A Case of Cerebral Venous Sinus Thrombosis Secondary to Norethisterone intake and Iron Deficiency Anemia
- 1. Department of Pediatric Neurology, Bangabandhu Sheikh Mujib Medical University, Bangladesh
- 2. Department of Pediatrics, Bangabandhu Sheikh Mujib Medical University, Bangladesh
Abstract
Cerebral venous sinus thrombosis (CVST) is a rare stroke-like syndrome which is associated with hypercoagulable states. We present a 13 years old girl who had severe headache, lower motor type of facial palsy and history of menorrhagia which was treated with norethisterone. She was moderately pale and had papilloedema. Vusculitic, thrombophillia and sepsis screening were normal except evidence of iron deficiency anemia. MRI of brain showed dense triangle sign and MRV showed occlusion of superior sagittal sinus, right transverse and both sigmoid sinuses. She was diagnosed to have multiple cerebral venous sinus thrombosis due to iron deficiency anemia and norethisterone enanthate. She was treated with naproxen, acetazolamide, enoxaparin followed by rivaroxaban and on iron supplementation. She made a full recovery in 1 month.
Keywords
• Cerebral
• Venus
• Thrombosis
• Secondary
CITATION
Fatema K, Rahman MM, Akhter S, Islam MI, Begum S (2018) A Case of Cerebral Venous Sinus Thrombosis Secondary to Norethisterone intake and Iron Deficiency Anemia. JSM Pediatr Neurol 2(1): 1014.
INTRODUCTION
Cerebral venous sinus thrombosis (CVST) is a rare stroke-like syndrome with significant morbidity and mortality. This entity is associated with hypercoagulable states and can present with a myriad of signs and symptoms ranging from simple headaches to localizing neurologic deficits, frank seizures, and coma. Prompt recognition and treatment can prevent significant morbidity and years of life lost [1].
It is calculated that CVST incidence rates in autopsy series are 7 cases per million children and infants, while in clinical series the incidence rate is 10 times greater. Oral contraceptives is a risk factor [2,3]. Other associated risk factors include infection, genetically acquired pro-thrombotic states [1]. We present a case of a CVST occurring in a 13 year old girl who had history of taking norethisterone and iron deficiency anemia (IDA).
CASE PRESENTATION
A 13 year old girl, third issue of her non consanguineous parents, presented with severe headache and vomiting for two months. Headache was diffuse, progressive, dull aching in nature. She also developed right sided lower motor type of facial palsy for two weeks. She had no history of recent fever, trauma, unconsciousness, blurring of vision, diplopia, ear infection, sinusitis, arthritis, skin rash, photophobia, oral ulcer, contact with TB patient, and no known congenital heart disease previously. There was no family history of migraine, brain tumor or vasculitis disorder. She had history of menorrhagia and was taking norethisterone for two and half months.
On physical examination, the girl was ill looking, co-operative, moderately pale. She had no jaundice, cyanosis, clubbing, edema or koilonychia. Vitals were within normal limit. Skin survey revealed BCG mark was present with no other skin lesion. There was right sided lower motor type of facial palsy (Figure 1).
Figure 1: 13 year girl with facial nerve palsy of right side.
Signs of meningeal irritation were absent. Ophthalmoscopy revealed bilateral papilloedema.
INVESTIGATION PROFILE
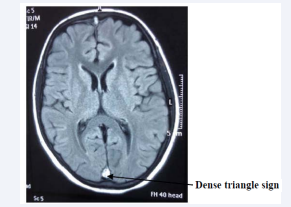
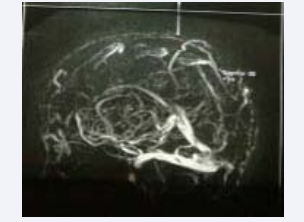
MRI of brain showed TI and FLAIR hyperintense signal change in superior sagittal sinus and in the sulci of right parietal region over the area of Vein of Troland. It also showed the classical ‘Dense Triangle sign ‘in the posterior part of the superior sagittal sinus which corresponds the fresh thrombus. Thus it suggested thrombosis of superior sagittal sinus and right Vein of Troland (Figure 2). The MRV showed non visualized superior sagittal sinus, right transverse sinus and both sigmoid sinuses which were due to thrombotic occlusion (Figure 2).
Figure 2: MRI of brain: Dense triangle sign.
Complete blood count showed hemoglobin was decreased (6.0 gm/dl), WBC: normal, platelet: increased (6,40,000/dl), HCT 25.40%, MCV 59.90 fl, MCH 16.00 pg, MCHC 26.80 g/dl, RDW 21.00%, ESR 61 mm in 1st hour. PBF showed, RBC: gross anisopoikilocytosis with many microcytic, hypochromic red cells, good number of elongated cells, few pencil shaped cells, WBC: mature.
Iron Profile
Serum Iron: 22 micro g/dl. Serum Ferritin: 9 ng/dl, TIBC: 550 micro g/dl, Prothrombin Time: Control: 12 sec, patient: 13 sec, INR: 1.09, APTT: normal, Protein C, Protein S, Antithrombin III: normal, ECG: Sinus tachycardia, fasting lipid profile: normal, 24 hrs. UTP: normal. ANA - Positive, Anti-DS DNA: Negative, anti phospholipids Ab - Negative, ENA Profile - Negative, anti cardiolipin Ab - Negative. Liver and renal function test: normal.
Treatment
On admission: norethisterone was discontinued. She was treated with naproxen for headache and acetazolamide for increased intracranial pressure. One unit of packed RBC was given as she had anemia. She was treated with subcutaneous enoxaparin (LMW heparin) 26 mg 12 hourly for 7 days with regular monitoring of PT and APTT. Then tab rivaroxaban was added at the dose of 10 mg daily for 3 months.
Outcome and follow-up
With treatment, the headache of the patient subsided, papilloedema was no longer found. Facial nerve palsy improved. She was discharged with oral medications. Her condition remained well throughout her follow-up visits. Anticoagulation was continued for 3 months as recommended. She was also advised to avoid prothrombotic drugs like norethisterone. For menorrhagia she was advised to take tranexamic acid and acetaminophen. A follow-up MRI brain with a venogram was suggested after 3 months.
DISCUSSION
Cerebral venous sinus thrombosis is a rare stroke-like syndrome that can present a diagnostic dilemma. Presentation is widely variable including isolated headache, mood changes, cranial nerve palsies, ocular complaints, aphasia, encephalopathy, TIA/stroke symptoms, seizures or frank coma. Headache is the most consistent presenting complaint and is classically described as slow-onset, dull, localized and worse with recumbency [1]. Our case presented with headache, which was progressive. Later, she also had facial nerve palsy which is a rare presentation in CVST.
Cranial nerve palsy as an isolated manifestation of CVST has been attributed to the elevated intracranial pressure, extension of thrombosis to venous channels or direct pressure from the clot itself [4]. Kuehnen et al., have reported five patients who were initially evaluated for etiologies of single/multiple cranial nerve palsies finally turning out to be the cases of the ipsilateral transverse and sigmoid sinuses thrombosis, on evaluation. According to Kuehnen et al., thrombosis of the lateral sinus can produce venous congestion and dilatation of the cranial nerve veins, this causes reversible compromised oxygen or glucose consumption within the cranial nerve tissue due to edema and backpressure, and due to this cranial nerve palsies will develop [5]. Straub et al., have described a 17-year-old lady with LMN facial palsy with ipsilateral TS thrombosis; they evaluated the patient with transcranial magnetic stimulation and concluded that the facial palsy was due to the transient neuropraxia in the intracranial segment of the nerve [6]. Our patient presented with thrombosis of superior sagittal sinus, right transverse sinus and both sigmoid sinuses which can thus explain the right sided facial palsy, headache and papilloedema.
Risk factors related to CVST are diverse. At least one risk factor could be identified in more than 85% of patients with CVST [7]. The common risk factors are pregnancy and puerperium, drugs like oral contraceptives, steroid, L asperginase, hormone replacements, malignancy, systemic inflammatory disease like Systemic lupus erythematosis, infectious diseases, hematological disorders like polycythemia, dehydration, coagulation disorders , congenital heart diseases, head trauma etc [8]. In our case the patient’s blood and urine investigations were within normal limits except IDA and thrombocytosis. She had been taking norethisterone for 6 months for menorrhagia. These two may be the risk factors in this case.
The drug norethisterone enanthate, a first-generation progestogen, has a lower risk of causing venous thrombosis when compared with third-generation progestogens. It has been shown to be partly metabolised to ethinyloestradiol [9-11]. This oestrogen compound (ethinyloestradiol) is thought to cause the increased risk of thrombosis by activating protein C resistance comparable with the resistance caused by a factor V Leiden mutation [12].
Our patient also had IDA along with thrombocytosis. This may be a risk factor for CSVT. Sudharani Busani et al., described a 28 year-old female who presented solely with a new onset headache due to transverse sinus thrombosis. Thrombophilia work-up was normal. She had no identifiable acquired causes of thrombosis. The patient demonstrated severe iron deficiency anemia secondary to myoma uteri causing menorrhagia [13]. The proposed mechanisms of IDA causing CSVT is it occasionally leads to thrombocytosis, which is associated with a hypercoagulable state [14]. Again it may also induce a hypercoagulable state by altering pattern of blood flow within the vessels due to decreased deformability and increased viscosity i.e. thickness of microcytic RBC [15]. Low hemoglobin causes poor oxygenation. As a result, anemic hypoxia consequent to IDA could precipitate situations of increased metabolic stress predominantly in susceptible areas of the brain like basal ganglia and thalamus, due to end arterial blood supply [16].
Various imaging techniques are used to confirm the diagnosis with CT angiography and MRI/MRV being most sensitive and specific. The “Dense Triangle Sign” is a hyperdense triangular or round shape in the posterior superior sagittal sinus that has been described in non-contrast head CT scans. “Empty Delta Sign” seen with contrast-enhanced CT scan is a triangular ring of enhancement with a central region lacking contrast in the posterior superior sagittal sinus [17]. In case of our patient, the MRI showed T1 and FLAIR hyperintense signal in superior sagittal sinus and area of vein of Troland. It also showed the classical ‘Dense Triangle sign ‘in the posterior part of the superior sagittal sinus which corresponds the fresh thrombus (Figure 2). Her MRV showed non visualized superior sagittal sinus, right transverse sinus and both sigmoid sinuses which confirmed the diagnosis (Figure 3).
Figure 3: MRV: non visualized superior sagittal sinus, right transverse sinus and both sigmoid sinuses suggestive of thrombotic occlusion.
We treated our patient with naproxen for headache and for increased ICP we have given acetazolamide. Heparin is safe and effective in mortality reduction even in those with small parenchymal hemorrhages in CVST [18]. After acute phase use of oral anticoagulant is recommended unless there is clear contraindication for about 3 months. Oral anticoagulant usually used is Warfarin, which need meticulous monitoring [19]. In addition, rivaroxaban is also approved for the treatment of acute coronary syndromes [20]. It is a newer anticoagulant which is a direct factor Xa inhibitor, safer than the other anticoagulants and need lesser coagulation monitoring [21]. In our case we used subcutaneous LMW heparin followed by oral rivaroxaban. With these medications our patient showed full clinical recovery. She was also advised to avoid norethisterone preparations and management for IDA was given. The prognosis of CVST is usually favorable with more than 80 % of the patients, as in our case, having a good neurological outcome [22].
CONCLUSION
Our patient is a rare case of CVST who had history of taking norethisterone and IDA as risk factor. If prompt identification and treatment is done, this life threatening condition can be easily managed with full recovery for most patients.
REFERENCES
1. Ferro JM, Canhao P, Stam J, Bousser MG, Barinagarrementeria F, ISCVT Investigators. Prognosis of cerebral vein and dural sinus thrombosis: results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT). Stroke. 2004; 35: 664-670.
3. Kalbag R, Woolf A. Cerebral venous thrombosis. London: Oxford University Press. 1967.
4. Kulkarni GB, Ravi Y, Nagaraja D, Veerendrakumar M. Lower motor neuron facial palsy in cerebral venous sinus thrombosis. J Neurosci Rural Pract. 2013; 4: 224-226.
7. Piazza G. Cerebral venous thrombosis. Circulation. 2012; 125: 1704- 1709.
8. Ehtisham A, Stern BJ. Cerebral venous thrombosis: a review. Neurologist. 2006; 12: 32-38.
11. FSRH. Faculty of sexual & reproductive healthcare of the Royal College of Obstetricians and Gynaecologists Statement. Venous Thromboembolism (VTE) and Hormonal contraception. 2014.
12.de Bruijn SF, Stam J, Koopman MM, Vandenbroucke JP. Case-control study of risk of cerebral sinus thrombosis in oral contraceptive users and in [correction of who are] carriers of hereditary prothrombotic conditions. The Cerebral Venous Sinus Thrombosis Study Group. BMJ. 1998; 316: 589-592.
13.Busani S, Scott S, Neely JA, Calvo AR. Cerebral Venous Thrombosis Secondary to Severe Iron Deficiency Anemia: A Case Study. Cancer Clin Oncol. 2012: 1.
14.Gupta MK, Joseph G. Severe Thrombocytopenia Associated with Iron Deficiency. Hospital Physician. 2001: 37; 49-54.
15.Hartfield DS, Lowry NJ, Keene DL, Yager JY. Iron deficiency: a cause of stroke in infants and children. Pediatr Neurol. 1997; 16: 50-53.
17.Ferro JM, Canhao P. Etiology, Clinical Features, and Diagnosis of Cerebral Venous Thrombosis. Up To Date. 2016.
18.Ferro JM, Canhao P. Treatment and Prognosis of Cerebral Venous Thrombosis. Up To Date. 2016.
20.Committee for Medicinal Products for Human Use: Summary of opinion (post authorisation): Xarelto, rivaroxaban. 2013.
21.Samama MM, Contant G, Spiro TE, Perzborn E, Le Flem L, Guinet C, et al. Laboratory assessment of rivaroxaban: a review. Thromb J. 2013; 11: 11.