average changes are shown.
|
Table 4: Mean Oswestry score reduction depending on diagnosis and subpopulations at year 1 and 2. |
||
|
Diagnosis |
Year 1 |
Year 2 |
|
Post lumbar laminectomy syndrome |
-12.3 |
-12.8 |
|
Sacral disorders |
-11.1 |
-13.3 |
|
Thoracic or lumbosacral neuritis or radiculitis |
-10.3 |
-13.3 |
|
Spondylolisthesis |
-11.9 |
-12 |
|
Lumbar spinal stenosis |
-12.7 |
-14.1 |
|
Juvenile discogenic disease |
-9.5 |
-13.2 |
|
DLIDWM |
-13.6 |
-12.6 |
|
Unspecific low back pain |
-12.7 |
-12.9 |
|
Lumbar degenerative disc disease |
-12.5 |
-11.6 |
|
Subpopulations |
|
|
|
Workers' compensation |
-10.4 |
-11.4 |
|
Other insurance |
-12.8 |
-13.6 |
|
Previous surgery |
-10.6 |
-11.5 |
|
No previous surgery |
-12.6 |
-13.4 |
|
Males |
-11.4 |
-11.6 |
|
Females |
-13.1 |
-14.7 |
|
Do not expect complete pain relief |
-10.6 |
-11.3 |
|
Expect complete pain relief |
-13.4 |
-14.3 |
|
Average mean Oswestry scores and dependence of diagnosis and subpopulations at year 1 and 2. Abbreviation: DLIDWM: Displacement of Lumbar Intervertebral Disc without Myelopathy. |
||
Functional activity analyses
For analyses related to functional activity within the available data set (n=78/various) at follow-up evaluations of 3 and 4 months, the factor liking coworkers more correlated significantly with improved low back pain measured via FAS (P=0.03). Bonferroni correction results indicated the significant difference to be between Sometimes vs. Always (P<0.05, mean difference=24.25). Within the linear regression derivations with ANOVA, when corrected for gender, no factors were indicated to correlate with changes in FAS, thus no combined linear regression analyses were performed.
Numeric analog scales
Higher education (i.e., high school vs. some college) and being female were factors significantly associated with improving low back pain over the observation period (P<0.05), whereas a positive family history concerning low back problems was correlated with less improvement of the condition as measured by NRS scores.The linear regression with ANOVA analyses, when corrected for gender, showed that no factor was correlated with a significant change in NRS. Within the Subgroup Analysis (n=786), four factors were correlated with an improvement of back pain as assessed by NRS pain scores: history of mental or emotional health counseling, older than 39 years, and being female (P<0.05). In contrast, smoking was negatively correlated; i.e., there was less improvement of chronic low back pain in such individuals as measured by NRS scores (P<0.05). Further, linear regression with ANOVA analyses, when corrected for gender, indicated no factors were significantly correlated with changes in NRS, thus no combined linear regression could be performed.
Axial spinal unloading
Due to our laboratory’s interest in the effectiveness of the LTX 3000® axial spinal unloading device relative to this program, analyses were completed to assess the relationship between continued use of the device at each follow-up and several outcome measures including FAS and Oswestry changes, NRS pain scores, back pain improvement, and changes in pain intensity.
Linear regression analysis of the available data set for these parameters (n values varied for each follow-up) was used. Purchase of the device was not consistently correlated with any factors, however having said that, the continued use of the device was more consistently correlated with improved outcomes for some factors at the follow-up controls at year 1 and 2 (P<0.003). These findings are summarized in Table 5.
|
Table 5: Various outcome changes based on LTX 3000® permanent access and continued axial spinal unloading status. |
||||||
|
|
LTX 3000® Permanent Access Acquired before or at: |
|||||
|
|
1 month |
2 months |
3 months |
4 months |
1 year |
2 years |
|
Category |
P Value |
P Value |
P Value |
P Value |
P Value |
P Value |
|
Fraction with permanent access |
260/2113 |
100/460 |
439/1196 |
5/21 |
1107/1731 |
1076/1511 |
|
FAS score change |
0.28 |
0.14 |
0.65 (n=101) |
NA |
NA |
NA |
|
VAS score change |
0.64 |
0.75 |
0.3 |
0.095 |
0.58 |
0.56 |
|
Oswestry score change |
0.4 |
0.49 |
0.73 |
0.03 |
0.04 |
0.06 |
|
Back pain improved |
0.43 |
0.78 |
0.82 |
0.98 |
< 0.001 |
< 0.0001 |
|
Pain intensity difference |
0.22 |
0.99 |
0.38 |
0.07 |
0.27 |
0.53 |
|
|
Still Unloading at: |
|||||
|
|
1 month |
2 months |
3 months |
4 months |
1 year |
2 years |
|
|
P Value |
P Value |
P Value |
P Value |
P Value |
P Value |
|
Fraction still unloading |
2001/2113 |
416/460 |
1180/1196 |
21/21 |
1024/1731 |
825/1511 |
|
FAS score change |
0.02 |
0.33 |
0.35 (n=101) |
NA |
NA |
NA |
|
VAS score change |
0.92 |
0.2 |
0.7 |
NA |
0.58 |
< 0.05 |
|
Oswestry score change |
< 0.0001 |
0.1 |
0.9 |
NA |
0.24 |
0.14 |
|
Back pain improved |
< 0.01 |
0.17 |
0.01 |
NA |
< 0.01 |
0.0001 |
|
Pain intensity difference |
< 0.001 |
0.87 |
0.56 |
NA |
0.64 |
0.86 |
|
Permanent access to the LTX 3000® improved back pain via each measure at each significant outcome in the follow-up evaluation at year 1; continued use of the LTX 3000® improved back pain via each measure at each significant outcome, except VAS in the follow-up evaluation at year 2. Abbreviations: FAS: Functional Activities Scale; VAS: Visual Analog Scale. |
||||||
DISCUSSION
Outcomes research on back pain remains a daunting task, due in part to the broad range of disorders that can present with this symptom [19]. In our retrospective analysis of a database of over 6,000 patients enrolled in a prototype multifaceted rehabilitation program, we were able to subdivide data into unique groups associated with a large number of associated variables. Overall, this multidisciplinary outpatient program resulted in numerous significant positive long-term outcomes for patients with low back pain.
In their study, Fairbank and coauthors indicated no clear evidence that primary spinal fusionsurgery was any more beneficial than intensive rehabilitation [20]. It further strengthened the argument that, relative to usual care or non-multidisciplinary rehabilitation, in most cases multidisciplinary rehabilitation is better suited to ultimately: 1) improve functioning; 2) reduce associated back pain;and/or 3) decrease episodes of work loss in patients with chronic low back pain [21,22]. In the current study, available FAS and Oswestry data obtained during treatment and post-treatment periods indicated statistically significant improvements in overall patient scores in association with the multidisciplinary outpatient rehabilitation program. However, the lack of reference to a control group in these retrospective analyses makes it difficult to compare these findings to outcomes of other standard treatment programs or the normal resolution of the disease process. Furthermore, we recognize as an additional limitation that non-uniform results identified in this database across follow-up evaluations may have compromised our ability to identify significant changes in outcome measures relative to time-dependent correlations. In other words, a factor of interest may have been represented by a non-linear relationship such that it was initially factored into the overall outcomes, but later its importance dissipated or vice versa. We suggest that more data and analyses are needed to elucidate such possibilities, as data collection and patient numbers in this database taper off over time, potentially introducing a selection bias for certain types of individuals or conditions. Nevertheless, the lessons learned by such a retrospective analysis are essential and important for designing a prospective study and database. One of the greatest difficulties in our retrospective analysis was defining a large enough complete data set and gathering the patient records with all these factors. In our measurements, incomplete data for any of the factors of interest greatly decreased the number of patients we were able to include while maintaining a constant number of records (Subgroup Analysis). In addition, because the outcomes of statistical significance based on the chosen factors differed when using different n values (Total Analysis vs. Subgroup Analysis), we can only conclude that the factors analyzed using a complete data set (Subgroup Analysis) were significant. Those deemed significant using the entire data set with varying n values demonstrate promise as indicators for this purpose. However, further data are necessary.
Studies have shown that modified Oswestry Disability Questionnaires have high reliability, validity, and sensitivity for change in measuring outcomes in patients with low back pain [23]. The FAS (SF36) has been examined as an outcome measure in low back pain patients and its reliability and validity has also been well established [23]. The Oswestry, in addition to the FAS and NRS, provided a comprehensive means of assessing relative efficiencies of the program, but also aided in capturing patient’s “perceived” disability and progress which is considered key when treating pain and/or functionally disabling conditions. The use of such standardized scales also allowed for comparisons with other therapeutic programs or approaches and could help determine the optimal criterion to be employed in subsequent prospective analyses.
We consider here that, in general, the tested program offers an effective approach for patients whose back pain has not resolved after 12 weeks. Yet, the earlier enrollment in the program was correlated with improved outcomes as well. The current consensus regarding treatment options for back pain typically specifies a conservative approach (e.g., physical therapy and rehabilitation) initially, except in specific cases where surgical intervention is medically required. From analyses of the subpopulation of patients with complete data sets (n=786) using a linear regression model, we identified a statistically significant improvement of low back pain measures. The greatest improvements were observed for females having previous counseling (at year 2), patients perceiving a need for weight loss (at year 1), and those with a shorter binary time onset to initial evaluation. For the male population, a higher education level, higher expectation of pain relief, liking one’s job, and a shorter time onset to evaluation were all significantly associated in the final linear regression model. Though the overall linear regression values demonstrate a modest overall benefit, one should consider that because of the numerous, heterogeneous factors contributing to the problem of chronic back pain, achieving even modest R2 values positively demonstrates great promise in the realm of multidimensional, standardized treatment options. Yet, it is also of interest to note that both FAS and NRS scores did not significantly correlate with any of the individual factors we examined when the database was corrected for gender. Furthermore, the factors that were found to be statistically significant in the Total Analysis data set of n=6,340, but not in the Subgroup Analysis with complete data sets (n=786), should be evaluated with caution and used only as potential indicators instead of proven correlations until further data are available. Relative to our analyses on enhanced benefits of axial spinal unloading device use, we noted statistically significant improvements, e.g., an overall back condition parameter with self-administered unloading therapy (traction) at early follow-ups and advantages relative to back pain reduction over time. Interestingly, a patient’s permanent access to the axial spinal unloading device was not well correlated to any of the outcome measures over time, but was found to be statistically significant at the follow-up evaluation after one or two years for controlling back pain. Finally, as pointed out earlier, a control group was not included into these analyses as this was a retrospective study. In any planned prospective study, one should include a non-intervention group to determine numbers and rates for spontaneous disease resolution.
Table 5: Various outcome changes based on LTX 3000® permanent access and continued axial spinal unloading status.
| LTX 3000® Permanent Access Acquired before or at: | ||||||
| 1 month | 2 months | 3 months | 4 months | 1 year | 2 years | |
| Category | P Value | P Value | P Value | P Value | P Value | P Value |
| Fraction with permanent access | 260/2113 | 100/460 | 439/1196 | 5/21 | 1107/1731 | 1076/1511 |
| FAS score change | 0.28 | 0.14 | 0.65 (n=101) | NA | NA | NA |
| VAS score change | 0.64 | 0.75 | 0.3 | 0.095 | 0.58 | 0.56 |
| Oswestry score change | 0.4 | 0.49 | 0.73 | 0.03 | 0.04 | 0.06 |
| Back pain improved | 0.43 | 0.78 | 0.82 | 0.98 | < 0.001 | < 0.0001 |
| Pain intensity difference | 0.22 | 0.99 | 0.38 | 0.07 | 0.27 | 0.53 |
| Still Unloading at: | ||||||
| 1 month | 2 months | 3 months | 4 months | 1 year | 2 years | |
| P Value | P Value | P Value | P Value | P Value | P Value | |
| Fraction with permanent access | 2001/2113 | 416/460 | 1180/1196 | 21/21 | 1024/1731 | 825/1511 |
| FAS score change | 0.02 | 0.33 | 0.35 (n=101) | NA | NA | NA |
| VAS score change | 0.92 | 0.2 | 0.7 | NA | 0.58 | < 0.05 |
| Oswestry score change | < 0.001 | 0.1 | 0.9 | NA | 0.24 | 0.14 |
| Back pain improved | < 0.01 | 0.17 | 0.01 | NA | < 0.01 | 0.0001 |
| Pain intensity difference | < 0.001 | 0.87 | 0.56 | NA | 0.64 | 0.86 |
| Permanent access to the LTX 3000® improved back pain via each measure at each significant outcome in the follow-up evaluation at year 1; continued use of the LTX 3000® improved back pain via each measure at each significant outcome, except VAS in the follow-up evaluation at year 2. Abbreviations: FAS: Functional Activities Scale; VAS: Visual Analog Scale. |
||||||
CONCLUSION
Apart from the limitations noted above, overall, the results from these retrospective analyses demonstrate that this multifaceted treatment program should be considered as an effective standard of care for a wide variety of individuals with underlying chronic low back pain. However, there were notable improvement differences found in each outcome variable over time; e.g., surgical avoidance (at least, over 80% of patients referred to the program to avoid surgery were successful at each individual follow-up evaluation), return to work, and decreased pain medication usage. Another important consideration is that a portion of the referred population came from several referring surgeons that may have previously appreciated the benefit of the program as part of their post-surgical regimen to maximize recovery and positive outcomes. The present investigation supports the notion that such multidisciplinary rehabilitation programs (those that track the aforementioned indications) can lead to medical benefits and thereby also to cost reduction. The patient satisfaction ratings at the follow-up evaluation at one (89.1%) and two months (90.9%) may indicate this program’s potential for improved success and patient participation, as compliance of the patients is crucial therein. In conclusion, our retrospective analysis suggests that a multidisciplinary outpatient rehabilitation program offers a valid treatment strategy for chronic back pain sufferers, and that various subpopulations could gain added benefit using this approach.
ACKNOWLEDGEMENTS
We would like to thank Gary Williams for his help with data analyses, Monica Mahre with the manuscript preparation, and Spinal Designs International for providing unrestricted access to their patient database. Financial support was provided by the Institute for Engineering in Medicine (University of Minnesota) and by an unrestricted gift for research from Spinal Designs International, Inc.