Seven Hemodialysis Patients with Covid-19 Pneumonia in a Thertiary Hospital, Istanbul, Turkey
- 1. Infectious Diseases and Clinical Microbiology, Bakirkoy Dr. Sadi Konuk Training Research Hospital, Istanbul, Turkey
Abstract
Objective: We aimed to summarize the clinical data from seven hemodialysis patients with COVID-19 pneumonia.
Methods: For this retrospective, single center study, we recruited 539 hospitalized patients who were diagnosed with COVID-19 pneumonia from March 27 to April 15, 2020 in Bak?rkoy Dr. Sadi Konuk Training and Research Hospital, Istanbul. Seven hemodialysis patients with Covid-19 pneumonia were analyzed.
Results: This study included seven hemodialysis patients of 539 cases with confirmed COVID-19, with an average age of 64 years (range, 42-83 years), including 3 females and 4 males. Among the seven patients, two cases were asymptomatic, five patients had fever and respiratory symptoms on admission . Asymptomatic patients were exposed to the virus via infected adults in their household.
Conclusion: All cases had high fever, low oxygen saturation (SO2 <93% ), high CRP, elevated ferritin and cytopenia at the seventh day of hospitalization. This suggests that cytokine storm may be more common in hemodialysis cases and the disease may progress more progressively.
Citation
Karaosmanoglu HK (2021) Seven Hemodialysis Patients with Covid-19 Pneumonia in a Thertiary Hospital, Istanbul, Turkey. JSM Renal Med 4(1): 1017.
INTRODUCTION
In late December 2019, an outbreak of COVID-19 was reported in Wuhan, a city in the Hubei Province of China. It rapidly spread, resulting in an epidemic throughout China, followed by an increasing number of cases in other countries throughout the world.
On March 11, 2020, the World Health Organization declared the COVID-19 outbreak a pandemic [1].
After the first case was reported on the 11 March 2020, The Turkish Government reported that 107,773 cases of COVID-19 had been confirmed, and 2,706 patients had died as of 25 April, 2020 [2].
The case fatality rate so far has ranged widely from 1% to 7.2% overall reaching up to 49% among the critically ill [3,4].
Risk factors for severe disease are older age and the presence of comorbidities such as diabetes, hypertension, chronic kidney disease, morbid obesity, coronary heart disease and chronic lung disease [5].
With the spread of the epidemic, the etiology, epidemiology, and clinical characteristics of COVID-19 have gradually been recognized, but the clinical and epidemiological characteristics of COVID-19 in hemodialysis (HD) patients is still limited, with only sporadic literature reported [6,7].
Here, we aimed to summarize the clinical data from seven hemodialysis patients with COVID-19 pneumonia.
METHODS
For this retrospective, single center study, we recruited 539 hospitalized patients who were diagnosed with COVID-19 pneumonia from March 27 to April 15, 2020 in Bak?rkoy Dr. Sadi Konuk Training and Research Hospital located in the centre of Istanbul. Seven hemodialysis patients with COVID-19 pneumonia were analyzed.
Information recorded includes epidemiological and demographic information, signs and symptoms on admission, laboratory results, CT findings, treatment measures, and outcome data from patients’ medical records. Clinical outcomes were followed up to April 15, 2020. A confirmed case of COVID-19 was defined as a positive result on high-throughput sequencing or real-time RT-PCR of nasal and pharyngeal swab specimens.
RESULTS
Demographic and clinical characteristics
This study included seven hemodialysis patients of 539 cases with confirmed COVID-19, with an average age of 64 years (range, 42-83 years), including 3 females and 4 males. Among the seven patients, two cases were asymptomatic, four patients had fever, fatique and respiratory symptoms (dispnea, dry cough) in admission . Asymptomatic patients were exposed to the virus via infected adults in their household.
All of the patients had lymphopenia, anemia, hyperferritinemia, elevated CRP in the seventh day of admission. The detailed clinical and laboratory features of patients are shown in (Table 1) .
Table 1. Characteristics of HD Patients with Covid-19 Pneumonia.
| Characteristics | Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 | Patient 7 |
| Age (year) | 59 | 71 | 79 | 78 | 52 | 42 | 69 |
| Gender | female | male | female | female | male | female | male |
| Lenght of stay (day) | 16 | 17 | 14 | 19 | 22 | 15 | Still ICU |
| Oxymetry saturation (At admission)) | 98 | 95 | 93 | 96 | 93 | 96 | 91 |
| Oxymetry saturation (7. day of admission) | 92 | 90 | 92 | 91 | 89 | 92 | 88 |
|
Signs and symptoms at admission
|
- - - - - |
+ + + + + |
+ + - + - |
- - - - - |
+ + - + - |
+ - + + - |
+ + + + - |
|
Laboratory Findings
|
410
|
610
|
900
|
780
|
870
|
560
|
401
|
| CT Findings Ground-glass opacity |
+ | + | + | + | + | + | + |
Treatment
All of the patients were treated with oseltamivir+ hydroksichlorokine+ azytromycine. Favipravir was added to treatment in four patients who had low oksigene saturation in the room air ( <%90). IVIG treatment was added in one critically ill patient who transferred to intensive care unit in ninth day of hospitalization.
CT Findings
CT images of six patients showed multiple ground-glass opacities were shown in (figure 1).
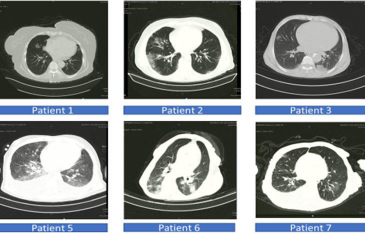
Figure 1 Characteristics of HD Patients with Covid-19 Pneumonia.
DISCUSSION
Currently, there are few reports of hemodialysis patients with COVID-19. We describe seven HD patients with COVID-19 pneumonia in our hospital, representing 1,5 % of our hospitalized COVID-19 cases at the time.
The dominant clinical features of COVID-19 were fever, cough, and fatigue, while congestion, rhinorrhea, sore throat and diarrhea are rare [8-11].
The most frequently reported finding on CT imaging was ground-glass opacities, particularly bilateral opacities impacting three or more lobes [12,13].
In our study, HD patients had similar symptoms, signs and the radiological findings on admission.
Lymphopenia is the most common laboratory finding in COVID-19 and is found in as many as 83% of hospitalized patients and lymphopenia, high CRP, and high ferritin levels may be associated with greater illness severity [14,15].
Bataille S et al reported that high ferritin levels may be associated with COVID-19 in HD patients, and that even ferritin levels can be used in COVID-19 screening in HD patients [16].
In all our cases, the level of Ferritin is over 1000 ng/mL .
Previous studies have revealed that severe illness predominantly occurs in adults with advanced age or underlying medical comorbidities. and hyperinflammation and cytokine storm may played an important role in the disease progression [17,18].
Most of our HD cases are of advanced age and the disease has been severe.
All of the patients were hospitalized for more than 2 weeks, one case was transferred to the intensive care unit.
Previous studies on COVID-19 associate fever, hypoxia, high CRP, elevated ferritin and presence of cytopenia with MAS / sHLH-like cytokine storm syndrome [19-21].
All HD cases had high fever, low oxygen saturation (SO2 <93% ), high CRP, elevated ferritin and cytopenia at week one.
This suggests that cytokine storm may be more common in HD cases and the disease may progress more progressively.
Antiviral treatments were given to our cases and none of them were given IL-6 or IL-2 inhibitors (tocilizumab or anakinra), but only a critically ill case was given intravenous immunoglobulin (IVIG) in intensive care.
CONCLUSIONS
It is clear that in HD COVID-19 patients, immunomodulating agents can be put on the agenda more in the treatment, but in cases where the presence of bacterial infection cannot be fully eradicated, immunosuppressive effects will cause reservations.
We think that larger series are needed in this regard.
REFERENCES
2. https://covid19.saglik.gov.tr/https://covid19.saglik.gov.tr.
4. Onder, G., G. Rezza, and S. Brusaferro, Case-Fatality Rate and Characteristics of Patients
5. Dying in Relation to COVID-19 in Italy. JAMA. 2020; 18: 1775-1776.
14. https://pubmed.ncbi.nlm.nih.gov/32053470/
15. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7266766/
21. Cron R Q, Chatham W W. The Rheumatologist’s Role in Covid-19. J. Rheumatol. 2020; 47: 639-642.








































































































































