Earlier Detection of Syphilis: Every 3-Month Screening with MSM and HIV
- 1. Department of Medicine, Loma Linda University Medical Center, USA
- 2. Department of Infectious Disease, Jerry L. Pettis Memorial VA Medical Center (JLP VAMC), USA
- 3. Department of Infectious Disease, Jerry L. Pettis Memorial VA Medical Center (JLP VAMC), USA
- 4. Department of Infectious Disease, Jerry L. Pettis Memorial VA Medical Center (JLP VAMC), USA
- 5. Department of Medicine, Loma Linda University Medical Center, USA
- 6. Department of Infectious Disease, University of California, USA
- 7. Department of Infectious Disease, Jerry L. Pettis Memorial VA Medical Center (JLP VAMC), USA
Abstract
The 2021 Sexually Transmitted Infectious (STI) Guidelines advise syphilis screening every 3-6 months despite a surge of rapid-onset syphilis symptoms in men who have sex with men (MSM) infected with human immunodeficiency virus (HIV). A retrospective chart review of the HIV Clinic Care Registry at Jerry L. Pettis Memorial Veterans Administration Medical Center (JLP VAMC) was conducted from 2002 to 2016. In 2004, Rapid Plasma Reagin (RPR) assay screening changed yearly to every 3 months. A total of 155 cases of syphilis occurred in 126 HIV-infected men; 81% were MSM, and 69% had prior syphilis. As many as 54.8% were virally suppressed, and 57% had CD4 counts greater than 400. After switching from yearly to every three-month screening, the percentage of symptomatic patients decreased from 71.4% to 41.9%. Of the 26 episodes of neurosyphilis, 11 showed ocular involvement. Increased screening has reduced the prevalence of symptomatic syphilis. This study included many patients with both neurosyphilis and ocular syphilis. Shortening the screening intervals in MSM and HIV-infected individuals will help to identify patients prior to developing symptomatic syphilis.
Keywords
• Syphilis
• Sexually Transmitted Infections
• HIV Infection
• Screening
• Neurosyphilis
• Ocular Syphilis
Citation
Carr K, Ing M, Wong B, Aung G, McCormack M, et al. (2025) Earlier Detection of Syphilis: Every 3-Month Screening with MSM and HIV. JSM Sexual Med 9(3): 1159.
INTRODUCTION
According to the Centers for Disease Control and Prevention (CDC), symptomatic syphilis infections have been increasing over the past few years, despite expanded screening and prevention efforts among MSM and those infected with HIV. From to 2014-2015, the national incidence of syphilis increased by 17.7%, the highest rate since 1994 [1]. Despite the 2015 STI guidelines increasing screening to every three to six months, after the pandemic, the rates of early syphilis in California increased by 13.2 percent from 2020 to 2021 [2]. There is also an alarming rise in neurosyphilis and ocular syphilis, suggesting a re evaluation of screening efforts [2]. Prior to 2015, the screening guidelines suggested yearly testing for high-risk groups [3-5]. In 2010, a landmark Australian study showed that among MSM in an HIV clinic, every 6-month screening increased the number of patients diagnosed with early asymptomatic syphilis from 21% (3 of 14) to 85% (41 of 48) with p=0.006 [6]. A 2015 study in Toronto noted that MSM rates of syphilis were 11% and 3.4% among those with and without HIV co-infection, respectively [7]. In 2015, the screening recommendation for this group changed from yearly to every three to six months, which has not changed with the updated 2021 STI guidelines [8]. A study conducted among the Canadian population showed that syphilis elimination could be achieved more easily with every three months of screening, requiring only 23% population coverage as opposed to 39% with every six-month screening [9,10]. A systematic review found that increased syphilis testing increased detection of asymptomatic early syphilis (OR 2.3-21) [11]. Every three to six months, screening since 2015 aimed to reduce the amount of symptomatic syphilis nationally. However, from 2020 to 2021, early syphilis (TES) cases in California increased by 13.2 percent [12]. The most concerning finding is a very high incidence of ocular syphilis. From 2011 to 2019, the incidence of syphilis, particularly ocular syphilis, increased. There was a low incidence in 2011 (0.08 per 100,000 population), but it increased in 2019 (0.23 per 100,000 population; p= .04) [13]. Literature suggests that the incidence of ocular syphilis has increased recently, but this was seen in the Inland Empire in California, especially at the Jerry L. Pettis Memorial Veterans Administration Medical Center (JLP VAMC) many years prior to the national increase in symptomatic syphilis cases. Our study aimed to determine whether an increased frequency of screening every three months could result in earlier detection of asymptomatic syphilis, and thus reduce the progression to symptomatic syphilis, particularly neurosyphilis.
METHODS
A retrospective chart review of the HIV Clinic Care Registry at the JLP VAMC was conducted from 2001 to 2016. Yearly screening occurred from 2001 to 2004, and evaluations were performed every three months from 2004 to 2016. This created cohorts of patients before and after the intervention. The patients were classified according to their symptoms and syphilis stage at the time of diagnosis. The examinations included a Rapid Plasma Reagin (RPR) assay and confirmatory treponemal syphilis serology. A new case of asymptomatic syphilis was diagnosed by either a new positive non-treponemal titer confirmed by a treponemal confirmatory test or in a patient with a persistently positive non-treponemal titer with a subsequent two-fold increase. Staging was based on symptoms, and appropriate antibiotic therapy with penicillin G was initiated. Symptomatic infections include primary, secondary, and any form of neurosyphilis. Asymptomatic syphilis includes early and late latent syphilis, excluding neurosyphilis. Other data collected included age, sexual partners, ethnicity, previous syphilis diagnosis, CD4 count, and viral load.Neurosyphilis was diagnosed based on many factors, including clinical presentation, lack of an appropriate serological response to late-latent syphilis treatment, and lumbar puncture results. For each neurosyphilis care, prior stages of the same disease course were excluded and CD4 and viral loads were noted at the time of the highest RPR value, which often coincided with the time of diagnosis. Ocular syphilis was confirmed by ophthalmologic examination or by improvement of visual symptoms after treatment with two weeks of high-dose intravenous penicillin G. Careful data notation concerning all neurosyphilis cases was retained, as there was concern about noncompliance issues with return visits and refusal of initial lumbar puncture. Due to some study findings, neurosyphilis patients were further divided into those that progressed rapidly, those who had a prior RPR within six months, and those who had a last RPR over seven months prior to neurosyphilis. The characteristics of each group were compared.
RESULTS
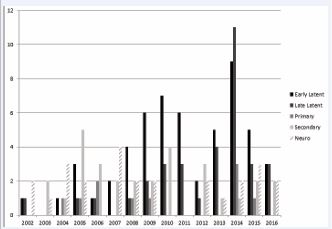
From 2002 to 2016, 155 cases of syphilis were diagnosed among 126 men with HIV infection. There were no cases of HIV infection in the females. Of the subset before the intervention in 2004, 71.4% (n=5 of 7) were symptomatic, including three with neurosyphilis. After increasing the screening every three months, only 41.92% (n=61 of 148) had symptomatic disease, including 24 with central nervous system (CNS) involvement. The types of syphilis diagnosed annually are shown in Figure 1.
Figure 1 Percentage of HIV Clinic Patients Diagnosed with Various Stages of Syphilis by Year (2002-2016) *Number of syphilis cases exceeding the number of subjects due to multiple reinfections.
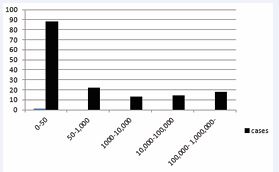
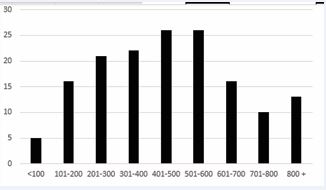
Most subjects were MSM (81%), Caucasian (71%), over the age of 50 years (56%), and 70% had a history of syphilis. Viral suppression and ART adherence were observed in 55% of the patients, and 57% had CD4 counts > 400. This is illustrated in Figure 2 and Figure 3. The remaining patient characteristics are presented in Table 1
Figure 2 Number of syphilis cases (n=155) with specific viral load ranges.
Figure 3 Number of syphilis cases (n=155) with specific CD4 ranges.
Table 1: Syphilis characteristics.
|
Number of Cases |
(n=155) and % |
|
Male |
155 (100%) |
|
Ethnicity |
|
|
Caucasian |
109 (86.5) |
|
African American |
18 (14.0) |
|
Hispanic |
23 (18.0) |
|
Asian/Pacific Islander |
3 (2.3) |
|
American Indian/Alaskan |
2 (1.5) |
|
Sexual Partners |
|
|
MSM |
125 (80.6) |
|
MSW |
20 (12.9) |
|
Both |
8 (5.2) |
|
Unknown |
2 (1.3) |
|
Age range |
|
|
20-29 |
6 (3.9) |
|
30-39 |
17 (11.0) |
|
40-49 |
45 (29.0) |
|
50-59 |
41 (26.5) |
|
60-69 |
40 (25.8) |
|
70-79 |
6 (3.9) |
Neurosyphilis was diagnosed in 26 patients, 85% of whom were symptomatic. Eleven patients had ocular syphilis infections. The two patients with recurrence had previously received adequate treatment. Ophthalmology confirmed eight cases, and the remaining three had symptomatic improvement after penicillin treatment. The clinical manifestations documented in Table 2
Table 2: Manifestations of ocular syphilis (n=11)
|
Manifestations and concurrent symptoms |
Number of Cases (n=11) |
% of total |
|
Uveitis |
5 |
45.5 |
|
Uveitis and Vitritis |
3 |
27.3 |
|
Hemianopsia (negative MRI’s) |
2 |
18.2 |
|
Optic neuritis/Papillitis |
2 |
18.2 |
|
Rash |
3 |
27.3 |
|
Memory deficit |
2 |
18.2 |
|
Headaches |
2 |
18.2 |
|
Hallucinations |
1 |
9.1 |
|
Otic |
1 |
9.1 |
|
Ocular Recurrence |
2 |
18.2 |
*Eleven cases of ocular syphilis were diagnosed in nine patients due to two recurrences after two weeks of intravenous PCN. Eight cases were confirmed by ophthalmology, and the remaining three improved with treatment. Many patients present with more than one ocular symptom.
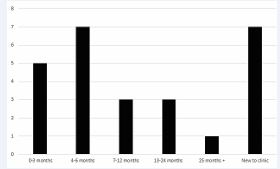
included uveitis, optic neuritis, vitritis, and loss of vision. Uveitis, alone or in combination with vitritis, was the most common finding (72%). Only 21 patients with neurosyphilis (81%) had LP, including four patients with asymptomatic disease. All patients tested positive for syphilis antibodies in their CSF. One patient with a positive Syphilis Antibody result was excluded, given that his titer responded to late-latent treatment. Among patients with neurosyphilis, Figure 10 shows 19% (n=5) had RPR testing within the previous three months, and 46% (n=12) within six months. Table 3 and Figure 4
Figure 4 Number of neurosyphilis cases (n=26) and the time range of their prior RPR at the time of diagnosis. *Patients placed in the “new to clinic” category did not have records of their last RPR value.
demonstrate how patients were divided into a rapid progression group of 12 patients who developed disease within six months, and 14 in the slow progression group with onset after severe months. Those who rapidly developed neurosyphilis had a higher RPR (1:128 vs. 1:16, X2 85.96, p<0.01), higher CD4 count (436 vs. 340, X2 9.43, p<0.01), were more likely to be virally suppressed (62% vs. 29%, X2 0.75, p=0.9-0.1), and had a higher incidence of syphilis (69 vs. 50%, X2 = 0.062, p 0.9-0.1). The clinical manifestations in both groups were similar.
Table 3: Neurosyphilis cases and comparison of those with rapid and slow progression.
|
Neurosyphilis characteristics |
Cases and % of total (n=26) |
Rapid Progression with % of group (n=12) |
Slow Progression with % of group (n=14) |
X2 |
P value |
|
Asymptomatic |
4 (15.4%) |
2 (16.7%) |
2 (14.3%) |
0.00 |
0.99 |
|
Symptomatic (including rash) |
22 (84.6%) |
10 (83.3%) |
12 (85.7%) |
0.045 |
0.9-0.1 |
|
VL<50 |
11 (42.3%) |
7 (58.3%) |
4 (28.6%) |
0.364 |
0.9-0.1 |
|
CD4 (mean) |
381 |
426 |
340 |
9.43 |
<0.01 |
|
Prior Syphilis |
15 (57.7%) |
8 (66.7%) |
7 (50.0%) |
0.063 |
0.9-0.1 |
|
RPR (median) |
1:64 |
1:128 |
1:16 |
85.56 |
<0.01 |
|
Ocular |
11 (42.3%) |
4 (33.3%) |
7 (50.0%) |
2.4 |
0.9-0.1 |
|
Rash (total) |
9 (34.6%) |
3 (25.0%) |
6 (42.9%) |
0.44 |
0.9-0.1 |
|
Memory deficit |
5 (19.2%) |
5 (41.7%) |
0 (0.0%) |
3.2 |
0.1-0.05 |
|
Dizziness/ataxia |
4 (15.4%) |
2 (16.7%) |
2 (14.3%) |
0.25 |
0.9-0.1 |
|
Headaches |
4 (15.4%) |
3 (25.0%) |
1 (7.1%) |
0.25 |
0.9-0.1 |
|
Rash (without neuro symptoms) |
3 (11.5%) |
1 (8.3%) |
2 (14.3%) |
0.00 |
0.99 |
|
Hallucinations |
2 (7.69%) |
2 (16.7%) |
0 (0.0%) |
0.5 |
0.9-0.1 |
|
Otic |
2 (7.69%) |
1 (8.3%) |
1 (7.1%) |
0.5 |
0.9-0.1 |
|
Fevers |
1 (3.7%) |
1 (8.3%) |
0 (0.0%) |
0.00 |
0.99 |
|
Chancre |
1 (3.7%) |
1 (8.3%) |
0 (0.0%) |
0.00 |
0.99 |
*Diagnosis of neurosyphilis was based on a combination of clinical symptoms or LP results consistent with the neurosyphilis CDC criteria. Many of the patients had more than one symptom. The rapid progression group was defined as those who had a diagnosis of neurosyphilis within 6 months of their last RPR. The slow-progression group included patients who had their last RPR 7 months prior or more remotely.
The incidence of primary and secondary symptomatic syphilis was noted and compared with that in the area. The VA population had rates of 579 and 389, respectively, with an especially large increase in the overall syphilis cases in 2014. The incidence rates of primary and secondary syphilis in San Bernardino in 2014 and 2015 were 6.3 and 8.4 per 100,000 [1]. The rate of syphilis among male patients with VA HIV was much higher than that in the general population.
DISCUSSION
This study illustrates a successful decrease in symptomatic syphilis from 71.4% to 41.9% when evaluations were increased annually to every three months. Due to the low incidence of syphilis prior to 2004, the pre-intervention cohort was small (n=7) compared to the post-intervention group (n=148); therefore, group characteristics were not divided between the two groups because statistical significance could not be reached. However, there are many clinically relevant secondary findings. Early latent syphilis was the most common disease stage between 2009 and 2016. In 2014, there was a large increase in syphilis, especially late latent, which correlates with the national data [1] Compared to most HIV clinics, this VA clinic has more MSM, which has a strong positive correlation with syphilis risk [2-16]. One study showed a 300 times increased risk of syphilis among HIV-infected and MSM individuals compared to the general population [2]. This population has a higher average age (mean: 51.4) and a high rate of viral suppression (54% vs. 25%) [2]. Despite good HIV control, owing to the high incidence of syphilis among MSM, more frequent screening has a beneficial effect on the prevalence of symptomatic disease. Even with a screening intervals of six months, unfortunately, 12 patients still developed neurosyphilis. Further stratification of these patients revealed that those with rapid disease progression had significantly higher CD4 counts and RPR values. There was an increased prevalence of viral suppression and history of syphilis, but the effect size was not sufficiently large. Most studies suggest that a lower CD4 count and high viral load are risk factors for neurosyphilis [17-19]. However, one study showed that patients with CD4 counts > 350 were more likely to have had prior disease (43 vs. 15%) [18]. These differences could suggest that patients with prior syphilis and good HIV control have an increased susceptibility to neurosyphilis, possibly suggesting an immunologic phenomenon. Other possibilities include concurrent infections with multiple strains or a single, more virulent strain of syphilis. The molecular techniques needed to confirm this hypothesis are not currently available. The rapid progression of neurosyphilis suggests the need for increased screening. Ocular findings were present in 41% of patients with neurosyphilis, the majority of which were confirmed by ophthalmology. In the pre-ART era, ocular syphilis rates were around 9%, [20] but a recent CDC data showed a similar rate of 51% [21,22]. Two cases of ocular syphilis (18%) recurred despite receiving two weeks of intravenous penicillin, compared to the literature showing a 15% rate [23]. Most patients with ocular involvement only had a mild CSF protein elevation and only 71% of patients with neurosyphilis agreed to an LP, and were diagnosed based on symptoms or serum serology and treated appropriately. Therefore, CSF data were not included. Given the rapid progression of neurosyphilis and the large proportion of patients with ocular involvement within a six-month interval, there are compelling reasons to screen patients every three months.Another study limitation was the lack of direct data comparison between screening every three or six months. Future investigations should explore the etiology of rapidly progressive neurosyphilis and prevalence of ocular syphilis. This should be performed using a large cohort, 100% CSF sampling, and analysis of different spirochete strains.
CONCLUSION
Screening guidelines should be changed for high risk populations to more frequent intervals every three months. This study showed an increase in the detection of latent syphilis by increasing screening from yearly to every three months. Despite the overall good HIV control status, there is a high incidence of syphilis among HIV-infected MSM. Ocular syphilis rates and manifestations are similar to those reported in the literature, approximately 40-50%, which can cause significant lasting damage. Almost half of the patients with neurosyphilis adhere to at least every six month screening. Overall, those who progressed rapidly had better HIV control and were slightly more likely to have prior syphilis, suggesting a possible immunological phenomenon that warrants further study. These factors suggest that increased screening is needed to prevent associated morbidity during the recent syphilis epidemic.
Funding Statement: This study was not supported by any funding source.
Ethical Compliance: All procedures performed in the studies involving human participants were in accordance with the ethical standards of the Loma Linda Veterans Administration Hospital IRB board.
Conflict of Interest Declaration: The authors declare that they have no affiliations with or involvement in any organization or entity with any financial interest in the subject matter or materials discussed in this manuscript.
REFERENCES
- Patton ME, Su JR, Nelson R, Weinstock H; Centers for Disease Control and Prevention (CDC). Primary and secondary syphilis--United States, 2005-2013. MMWR Morb Mortal Wkly Rep. 2014; 63: 402-406.
- Workowski KA, Bachmann LH, Chan PA, Johnston CM, Muzny CA, Park I, et al. Sexually Transmitted Infections Treatment Guidelines, 2021. MMWR Recomm Rep. 2021; 70: 1-187.
- Branger J, van der Meer JT, van Ketel RJ, Jurriaans S, Prins JM. High incidence of asymptomatic syphilis in HIV-infected MSM justifies routine screening. Sex Transm Dis. 2009; 36: 84-85.
- Winston A, Hawkins D, Mandalia S, Boag F, Azadian B, Asboe D. Is increased surveillance for asymptomatic syphilis in an HIV outpatient department worthwhile? Sex Transm Infect. 2003; 79: 257-259.
- Cohen CE, Winston A, Asboe D, Boag F, Mandalia S, Azadian B, et al. Increasing detection of asymptomatic syphilis in HIV patients. Sex Transm Infect. 2005; 81: 217-219.
- Bissessor M, Fairley CK, Leslie D, Howley K, Chen MY. Frequent screening for syphilis as part of HIV monitoring increases the detection of early asymptomatic syphilis among HIV-positive homosexual men. J Acquir Immune Defic Syndr. 2010; 55: 211-216.
- Burchell AN, Allen VG, Gardner SL, Moravan V, Tan DH, Grewal R, et al; OHTN Cohort Study Team. High incidence of diagnosis with syphilis co-infection among men who have sex with men in an HIV cohort in Ontario, Canada. BMC Infect Dis. 2015; 15: 356.
- Kimberly A. Workowski, Laura H. Bachmann, Philip A. Chan, ChristineM. Johnston, Christina A. Muzny, Ina Park, et al. Centers for Disease Control and Prevention. Sexually Transmitted Diseases Treatment Guidelines, 2021. MMWR Recomm Rep. 2021; 70: 1-187.
- Tuite AR, Fisman DN, Mishra S. Screen more or screen more often? Using mathematical models to inform syphilis control strategies. BMC Public Health. 2013; 13: 606.
- Tuite A, Fisman D. Go big or go home: impact of screening coverage on syphilis infection dynamics. Sex Transm Infect. 2016; 92: 49-54.
- Zou H, Fairley CK, Guy R, Chen MY. The efficacy of clinic-based interventions aimed at increasing screening for bacterial sexually transmitted infections among men who have sex with men: a systematic review. Sex Transm Dis. 2012; 39: 382-387.
- Centers for Disease Control and Prevention
- Mir TA, Kim SJ, Fang W, Harvey J, Hinkle DM. Rising Incidence of Syphilitic Uveitis-Related Hospitalizations in the US. JAMA Ophthalmol. 2024; 142: 7-14.
- Petrosky E, Neblett Fanfair R, Toevs K, DeSilva M, Schafer S, Hedberg K, et al. Early Syphilis Among Men Who Have Sex with Men in the US Pacific Northwest, 2008-2013: Clinical Management and Implications for Prevention. AIDS Patient Care STDS. 2016; 30: 134-140.
- Solomon MM, Mayer KH, Glidden DV, Liu AY, McMahan VM, Guanira JV, et al; iPrEx Study Team. Syphilis predicts HIV incidence among men and transgender women who have sex with men in a preexposure prophylaxis trial. Clin Infect Dis. 2014; 59: 1020-1026.
- Chen YC, Liu HY, Li CY, Lee NY, Li CW, Ko WC, et al. The rising trend of sexually transmitted infections among HIV-infected persons: a population-based cohort study in Taiwan, 2000 through 2010. J Acquir Immune Defic Syndr. 2015; 68: 432-438.
- Marra CM, Maxwell CL, Smith SL, Lukehart SA, Rompalo AM, Eaton M, et al. Cerebrospinal fluid abnormalities in patients with syphilis: association with clinical and laboratory features. J Infect Dis. 2004; 189: 369-376.
- Wang YJ, Chi CY, Chou CH, Ho CM, Lin PC, Liao CH, et al. Syphilis and neurosyphilis in human immunodeficiency virus-infected patients: a retrospective study at a teaching hospital in Taiwan. J Microbiol Immunol Infect. 2012; 45: 337-342.
- Centers for Disease Control and Prevention (CDC). Symptomatic early neurosyphilis among HIV-positive men who have sex with men--four cities, United States, January 2002-June 2004. MMWR Morb Mortal Wkly Rep. 2007; 56: 625-628.
- Flood JM, Weinstock HS, Guroy ME, Bayne L, Simon RP, Bolan G. Neurosyphilis during the AIDS epidemic, San Francisco, 1985-1992. J Infect Dis. 1998; 177: 931-940.
- Centers for Disease Control and Prevention. Clinical advisory: ocular syphilis in the United States. 2016.
- Centers for Disease Control and Prevention (CDC). Symptomatic earlyneurosyphilis among HIV-positive men who have sex with men--four cities, United States, January 2002-June 2004. MMWR Morb Mortal Wkly Rep. 2007; 56: 625-628.
- Tsuboi M, Nishijima T, Yashiro S, Teruya K, Kikuchi Y, Katai N, et al. Prognosis of ocular syphilis in patients infected with HIV in the antiretroviral therapy era. Sex Transm Infect. 2016; 92: 605-610. es