Penile Cancer in Kamenge Univesrity Hospital Center at Bujumbura: A Literature Review for Five Cases
- 1. Kamenge University Hospital Center - Bujumbura, BURUNDI/ Visceral Surgery and Urology, Republic of Congo
- 2. University Clinic of Urology and Andrology, National Hospital and University Center Hubert Koutoukou Maga (CNHU HKM), Cotonou, Benin
Abstract
Background: Penile cancer is the rarest among genitourinary cancers. Data on the extent (incidence and prevalence) and mortality of this cancer are either unavailable or scarce in most African countries, including Burundi.
The objective is to study the epidemiology, signs, diagnosis, and treatment of penile cancer in Bujumbura.
Methods: Prospective study over a period of ten months, collecting data from patients treated for penile cancer in certain hospitals in Bujumbura.
Results: Over ten months, 5 cases of penile cancer were recorded. The majority of patients come from rural social strata (n=4). The average age of patients is 63 years. The average consultation delay was 2.6 years. Lack of circumcision and poor hygiene are implicated as risk factors. Glandular localization is the most common (n=3). Squamous cell carcinoma is the dominant histological type (n=4). Partial penile amputation is the main treatment (n=3) with postoperative chemotherapy (n=2).
Conclusion: Penile cancer is rare but exists in Burundi. Emphasis should be placed on early circumcision and intimate hygiene. Several challenges related to psychological behavior and difficult economic circumstances constitute a major obstacle to the proper management of this pathology.
Keywords
• Penile cancer
• Squamous cell carcinoma
• Circumcision
CITATION
Ndayirorere R, Ngabire NE, Valimungighe MM, Bagaya L, Mossini J, et al. (2023) Penile Cancer in Kamenge Univesrity Hospital Center at Bujumbura: A Literature Review for Five Cases. JSM Sexual Med 7(4): 1124.
INTRODUCTION
Penile cancer is the rarest among genitourinary cancers, constituting only 0.5% of malignant tumors in men [1,2]. Several additional risk factors for penile cancer are implicated, including infection with the human did not reveal any particularities.
Neoadjuvant chemotherapy was initiated with fluorouracil papillomavirus (HPV), phimosis, lack of circumcision, poor hygiene, smoking, urogenital infections, and more.
In Burundi, the population may be exposed to all these aforementioned factors to some extent. However, data on the extent (incidence and prevalence) and mortality of this cancer are scarce due to the absence of a cancer registry in most African countries, including Burundi.
Therefore, this study aims to serve as a precursor with the goal of investigating the epidemiological, clinical, diagnostic, and therapeutic aspects of penile cancer cases treated in hospitals in Bujumbura.
PATIENTS AND METHODS
This is a prospective study of 5 cases of penile cancer treated in certain hospitals in Bujumbura, including 3 cases at the University Hospital of Kamenge, 1 case at Tanganyika Hospital, and 1 case at the Medical and Surgical Center of Kinindo over a period of 10 months (January 2023 to October 2023). Epidemiological, clinical, and therapeutic aspects were investigated.
For each patient, the following parameters were assessed: age at the time of diagnosis, origin, the interval between the onset of lesions and the first consultation, risk factors or precancerous lesions, localization, lesion size, tumor histology, and the type of treatment.
CLINICS OBSERVATIONS
Case 1
A 67-year-old patient with no significant medical history presented with pain and deformation of the penis along with dysuria. The patient also reported chronic cough over a three-year period.
Physical examination revealed a compromised general condition, a non-circumcised penis, deformation with a leftward deviation, and a small nodular mass (2cm) located at the sulcus. The corpus cavernosum was firm, especially on the right, with palpable bilateral inguinal adenopathies.
A biopsy performed after excision of a penile nodule confirmed abasaloid squamous cell carcinoma.
Extension assessment:
-
- Abdominopelvic ultrasound: Multiple hepatic nodules
- Chest X-ray: Balloon drop-like images
A metastatic penile tumor classified as T4N2M1 was diagnosed.
The patient received palliative treatment with analgesics and oxygen therapy.
Palliative chemotherapy was recommended, but the patient succumbed to respiratory distress.
Case 2
A 66-year-old patient with no significant medical history presented with a painless lesion on the penis evolving for almost a year, accompanied by progressively developing dysuria. Clinical examination revealed a bleeding, budding lesion on the gland measuring 4cm on a non-circumcised penis.
No palpable inguinal adenopathies were observed. Due to a lack of resources, the patient did not undergo diagnostic or staging tests. Partial penectomy was performed.
Biopsy on the operative specimen revealed a well-differentiated, mature, infiltrating squamous cell carcinoma developed on a scleroatrophic lichen. Presence of vascular emboli. Complete excision was achieved. The lesion was classified as T1aNoMx. Abdominopelvic ultrasound and chest X-ray conducted as part of pre- therapeutic assessments and cisplatin.
Case 3
A 69-year-old patient with no significant medical history presented with an ulcerating and budding lesion located on the foreskin, measuring 3cm, on a non-circumcised penis, evolving for nearly 3 years. The patient reported condylomatous lesions in the past, urinary disturbances such as burning sensation during urination, dysuria, and excruciating penile pain.
Physical examination revealed multiple mobile inguinal lymph nodes, with soft corpus cavernosum. No diagnostic or staging tests were conducted before treatment due to financial constraints. Surgery was indicated, and partial penectomy with complete excision was performed. Anatomopathological examination of the operative specimen concluded a moderately differentiated squamous cell carcinoma.
A TAP (thoraco-abdominopelvic) scan conducted as part of pre-therapeutic assessments noted suspicious inguinal adenopathies without other anomalies. The tumor was classified as T1aN2M0.
Palliative chemotherapy with carboplatin and paclitaxel was initiated at a frequency of one cycle every three weeks.
Case 4
A 41-year-old immunocompromised patient with known HIV, under treatment for 10 years, presented with an ulcerating and budding lesion on the glans of the circumcised penis, evolving for about two years, accompanied by dysuria.
Physical examination revealed a circumferential glandular lesion, obscuring the urethral meatus, extending beyond the balanopreputial sulcus, measuring 5cm. The corpus cavernosum and spongiosum were soft, with no palpable inguinal adenopathies.
Biopsy of the lesion confirmed a well-differentiated non- invasive squamous cell carcinoma. A TAP scan conducted as a staging assessment did not show secondary locations. The lesion was classified as T1AN0M0.
Partial penectomy with complete excision of the lesion was performed. No neoadjuvant chemotherapy was instituted, and oncologists adopted strict surveillance.
Case 5
A 72-year-old patient with no significant medical history presented with acute urinary retention and a budding vegetation on the glans, evolving for 4 years, in a non-circumcised individual living in precarious conditions.
Clinical examination was conducted on an agitated patient with an altered general condition. The patient exhibited a distended bladder, and the budding lesion extended to the base of the penis (7cm). Palpable mobile bilateral inguinal adenopathies were noted.
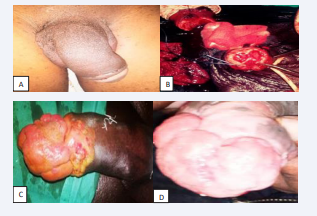
A suprapubic catheter was inserted to relieve urinary retention. Biopsy of the lesion concluded a Kaposi’s sarcoma. The lesion was classified as T3NxMx. Despite medical advice, the patient requested discharge without undergoing staging tests or treatment for extension (Figure 1).
Figure 1: A. Deformed penis after removal of the nodule in the first case B. Perioperative time for partial penectomy in the fourth case C. And D. Appearance of ulcerative –nodular lesions on the glan
Patients’ characteristics have been detailed in Table 1.
Table 1: Key characteristics of the patients.
|
Patient |
Age (years) |
Consultation Delay (years) |
Size (cm) |
Histological Type |
R F |
TNM |
TTT |
|
1 |
67 |
3 |
2 |
SCC |
NCP |
T4N2M1 |
CT |
|
2 |
66 |
1 |
4 |
SCC |
- |
T1aNoMx |
PP |
|
3 |
69 |
3 |
3 |
SCC |
Condylomas NCP |
T1aN2M0 |
PP+CT |
|
4 |
41 |
2 |
5 |
SCC |
HIV |
T1ANoMo |
PP |
|
5 |
72 |
4 |
7 |
Sarcoma |
NCP |
T3NxMx |
|
RF: Risk Factors, TTT: Treatment, SCC: Squamous Cell Carcinoma, NCP: Non-circumcised Penis, CT: Chemotherapy, PP: Partial Penectomy
DISCUSSION AND LITERATURE REVIEW
Penile cancer is a rare tumor, with generally low incidence, but geographical variations exist. In America and Europe, the incidence is typically less than 1 per 100,000 men [3,4]. Conversely, the frequency is higher in Africa, Asia, and South America, reaching up to 10% of cancers in certain regions [5]. Cultural differences also play a significant role, as regions practicing neonatal circumcision tend to have a lower incidence [6].
This significant variation in penile cancer incidence suggests a connection to underdevelopment [7]. This hypothesis is supported by the fact that four of our patients come from impoverished rural communitie.
To date, no study has been conducted to assess the extent of penile cancer in Burundi. The socio-cultural context, considering genitourinary pathologies in men as taboo, may be the root cause of underdiagnosis and therapeutic difficulties.
Nevertheless, studies from the East African region, to which Burundi belongs, highlight the magnitude of the disease. For example, Ngendahayo et al., in Rwanda [8], Wabinga et al., in Uganda [9], Magoha et al., in Kenya [10], and Chalya et al., in Tanzania [11] found respective incidences of penile cancer as 0.3 per 100,000; 4.4%; 0.1% and 2.2%.
These studies underscore the importance of regional awareness and epidemiological research to understand the prevalence and unique challenges associated with penile cancer in specific areas. Collaborative efforts between healthcare providers, public health agencies, and communities can contribute to breaking down cultural barriers, improving early detection, and enhancing therapeutic outcomes for individuals affected by penile cancer in the Burundian context.
The average age of onset for penile cancer is reported to be around 50 years [12]. The average age of diagnosis in our patients is 63 years (ranging from 41 to 72 years). Our results align with those of studies by Houyem et al. in Tunisia and Yacoubi et al. in Morocco, reporting average ages of 64.27 years and 60.5 years, respectively [13,14].
Demographic data indicates that penile cancer rates tend to increase with age.
The higher average age at diagnosis in our study and in other research from the region may reflect late-stage presentations, delayed healthcare seeking, or specific age-related risk factors. Understanding these age patterns is crucial for tailoring awareness campaigns and screening programs to effectively target at-risk populations and improve early detection in older age groups.
We believe that penile cancer occurs much earlier in Burundi, but patients seek medical attention late due to, on the one hand, the taboos surrounding genital conditions, and on the other hand, the negligence of patients who do not worry about suspicious lesions on the penis [15]. The average consultation delay was 2.6 years.
Additional risk factors for penile cancer include HPV infection. The presence of phimosis, lack of circumcision with a history of phimosis, exposure to tobacco, poor hygiene, and obesity are associated with an increased risk.
Medical conditions of the penis such as genital warts, penile trauma, urogenital infections, and strictures are also linked to an elevated risk [16,17].
We had four cases who were not circumcised and came from unfavorable socio-economic conditions. Neonatal circumcision is not even routine in our country. The absence of circumcision and poor hygiene were thus implicated as risk factors in our series.
The association between the absence of circumcision and penile cancer has been established in several studies. However, this notion has gradually been set aside, with phimosis being considered the primary risk factor for invasive penile cancer due to the accumulation of smegma causing repeated chronic inflammation and subsequent carcinogenesis. It is inferred that circumcision eliminates the risk of phimosis, which could otherwise lead to penile cancer [18].
The tumor typically presents as an ulcerative and nodular growth, easily bleeding upon contact. In our series, only one case manifested as a penile nodule. It usually originates in the glans, sometimes on the epithelial surface of the prepuce or in the balanopreputial sulcus. We had three cases involving the glans, one case in the prepuce, and one case in the sulcus.
The most common histological form is squamous cell carcinoma.
Basal cell carcinomas are rarer [19-21].
Sarcomas and leiomyosarcomas are exceptional, with only one case observed in our series.
The local extension is slow and progresses towards the corpora cavernosa, scrotum, or even the pubis. Remaining limited for a long time, it rarely concerns patients in our regions, and they seek consultation when the lesions are exaggerated, even mutilating, with lymph node or distant metastases. Some patients consult due to societal pressure bothered by the foul odor emanating from the lesions. Regional extension occurs through the lymphatic system.
Metastasis through the bloodstream is rare [21]. According to Johnson [20], it occurs in less than 10% of cases. We suspected a case of distant metastasis; pulmonary and hepatic, in our series.
The assessment of local and regional extension in our series relies on clinical examination, ultrasound, and TAP (thoracic, abdominal, and pelvic) CT scan. The extension assessment is not easily achievable in Burundi due to limitations in availability and financial means of our patients, which poses a major obstacle to the diagnosis and management of cancer in general.
The treatment depends on the stage, size, and location of the tumor. Therapeutic options include surgery, radiotherapy, chemotherapy, and new therapies. Surgical resection is an important part of penile cancer treatment.
For locally confined disease, conservative treatments such as cryotherapy, laser therapy, and the microsurgical Mohs method can be used.
In cases of metastatic disease, partial or total penectomy is necessary, along with iliac lymph node dissection for high-risk tumors. Radiotherapy offers the advantage of ensuring lasting local control while preserving functional anatomy. However, this therapy is not without its toxicities, including skin toxicity, soft tissue ulceration, meatal stenosis, and, more rarely, urethral and penile fistulas, necrosis, and edema.
Any slow healing of ulcers resulting from radiotherapy should be biopsied to rule out tumor recurrence. Circumcision is performed routinely before radiotherapy. Chemotherapy is used for metastatic tumors in conjunction with surgery for patients with locoregional involvement, either in a neoadjuvant or in postoperative setting [22]. Chemotherapy regimens typically involve combinations of 2 or 3 drugs due to the relative resistance of penile cancer to chemotherapy, with cisplatin being a common component. Neoadjuvant chemotherapy followed by surgery is recommended for patients with unresectable inguinal lymph nodes [22].
In our series, three patients underwent partial penectomy, and two of them received postoperative chemotherapy. Neoadjuvant chemotherapy was indicated for a patient who unfortunately passed away during the treatment. One of our patients declined any treatment before escaping.
Non-adherence of patients to radical cancer treatment due to socio-cultural considerations and mysterious beliefs, limited financial means of patients, and the inadequacy of well-developed oncology centers are the main problems encountered in the management of cancer in general, and penile cancer in particular.
CONCLUSION
Penile cancer exists in Burundi. Its rarity explains the absence of comprehensive studies to guide well-defined diagnosis and treatment. Various risk factors have been discussed, and emphasis should be placed on the protective effects of early circumcision and intimate hygiene.
Delay in seeking medical consultation, limited financial means, and the inadequacy of centers for the diagnosis and treatment of cancers pose a major challenge in managing this disease.
REFERENCES
- Mottet N, Avances C, Bastide C, Culine S, Ibora F, Kouri G, et al. Penile tumors. Prog Urol. 2004; 14: 903-11.
- Mottet N. Epidemiology of Penile Cancer. Prog Urol. 2003; 13: 1237.
- Chaux A, Netto GJ, Rodríguez IM, Barreto JE, Oertell J, Ocampos S, et al. Epidemiologic profile, sexual history, pathologic features, and human papillomavirus status of 103 patients with penile carcinoma. World J Urol. 2013; 31: 861–867.
- Backes DM, Kurman RJ, Pimenta JM, Smith JS. Systematic review of human papillomavirus prevalence in invasive penile cancer. Cancer Causes Control. 2009; 20: 449-457.
- Hakenberg OW, Compérat E, Minhas S, Necchi A, Protzel C, Watkin N. EAU guidelines on penile cancer. Eur Urol. 2015; 67: 142-150.
- Thomas A, Necchi A, Muneer A, Tobias-Machado M, Tran ATH, Van Rompuy AS, et al. Penile cancer. Nat Rev Dis Primers. 2021; 7: 11.
- SOLIS WA. Cancer de la verge. Notre expérience. Ann Urol. 1985; 19: 338-344.
- Ngendahayo E, Nzayirambaho M, Bonane A, Gasana GA, Ssebuufu R, Umurangwa F, et al. Pattern and clinical management of penile cancer in Rwanda. Afr J Urol. 2018; 24: 274–81.
- Wabinga HR, Parkin DM, Wabwire-Mangen F, Nambooze S. Trends in cancer incidence in Kyadondo County, Uganda, 1960–1997. Br J Cancer. 2000; 82: 1585-92.
- Magoha GA, Ngumi ZW. Cancer of the penis at Kenyatta National Hospital. East Afr Med J. 2000; 77: 526–30.
- Chalya PL, Rambau PF, Masalu N, Simbila S. Ten-year surgical experiences with penile cancer at a tertiary care hospital in northwestern Tanzania: a retrospective study of 236 patients. World J Surg Oncol. 2015; 13 :71.
- Mottet N et al. Cancer of the penis: Association Francaise d’Urologie, Cancer Committee guidelines. Prog Urol. 2008; 18: 685-6.
- Mansouri H, Safta, Ayadi MA, Selma G, Tarek BD, Rahal K. Cancers primitifs de la verge: à propos de 11 cas et revue de la littérature. Pan Afr Med J. 2018; 31: 14.
- Nouri A, Elkarni H, El Yacoubi S, Karmouni T, El Kahder K, Koutani A, et al. Cancer du pénis: À propos de 6 cas à l’hôpital universitaire de Rabat et revue de la littérature. African Journal of Urology 2012; 18: 66-70.
- Chadha J, Chahoud J, Spiess PE. An update on treatment of penile cancer. Ther Adv Med Oncol. 2022; 14: 1-17.
- Daling JR, Madeleine MM, Johnson LG, Schwartz SM, Shera KA, Wurscher MA, et al. Penile cancer: importance of circumcision, human papillomavirus and smoking in in situ and invasive disease. Int J Cancer. 2005; 116: 606–616.
- Barnes KT, McDowell BD, Button A, Smith BJ, Lynch CF, Gupta A. Obesity is associated with increased risk of invasive penile cancer. BMC Urol. 2016; 16:42.
- Larke NL, Thomas SL, dos Santos SI, Weiss HA. Male circumcision and penile cancer: a systematic review and meta-analysis. Cancer Causes Control. 2011; 22: 1097–110.
- Dargent M, Colon J, Delore X. Cancer de la verge. Ann Chir. 1963; 17:509-532.
- Johnson DE, Swanson DA, Von Eschenback AC. Tumeurs de la verge. In Smith urologie. Ed. Piccin 1991: 428-431.
- Solis WA. Cancer de la verge. Notre expérience. Ann Urol. 1985; 19: 338-344.
- Van Poppel H, Watkin NA, Osanto S, Moonen L, Horwich A, Kataja V, et al. Penile cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013; 24:115-124.