Educational Intervention Program Improved the Torqued Testis Survival: A Quality-of-Care Study
- 1. Department of Urology, Hadassah Medical Center and Hebrew University, Israel
- 2. Braun School of Public Health and Community Medicine, Hadassah Medical Center and Hebrew University, Israel
Abstract
Introduction: The time from onset of symptoms to surgery is the most important factor determined testicular survival due to testicular torsion (TT). While the time between the onset of symptoms and arrival to the Emergency department (ED) is not depended on medical team, delay in time spent in the ED is preventable and should be minimized. In this study we examined the impact of an educational intervention program to reduce the length of time passing from patient admission to the ED to the start of de-torsion surgery.
Methods: An explanatory intervention, which included frontal lectures followed by knowledge test on TT was conducted for nursing and medical staff working in the ED. Door to detorsion time (DTD) defined as the duration of time from admission to ED, to onset of surgery. DTD was reviewed before and after the intervention. The correlation to testicular survival rate before and after the intervention were examined using a univariate and multivariate analysis.
Results: Data on 46 patients with TT were retrospectively reviewed in the pre-intervention period and 56 were prospectively reviewed the post- intervention period. Following educational intervention program time between ED arrival to OR was shortened from 169.76 minutes to 107.52 minutes (p=0.001) which reflects a relative time decrease of 58.89%. Orchiectomy rates were substantially lower from 12 patients (26.08%) to 10 patients (17.86%) though this was not statistically significant, (p=0.32). Multivariate regression showed intervention program lowered substantially ED delay with an average of64.9 minutes shortening when compared to pre-intervention period (p<0.001). Orchiectomy rates were substantially lowered following implementation of the intervention program with an odds ratio of 4.05. 95% CI [1.11,14.71].
Conclusions: Following a dedicated and ongoing educational intervention program the duration from patient entrance to the ED to surgery for detorsion shortened. Shortening this time frame is expected to significantly reduce the risk of orchiectomy.
Keywords
- Torqued testis
- Testicular torsion
- Torsion surgery
- Emergency department
Citation
Lorber A, Atias E, Levine H, Duvdevani M, Boyarsky L, et al. (2024) Educational Intervention Program Improved the Torqued Testis Survival: A Quality-of-Care Study. JSM Sexual Med 8(3): 1136.
ABBREVIATIONS
TT: Testicular Torsion; DTD: Door to Detorsion Time; ED: Emergency Department; TT: Torqued Testis
INTRODUCTION
Testicular torsion (TT) is a twisting of the spermatic cord and its contents, causing spermatic venous compression and testicular edema. This leads to arterial occlusion and eventually to testicular ischemia and necrosis [1]. TT affecting 4.5 cases per 100,000 male subjects per year. It accounts for 18-41% orchiectomy rate during scrotal exploration [2].
Testicular torsion is a leading cause of testicular loss and can result in fertility and endocrine impairment [3,4]. Abnormal sperm analysis was found after torsion in over 50% of patients, which correlated with the duration of torsion [5]. Some of these patients were declared infertile and were unable to conceive a child [6].
TT is an emergency requiring prompt diagnosis and treatment. Duration of symptoms is an important predictor of testicular damage, emphasizing the importance of immediate scrotal exploration, de-torsion and orchiopexy [7]. Early scrotal exploration, in patients presented with symptoms duration under 6 hours, can salvage most testes [8,9], When symptoms last longer, testes viability rates decline. Dunne et al., showed a 67% of orchiectomy performed when symptoms lasted more than 12 hours 10 and after 48 hours, no viable testes can be found [11].
In contrast to the great knowledge we have about the meaning of time passing from the onset of symptoms in patients with testicular torsion there wasn’t information in the literature on the duration of hospital management of patients suspected to have testicular torsion and the delays in their treatment. Previously [12], we offer a new term - “Door-To-Detorsion” (DTD) time – which is the time measured from the moment a patient suspected with testicular torsion enters the emergency room, to the time testicular de-torsion is done in the operating room. Testicular salvage rate after torsion depends on two main factors—quick seeking of medical attention and fast and efficient in-hospital management. We found DTD to be an important and independent factor affecting testicular survival, regardless of the prehospital delay.
While the time from initial symptoms presentation to arrival to medical care is difficult to control, late diagnosis and slow management in the hospital are factors that should be minimized by the medical staff. Since short DTD is crucial for testicular survival, the next necessary step should involve finding ways to shorten this interval.
In this study, in order to improve quality of care of patients suspected with testicular torsion, we developed an educational, interventional program among the nursing and medical staff working in the emergency department (ED) at Hadassah Medical Center in order to shorten DTD time. We aimed to assess the effectiveness of our intervention in shortening ED to Operation Room (OR) and to assess testis survival rate represented inversely by orchiectomy rate.
METHODS
This study is an analytic, interventional, prospective single center study.
We retrospectively collected surgical, clinical, and demographic Data on consecutive patients, referred to Emergency Department with testicular torsion during the years 2015-2017 (control group) and prospectively collected the same data on the post intervention education program (study group) during the years 2018-2020. All patients had clinically, and sonography approved testicular torsion and underwent surgical exploration. During surgery, the involved testicle de-torsed and placed in a warm cover. The contralateral testis was fixed to the dartos tissue, in cases of macroscopically appearance of testicular recovery, the involved testis was fixed in the same way. In case of surgeon impression of macroscopically irreversible necrotic testis that not recover after detorsion warming and waiting 15 minutes, orchiectomy was performed.
Data was extracted from electronic medical records, imaging software and surgery reports.
The following data was collected: (1) demographic data - age, (2) clinical data - duration of symptoms, affected testicle, ultrasound findings; (3) timing data - date of admission, date of operation, time of registration to emergency room at arrival, time of ultrasound examination, time of operation initiation; (4) outcomes - scrotal exploration findings (viable/ black testis) type of operation performed (orchiopexy/ orchiectomy) and post- operative ultrasound examination when available.
Intervals from time of emergency room registration to operation initiation (Door-To-Detorsion - DTD), from registration to ultrasound scrotal examination and from ultrasound to operation were calculated from extracted data. Since the decision to perform an orchiectomy is subjective, we analyzed the data twice with two endpoints. One is the type of operation performed (orchiectomy vs. orchiopexy) and the other is testis viability (necrotic testis vs. viable) as found during surgical exploration and documented by the surgeon in the surgical report. Calculated intervals, duration of symptoms and demographic data were compared between the groups.
We integrated educational intervention program from 2018 to 2020. The program included frontal lectures about testicular torsion, with the emphasis of the need of urgent and fast diagnosis and detorsion lectures followed by knowledge test. The participants included nurses and doctors the relevant department including Emergency Department, Radiology and Operation Room staff. Participants received knowledge questionnaires to verify implementation the main topics.
The intervention plan: When we approach behavior change, we have used the PDCA - Plan-Do-Check-Act cycle, a well-known and accepted method to achieve improvement in a given field [13].
The cycle of change includes observation – In our previous research [12] we examined for 10 years the management and treatment results in diagnosing testicular torsion and identified that time spent in the emergency room is an independent factor that affects testicular survival. With the help of questionnaires, we identified barriers that are mainly expressed in knowledge gaps and awareness among the staff treating in the emergency department, operating room staff and the staff in urology department.
In light of the principles of the PDCA method and the data obtained from the questionnaires, we performed an intervention in the form of frontal lectures for the treating staff, including emergency room staff, operating rooms and urology residences [14]. Next, we tested the same performance among the treating teams, following the intervention.
Statistical analysis- Statistical analysis was conducted using Statistical Product and Service Solutions (SPSS) v26.0 statistical software (SPSS Inc., Chicago, IL, USA). We produced descriptive statistics to generally describe relevant characteristics. We checked correlation between covariates, compared means using independent t-test. We used multivariate linear regression to assess intervention efficacy in shortening ED to OR interval. We predicted the binary covariate using multivariate logistic regression analysis. P-value < 0.05 was considered as a threshold for statistical significance. We used forced inclusion of all covariates rather stepwise model selection as been supported by several investigators and reviewed by Smith et al (Smith G, 1999) [15]. A p-value <0.05 was considered significant for every coefficient in the final model. Wald statistic was calculated for coefficient significance.
The Ethics and Research Committees of the organization approved the study. IRB – HMO-0015-17.
RESULTS
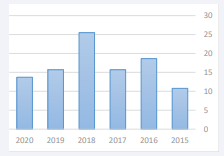
Overall, 102 patients had testicular torsion between 2015 and 2020 (Figure 1).
Figure 1: Torsion Incidence per year
Mean age was 15.73 years (SD 7.37). Mean symptoms duration was 32.53 hours (SD 50.40). 34.31% of the patients had symptoms for more than 24 hours. Mean Time from ED arrival to Operation Room was 135.59 minutes (SD 73.79). Orchiectomy rate was 21.57%.
|
Table 1: Univariate Analysis. |
|||
|
|
Pre- Intervention |
Post Intervention |
significance |
|
Age |
16.46 |
15.13 |
0.37 |
|
Orchiectomy rates |
26.09% |
17.86% |
0.319 |
|
ER to OR Interval (min) |
169.76 |
107.52 |
<0.0001 |
|
Duration of Symptoms (hr) |
25.02 |
38.7 |
0.156 |
|
Symptoms > 24 hrs |
0.35 |
0.34 |
0.929 |
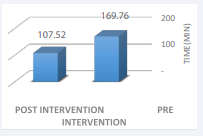
The intervention group included 56 and the control 46 patients. In a univariate analysis (Table 1), when comparing both groups, the time between ED arrival to OR was shortened from 169.76 minutes to 107.52 minutes (p=0.001) which reflects a relative time decrease of 58.89% (Figure 2).
Figure 2: ER to OR Interval (min)
Orchiectomy rates were substantially lower from 12 patients (26.08%) to 10 patients (17.86%) though this was not statistically significant (p=0.319).
We conducted multivariate analysis to assess the impact of our intervention program on time from Emergency Department to Operation Room. Our intervention lowered this delay in 64.99 minutes (p<0.001). The effect of other contributors as age and duration of symptoms are showed in Table 2.
|
Table 2: Multivariate Linear regression for ER to OR interval (min). |
||||||
|
|
Unstandardized Coefficients |
Standardized Coefficients |
Sig. |
95.0% Confidence Interval for B |
||
|
|
B |
Std. Error |
Beta |
Lower Bound |
Upper Bound |
|
|
Age |
-1.175 |
0.915 |
-0.117 |
0.202 |
-2.991 |
0.64 |
|
Pre vs. post intervention |
-64.996 |
13.528 |
0.44 |
0 |
-91.842 |
-38.149 |
|
Duration of Symptoms |
0.087 |
0.134 |
0.059 |
0.52 |
-0.18 |
0.354 |
We also conducted multivariate binary regression to assess orchiectomy rate predictors following our intervention. When controlling for potential confounders our intervention lowered orchiectomy rate significantly with an odds ratio of 4.058 comparing the pre-intervention period. The effect of other contributors as age and duration of symptoms are showed in Table 3.
|
Table 3: Multivariate Regression for Orchiectomy Rate. |
|||||
|
|
B |
Sig. |
Odd Ratio |
95% CI.for Odds ratio |
|
|
|
Lower |
Upper |
|||
|
Age |
-0.098 |
0.019 |
0.907 |
0.835 |
0.984 |
|
Pre vs. post intervention |
1.401 |
0.033 |
4.058 |
1.119 |
14.715 |
|
Duration of Symptoms |
0.02 |
0 |
1.02 |
1.009 |
1.031 |
|
ER to OR Interval |
-0.004 |
0.381 |
0.996 |
0.988 |
1.004 |
DISCUSSION
In this study we were able to demonstrate a substantial reduction of time from ED to testicular detorsion. The delay from ED arrival decreased from 169.76 to 107.52 minutes reflects a relative time decrease of 58.89%. Orchiectomy rates were substantially lowered following implementation of the intervention program with an odds ratio of 4.05.
Testicular torsion is a surgical emergency accounts for up to 15% of acute scrotal disease and must not be missed. A good working knowledge is required, and the treating staff must be well trained and full minded to prompt recognition and treatment [16]. Although the literature reported a six hours threshold for loss of testicular viability, some claim a longer time a phrase known as ‘testicular pain honeymoon [17,18]. Therefore, any delay in ED should be shortened. We recently published that the time to de-torsion was an independent factor predicting testicular survival12. The next necessary step to implant the conclusions of this study is to invest an effort to shorten DTD time interval. We implemented a comprehensive educational intervention program to address this issue, has been done successfully in other fields in the previous successful initiatives: door to balloon angioplasty [19], door to needle in acute ischemic stroke [20] door to electrocardiogram [21], time to pain management [22], among other.
Ramachandra et al. showed that the time to presentation is the most important factor in predicting testicular salvage, even if the time frame from ED arrival to operating room is longer17, this study shows that reducing ED delay would improve testicular survival rates. To the best of our knowledge, this is a unique and innovative study in this context, and no intervention studies have yet been published that have been able to show such a significant improvement in testicular survival rates.
Duration of symptoms is a well-known risk factor and played a pivotal role in testicular survival outcomes. Our results showed a significant reduction in time to detorsion and a substantial reduction in orchiectomy rate.
Our study, however, has some limitations. As clinically accepted testis survival and therefore orchiectomy rate is based on the discretion of the surgeon. Possibly, and some of the fixed testis rather than excised, are not really functional. For this purpose, performing a follow-up ultrasound examination was appropriate, but it is beyond of the scope of this study. Another issue is the relatively low number of cases in the both groups. Since TT is not a common phenomenon, this initiative study could prepare the ground for further larger, well design intervention study that will eliminate this shortage. Hawthorne effect, meaning, a change of individual behavior when being observed, could play a role in any intervention program. We had approximately 26 months monitoring of the intervention effect and this might overcome this effect. Finally, the confounding effect that might be attributed to duration of symptoms. As much as this is true, we believe this did not invalidate the impact of intervention program but rather influence the significance. Our results support that ED and Urology team should do their best to operate TT as soon as possible, regardless of symptoms durations, resulting in better testicular survival rates. The importance of lowering the delay from ED entrance to surgical exploration and detorsion could not be overemphasize and should be considering in every testicular- torsion-suspected patient.
We suggest that in a given symptoms duration, shortening ED delay will improve testicular survival rates. The importance of lowering the delay from ED entrance to surgical exploration and detorsion could not be overemphasize and should be taking into account in every testicular-torsion-suspected patient.
CONCLUSION
Implementing intervention educational program to providers and nursing stuff manage patients with testicular torsion reduce door to detorsion time, and may improve testicular survival rate.
Our impression is that such a program can also be implemented in other hospitals in Israel. In order to implement it successfully there is a need for inter-departmental cooperation and commitment of emergency room, urologist and operating rooms teams.
REFERENCES
- Kapoor S.Testicular torsion: a race against time. Int J Clin Pract. 2008; 62: 821-827.
- Mansbach JM, Forbes P, Peters C. Testicular torsion and risk factors for orchiectomy. Arch Pediatr Adolesc Med. 2005; 159: 1167–71
- Thomas WE, Cooper MJ, Crane GA, Lee G, Williamson RC. Testicular exocrine malfunction after torsion. Lancet. 1984; 2: 1357-1360.
- Carmelo Romeo, Pietro Impellizzeri, Teresa Arrigo, Pietro Antonuccio, Mariella Valenzise, Silvio Mirabelli, et al. Late hormonal function after testicular torsion. J Pediatr Surg.2010; 45: 411-413.
- Mark J. Anderson, J. Kay Dunn, Larry I. Lipshultz.Semen Quality and Endocrine Parameters after Acute Testicular Torsion. J Urol. 1992; 147: 1545-1550.
- Ilan Gielchinsky, Efrat Suraqui,Guy Hidas, Mohammad Zuaiter, Ezekial H Landau, Alexander Simon,et al. Pregnancy rates after testicular torsion. J Urol. 2016; 196: 852–855.
- Cuckow PM, Frank JD. Torsion of the testis. BJU Int. 2001; 86: 349–353.
- Anderson JB, Williamson RC.Testicular torsion in Bristol: a 25-year review.Br J Surg.1988; 75: 988–992.
- Ringdahl E, Teague L.Testicular torsion. Am Fam Physician. 2006; 74: 1739–1743.
- Dunne PJ, O’Loughlin BS. Testicular torsion: time is the enemy.Aust N Z J Surg. 2000; 70: 441-442.
- Lewis AG, Bukowski TP, Jarvis PD, Wacksman J, Sheldon CA. Evaluation of acute scrotum in the emergency department. J Pediatr Surg. 1995; 30: 277-281; discussion 281-272.
- Daniel D Gold 1, Amitay Lorber, Hagai Levine, Shilo Rosenberg, Mordechai Duvdevani, Ezekiel H Landau, et el.Door To Detorsion Time Determines Testicular Survival. Urology.2019; 133: 211-215.
- Lauren Destino MD, Denise Bennett MBA,RN,RM, Matthew Wood PhD, Christy Acuna MD, Stephanie Goodman, Asch SM, et al, Improving Patient Flow: Analysis of an Initiative to Improve Early Discharge. J Hosp Med. 2019; 1: 22-27
- J L M Lieow, FSM Chen, G Song, PS Tang, Y Kowitlawakul, A Mukhopadhyay.Effectiveness of an advanced practice nurse-led delirium education and training programme. International Nursing Review. 2019; 66: 506-513.
- Allison, Paul David. Multiple regression: a primer. Pine Forge Press, Thousand Oaks, Calif. London. 1999.
- Sharp VJ, Kieran K, Arlen AM.Testicular torsion: diagnosis, evaluation, and management.2013; 15; 88: 835-40.
- Ramachandra P, Palazzi KL, Holmes NM. Factors influencing rate of testicular salvage in acute testicular torsion at a tertiary pediatric center. West J Emerg Med. 2015; 16: 190-194.
- Mellick L, Sinex J. Testicular Torsion Pain Honeymoons. Pediatr Emerg Care. 2019; 35: 241-244.
- Laurent Faroux, Thibault Lhermusier, Flavien Vincent, Luis Nombela- Franco, Didier Tchétché, Marco Barbanti, et al. Effect of door-to- balloon time on mortality in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2006; 47: 2180-2186.
- Gregg C Fonarow, Eric E Smith, Jeffrey L Saver, Mathew J Reeves, Adrian F Hernandez, Eric D Peterson, et al. Improving door-to-needle times in acute ischemic stroke: the design and rationale for the American Heart Association/American Stroke Association’s Target: Stroke initiative. 2011; 42: 2983-2989.
- Michael P Phelan, Jon Glauser, Elizabeth Smith, Craig Martin, Stefanie Schrump, Pat Mahone, et al. Improving emergency department door-to-electrocardiogram time in ST segment elevation myocardial infarction. Crit Pathw Cardiol. 2009; 8: 119-121.
- Sarah SS, Rebecca BR, Lindsay HS, Camden Harrell, Tamekia LJ, Barbara MS, et al. Reducing time to pain medication administration for pediatric patients with long bone fractures in the emergency department. Pediatr Qual Saf. 2018; 3: 120.