The Effects of Vaginal Laser Therapy on Sexual Quality of Life in Patients with Genitourinary Syndrome of Menopause (GSM)
- 1. Department of Obstetrics and Gynecology, Ren-Ai Branch, Taipei, Taiwan
Abstract
Background: Genitourinary syndrome of menopause (GSM) is a chronic and progressive syndrome that markedly impairs sexual quality of life in postmenopausal women. While vaginal laser therapy has emerged internationally as a promising non-hormonal treatment, data from Asian populations remain limited.
Aim: To evaluate the effects of fractional CO2 vaginal laser therapy on sexual quality of life in Taiwanese women with GSM, with subgroup analysis by recent hormone replacement therapy (HRT) exposure.
Methods: This retrospective single-center study included 27 postmenopausal women treated at a secondary teaching hospital in Taiwan from August 2022 to September 2024. All underwent three sessions of SmartXide² CO2 vaginal laser therapy. Sexual quality of life was assessed with the Pelvic Organ Prolapse/ Urinary Incontinence Sexual Questionnaire short form (PISQ-12, item 5-8) and a Sexual Satisfaction Visual Analog Scale (VAS) at baseline, 3, 6, and 12 months.
Outcomes: The primary outcome was improvement in PISQ-12 short form scores and Sexual Satisfaction VAS score across the study period, with subgroup analysis by HRT status.
Results: The mean PISQ-12 short form score improved from 9.9 ± 4.7 to 12.7 ± 3.5 (p = 0.004). Significant improvement was observed in the non-HRT group (p = 0.008), but not in the HRT group (p = 0.154). In longitudinal analysis, the non-HRT group demonstrated sustained increases in Sexual Satisfaction VAS score up to 12 months (all p < 0.01 vs baseline), whereas the HRT group showed only transient, non-significant changes.
Clinical Implications: Fractional CO2 vaginal laser therapy may serve as a valuable non-hormonal option for GSM, particularly for women who are not candidates for or do not respond well to HRT.
Strengths & Limitations: This study used a standardized laser protocol in an Asian cohort, enhancing validity and local relevance, but its retrospective single-center design, small sample size, self-reported measures, and short follow-up limit generalizability.
Conclusions: Fractional CO2 vaginal laser therapy improved sexual quality of life in postmenopausal women with GSM, with sustained benefits most evident in those without recent HRT exposure. It may represent a valuable alternative for patients who are not candidates for or do not respond to hormone therapy.
Keywords
• ISexual Function; Genitourinary Syndrome of Menopause (GSM); Laser Therapy; Quality of Life; Vaginal Atrophy; Hormone Replacement Therapy (HRT); Menopause
Citation
Ho PH, Lin TY (2025) The Effects of Vaginal Laser Therapy on Sexual Quality of Life in Patients with Genitourinary Syndrome of Menopause (GSM). JSM Sexual Med 9(4): 1166.
ABBREVIATIONS
GSM: Genitourinary Syndrome of Menopause; HRT: Hormone Replacement Therapy; PISQ-12: Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire-12; VAS: Visual Analog Scale; BMI: Body Mass Index
INTRODUCTION
The genitourinary syndrome of menopause (GSM) is a relatively new term that replaces previous terminology such as vulvovaginal atrophy, atrophic vaginitis, and urogenital atrophy [1]. GSM is a chronic and progressive condition affecting the vulvovaginal area, sexual function, and lower urinary tract, primarily resulting from estrogen deficiency. Approximately 40–54% of postmenopausal women and 15% of premenopausal women are affected by GSM, yet only a small proportion seek medical consultation [2].
Common symptoms include vaginal dryness, irritation, burning, dyspareunia, recurrent urinary tract infections, and urinary incontinence [3]. Studies have shown that these symptoms significantly impact women’s ability to achieve sexual enjoyment (75%), their relationship with their partner (67%), and their sexual spontaneity (66%) [4]. These symptoms can greatly affect the quality of life (QOL) of women, especially those who are sexually active (3). Nonhormonal therapies, such as lubricants and moisturizers, are recommended as first-line treatments to relieve symptoms, while the gold standard is represented by topical estrogen therapy [5].
Recent studies have shown that fractionated CO? vaginal laser therapy provides improvements in GSM symptoms, sexual function, and overall patient satisfaction that are comparable to those achieved with vaginal estrogen treatment [6]. The vaginal laser works through activation of regenerative mechanisms in the connective tissue—stimulating the formation of new blood vessels, dermal papillae, and collagen—and in the epithelium, resulting in thickening and desquamation of epithelial cells [7]. These changes lead to remodeling of the vaginal tissue and improved lubrication, which ultimately contribute to symptom relief in GSM [6].
However, local data on the use of vaginal laser therapy for GSM in Taiwan remain limited, and few studies have specifically explored its effect on sexual quality of life in this population. Therefore, this study is based on the initial results from Taipei City Hospital and aims to evaluate the effects of vaginal laser therapy on sexual quality of life in patients with GSM.
MATERIALS AND METHODS
Study design
This retrospective single-center study was conducted at a secondary teaching hospital in Taiwan. The study aimed to evaluate improvements in sexual quality of life among postmenopausal women suffering from GSM following vaginal laser therapy. Patients were selected between August 2022 and September 2024.
Inclusion criteria included postmenopausal women who had completed at least three sessions of vaginal laser therapy and had fully completed the associated questionnaires during treatment.
Exclusion criteria included the absence of sexual activity within the past year, incomplete treatment with fewer than three vaginal laser sessions, missing questionnaire or demographic data, and premenopausal status at the time of treatment.
Procedure
Patients who met the inclusion criteria underwent vaginal laser therapy at Taipei City Hospital, Renai Branch. The treatment was performed using the SmartXide² CO? laser system and incorporated three different types of laser probes during each session: a 360-degree probe, a 90-degree single-mirror probe, and a straight vulvar probe. For the 360-degree probe, the energy settings were 30 W of power, with a 1000 microseconds pulse duration, 1000 micrometers spacing, a pulse stack of 2, and the D-Pulse mode. The 90-degree single-mirror probe utilized the same energy parameters but was applied three times, specifically targeting the anterior vaginal wall at the 11, 12, and 1 o’clock positions. The straight vulvar probe was set to deliver 4.0 W of power, with an 800 microsecond pulse duration, 1000 micrometer spacing, a pulse stack of 1, and the D-Pulse mode. Each patient received a total of three treatment sessions, spaced one month apart. All procedures were conducted in an outpatient setting, without the use of anesthesia or analgesic medication.
Assessment
Sexual quality of life was assessed before and after the third session of vaginal laser therapy using the Short Form of Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12), specifically items 5 through 8 (Table 1).
Table 1: PISQ-12 short form items.
|
|
Always |
Usually |
Sometimes |
Seldom |
Never |
|
Do you feel pain during sexual intercourse? |
4 |
3 |
2 |
1 |
0 |
|
Are you incontinent (leak urine) with sexual activity? |
4 |
3 |
2 |
1 |
0 |
|
Does fear of incontinence (either stool or urine) restrict your sexual activity? |
4 |
3 |
2 |
1 |
0 |
|
Do you avoid sexual intercourse because of bulging in the vagina (either bladder, rectum or vagina falling out)? |
4 |
3 |
2 |
1 |
0 |
PISQ-12 short form (items 5–8) used for sexual quality of life assessment in patients with GSM.
These four questions were selected because they are more directly related to GSM, whereas other items in the questionnaire (e.g., “Does your partner have a problem with erections that affects your sexual activity?” or “Does your partner have a problem with premature ejaculation that affects your sexual activity?”) were considered less relevant to the scope of this study and thus excluded. Additionally, patients were followed up through telephone interviews conducted one year after the initiation of treatment. During these interviews, participants were asked to subjectively assess their sexual quality of life by considering multiple factors, including vaginal dryness, dyspareunia, and recurrent infections. A self-reported 10-point scale, referred to as the Sexual Satisfaction VAS Score, was used to quantify their experiences, with 0 indicating the lowest level of satisfaction and 10 indicating the highest (Figure 1).
Figure 1 Sexual Satisfaction VAS score used for subjective assessment of sexual quality of life, ranging from 0 (lowest satisfaction) to 10 (highest satisfaction).
Patients were asked to rate their sexual quality of life at four specific time points: prior to treatment, three months after the initiation of treatment (i.e., upon completion of all three vaginal laser sessions), six months after treatment initiation, and one year after treatment initiation.
Statistical analysis
Statistical analyses were performed using SPSS Statistics for Windows, Version 22.0 (IBM Corp., Armonk, NY, USA). Continuous variables were summarized as mean and standard deviation (SD). Descriptive statistics were used to present baseline demographic and clinical characteristics. Independent-samples t-tests were applied to compare baseline variables between patients who had and had not received hormone replacement therapy (HRT) in the past year. Paired-samples t-tests were used to assess changes in sexual quality of life, as measured by the PISQ-12 short form, before and after vaginal laser therapy. Longitudinal changes in Sexual Satisfaction VAS scores across four time points—prior to treatment, three months after initiation of treatment (i.e., upon completion of three vaginal laser sessions), six months after initiation, and one year after initiation—were evaluated using repeated-measures analysis of variance (ANOVA). Where appropriate, post hoc pairwise comparisons with Bonferroni adjustment were conducted to identify significant differences between time points. A p-value of <0.05 was considered statistically significant.
RESULTS
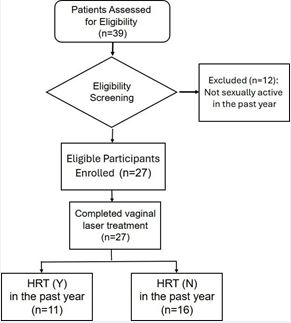
A total of 39 patients were initially assessed for eligibility (Figure 2). Twelve patients were excluded because they had not been sexually active in the past year, leaving 27 participants who were enrolled and completed the full course of vaginal laser treatment.
Figure 2 Study flow diagram Flow diagram showing patient enrollment, exclusion, and subgroup classification according to hormone replacement therapy (HRT) exposure.
The overall mean age of participants was 55.89 years (SD = 5.80), with a range from 46 to 69 years. The mean body mass index (BMI) was 22.88 (SD = 3.68), ranging from 16.0 to 32.5. The mean number of pregnancies was1.44 (SD = 0.89), with a range from 0 to 3.
Participants were further divided into two groups based on whether they had received HRT in the past year: 11 in the HRT group and 16 in the non-HRT group. Among HRT users, the mean age was 55.82 years (SD = 5.17), BMI was 22.22 (SD = 2.52), and gravidity was 1.36 (SD = 1.12).
Among non-users, the mean age was 55.94 years (SD = 6.36), BMI was 23.33 (SD = 4.32), and gravidity was 1.50 (SD = 0.73). Baseline characteristics were comparable between groups (Table 2).
Table 2: Baseline characteristics of study participants
|
|
HRT(Y) (n=11) |
HRT(N) (n=16) |
p-value |
|
Age Mean (SD) |
55.82 (5.17) |
55.94 (6.36) |
0.96 |
|
BMI Mean (SD) |
22.22 (2.52) |
23.33 (4.32) |
0.41 |
|
Gravidity Mean (SD) |
1.36 (1.12) |
1.50 (0.73) |
0.70 |
Baseline demographic and clinical characteristics of participants stratified by recent HRT exposure.
Independent-samples t-tests indicated no statistically significant differences between the two groups in age (p = 0.959), BMI (p = 0.406), or gravidity (p = 0.704), confirming that baseline characteristics were comparable.
Improvement in PISQ-12 short form
Among all 27 participants, vaginal laser treatment led to a significant improvement in sexual quality of life, as measured by the PISQ-12 short form questionnaire.
The overall mean PISQ-12 short form score increased from 9.85 (SD = 4.70) before treatment to 12.67 (SD = 3.50) after treatment. A paired-samples t-test confirmed this improvement was statistically significant, t(26) = -3.113, p = 0.004.
Further analysis was conducted based on whether the patients had undergone HRT in the past year. In the non- HRT group (n = 16), the mean PISQ-12 short form score improved from 10.50 (SD = 4.02) to 13.31 (SD = 2.21), with a mean difference of -2.81 (SD = 3.71), which was statistically significant, t(15) = -3.033, p = 0.008. In the HRT
group (n = 11), the mean score increased from 8.91 (SD = 5.61) to 11.73 (SD = 4.78), with a similar mean difference of -2.82 (SD = 6.06), though this change did not reach statistical significance, t(10) = -1.542, p = 0.154 (Table 3).
Table 3: Improvement in PISQ-12 short form scores before and after treatment
|
|
Number of participants |
Pre- treatment Mean (SD) |
Post- treatment Mean (SD) |
Mean Difference (SD) |
p-value |
|
Total |
27 |
9.85 (4.70) |
12.67 (3.50) |
2.81 (3.62) |
0.004 |
|
HRT(Y) |
11 |
8.91 (5.61) |
11.73 (4.78) |
2.82 (6.06) |
0.154 |
|
HRT(N) |
16 |
10.50 (4.02) |
13.31 (2.21) |
2.81 (3.71) |
0.008 |
Comparison of PISQ-12 short form scores before and after vaginal laser therapy, stratified by recent HRT exposure.
These findings suggest that vaginal laser therapy was associated with improved sexual quality of life across the entire cohort, with statistically significant improvements observed particularly in those who had not received hormone therapy in the past year.
Improvement in Sexual satisfaction VAS Score
Longitudinal changes in Sexual Satisfaction VAS Scores were evaluated using repeated-measures ANOVA across four time points: prior to treatment, three months after the initiation of treatment (i.e., upon completion of all three vaginal laser sessions), six months after treatment initiation, and one year after treatment initiation. Scores at follow-up were obtained through structured telephone interviews with the participants. At the one-year assessment, 6 women were lost to follow-up, resulting in a final analytic sample of 9 in the HRT group and 12 in the non-HRT group.
In the HRT group (n = 9), mean scores increased from
3.11 (SE = 0.59) prior to treatment to 5.22 (SE = 0.74) at three months, followed by a decline to 4.44 (SE = 0.67) at six months and 4.56 (SE = 0.80) at one year. The repeated- measures ANOVA indicated no statistically significant effect of time (p = 0.24).
In contrast, the non-HRT group (n = 12) showed a sustained improvement over time, with mean scores increasing from 3.83 (SE = 0.42) prior to treatment to6.33 (SE = 0.54) at three months, peaking at 7.08 (SE = 0.63) at six months, and slightly decreasing to 6.33 (SE = 0.60) at one year (Table 4). The overall effect of time was statistically significant (p < 0.001). Post-hoc pairwise comparisons demonstrated that scores at three months (p = 0.005), six months (p = 0.007), and one year (p = 0.001) were all significantly higher compared with baseline.
Table 4: Longitudinal changes in Sexual Satisfaction VAS scores.
|
|
Pre-treatment Mean (SE) |
Post-treatment (3m after initiation) Mean (SE) |
Post-treatment (6m after initiation) Mean (SE) |
Post-treatment (1y after initiation) Mean (SE) |
p-value |
Post-hoc |
|
HRT(Y) (n=9) |
3.11 (0.59) |
5.22 (0.74) |
4.44 (0.67) |
4.56 (0.80) |
0.24 |
- |
|
HRT(N) (n=12) |
3.83 (0.42) |
6.33 (0.54) |
7.08 (0.63) |
6.33 (0.60) |
<0.001 |
Post>pre (p= 0.005) |
|
6m>pre (p= 0.007) |
||||||
|
12m>pre (p=0.001) |
Mean Sexual Satisfaction VAS score at baseline, 3, 6, and 12 months following vaginal laser therapy, stratified by HRT exposure.
DISCUSSION
Based on the results of our study, we confirmed that vaginal laser therapy is a highly effective treatment option for GSM. In a prospective study involving 102 women with moderate to severe GSM, fractional microablative CO? laser therapy achieved symptomatic improvement in 84% of participants, with sustained benefits in sexual quality of life, dyspareunia, bladder control, and vaginal lubrication lasting for 12–24 months [8]. Likewise, a comprehensive review of both Er: YAG and CO? vaginal laser modalities concluded that these energy-based interventions effectively restore vaginal health, alleviate vulvovaginal atrophy (VVA) symptoms, and enhance sexual function in postmenopausal women, including breast cancer survivors [9]. Taken together, our findings and previous reports provide strong evidence for both the therapeutic efficacy and long-term stability of vaginal laser therapy in GSM management.
Our results further indicate that the beneficial effects of vaginal laser therapy on GSM symptoms can be sustained for at least one year post-treatment, with particularly robust responses observed in patients who had not received HRT in the past year. This is consistent with prior findings from Sokol et al. [10], who reported that fractional CO? laser treatment yielded significant improvements in vaginal pain, burning, itching, dryness, dyspareunia, and overall sexual function at 3 months, and these gains remained statistically significant at the 1-year follow-up, with patients maintaining comfort with vaginal dilators and expressing high satisfaction rates (~92%). Similarly, Schachar et al., conducted a prospective CO? laser study in a cohort of postmenopausal women, observing sustained significant improvements in both subjective assessments (e.g., VAS-VA, SAVQ, mVSQ, PISQ-12) and objective indices (Bachmann Vaginal Health Index and Vaginal Health Assessment) from baseline through one year after treatment completion. Moreover, histological evaluation in that study revealed evidence of neovascularization without worsening of epithelial atrophy, supporting both the efficacy and histologic safety of laser treatment over the long term [11].
The mechanisms of action of vaginal laser therapy and HRT are fundamentally different, which may be one of the reasons for the observed differences in treatment response. Vaginal laser therapy primarily promotes mucosal tissue remodeling through minimally invasive photothermal effects, leading to epithelial thickening, neovascularization, and collagen neosynthesis, thereby enhancing mucosal elasticity, hydration, and thickness. Histological studies have demonstrated that, following treatment, the number of epithelial cell layers increases, glycogen content is enhanced, and connective tissue papillae and neovascularization are observed [12]. In contrast, the therapeutic effects of HRT are mainly mediated through estrogen receptor–dependent pathways, which promote epithelial cell proliferation, increase vascular density and hydration, and improve mucosal metabolism and structural integrity. Evidence indicates that local vaginal estrogen therapy can restore vaginal pH to the acidic range typical of the reproductive years, stimulate epithelial maturation with glycogen-rich superficial cells, and enhance vaginal blood flow, elasticity, and lubrication, thereby alleviating GSM symptoms such as dryness and dyspareunia [13,14].
Due to these mechanistic differences, patients who have already received HRT may have mucosa in a relatively more optimal baseline condition, thereby limiting the additional tissue restoration achievable through laser therapy. This pattern was evident in our study, where the HRT group showed numerical improvement after treatment but did not reach statistical significance, suggesting a possible ceiling effect. Previous research has also reported that when estrogen therapy has already optimized mucosal lubrication and elasticity, the incremental benefit of subsequent laser treatment in these specific domains may be limited [15].
Another possible factor influencing treatment outcomes is that patients who respond poorly to HRT may also derive limited benefit from vaginal laser therapy. Poor responsiveness of the vaginal mucosa, epithelial thickness, or blood flow to estrogen may reflect more advanced tissue degeneration, thereby reducing responsiveness to non-hormonal treatments such as laser therapy. Potential mechanisms include decreased estrogen receptor sensitivity (e.g., with advanced age or prolonged postmenopausal status), severe tissue atrophy with limited repair capacity, and chronic inflammation or altered immune status. The literature also supports the importance of baseline tissue status in determining treatment response. Sokol et al. [10], reported that while laser therapy is effective for moderate-to-severe GSM, its benefits are limited in women with very severe symptoms or those unresponsive to other treatments. Portman et al. [16]. similarly emphasized that individual factors such as age, medical history, and tissue characteristics influence treatment outcomes. As our study classified participants only by whether they had used HRT in the past year, without data on actual clinical response, type, duration, or continuity of HRT use, we could not directly confirm this hypothesis.
The strength of this study lies in the use of a standardized treatment protocol, as all patients underwent vaginal laser therapy using the same SmartXide² Laser System. This minimized variability associated with different devices and consumables. Additionally, the data were derived exclusively from local Taiwanese patients, which reduced potential confounding factors related to ethnicity and lifestyle, and enhanced the applicability of the findings to the local population. However, several limitations should be noted. First, this was a single-center study with a relatively small sample size, and it focused exclusively on postmenopausal women, which may limit the generalizability of the results. Second, the study did not further analyze the specific types or duration of hormone therapy used, which may have influenced the treatment response in the subgroup analysis. Third, sexual quality of life was assessed using self-reported questionnaires, which may be subject to response bias. Lastly, only short-term outcomes were evaluated; thus, the long-term efficacy and safety of vaginal laser therapy remain to be established.
CONCLUSION
This study demonstrated that fractional CO? vaginal laser therapy significantly improved sexual quality of life in postmenopausal women with genitourinary syndrome of menopause (GSM). Improvements were observed in both PISQ-12 short form and Sexual Satisfaction VAS scores, with more consistent and sustained benefits in women without recent hormone replacement therapy (HRT) exposure. These findings suggest that vaginal laser therapy may be a valuable non-hormonal therapeutic option, particularly for patients who are unsuitable for or unresponsive to HRT. Nevertheless, the retrospective design, single-center setting, small sample size, and limited follow-up period constrain the generalizability of the results. Larger multicenter prospective studies with longer follow-up are warranted to confirm the long-term efficacy and safety of this modality.
ACKNOWLEDGMENTS
The authors thank Chang Mei-Ju for her assistance in collecting the raw data for this study. This research received no external funding.
REFERENCES
- Carlson K, Nguyen H. Genitourinary syndrome of menopause. In: StatPearls. 2024.
- Wasnik VB, Acharya N, Mohammad S. Genitourinary Syndrome of Menopause: A Narrative Review Focusing on Its Effects on the Sexual Health and Quality of Life of Women. Cureus. 2023; 15: e48143.
- Angelou K, Grigoriadis T, Diakosavvas M, Zacharakis D, AthanasiouS. The Genitourinary Syndrome of Menopause: An Overview of the Recent Data. Cureus. 2020; 12: e7586.
- Palacios S, Cancelo MJ, Castelo Branco C, Llaneza P, Molero F, Borrego RS. Vulvar and vaginal atrophy as viewed by the Spanish REVIVE participants: symptoms, management and treatment perceptions. Climacteric. 2017; 20: 55-61.
- Christmas M, Huguenin A, Iyer S. Clinical Practice Guidelines for Managing Genitourinary Symptoms Associated With Menopause. Clin Obstet Gynecol. 2024; 67: 101-114
- Paraiso MFR, Ferrando CA, Sokol ER, Rardin CR, Matthews CA, KarramMM, et al. A randomized clinical trial comparing vaginal laser therapy to vaginal estrogen therapy in women with genitourinary syndrome of menopause: The VeLVET Trial. Menopause. 2020; 27: 50-56.
- Salvatore S, França K, Lotti T, Parma M, Palmieri S, Candiani M, et al. Early Regenerative Modifications of Human Postmenopausal Atrophic Vaginal Mucosa Following Fractional CO2 Laser Treatment. Open Access Maced J Med Sci. 2018; 6: 6-14.
- Fariba Behnia-Willison, Sara Sarraf, Joseph Miller, Behrang Mohamadi, Alison S. Care, Alan Lam, et al. Safety and long-term efficacy of fractional CO? laser treatment in women suffering from genitourinary syndrome of menopause. Eur J Obstet Gynecol Reprod Biol. 2017; 213: 39-44.
- Gambacciani M, Levancini M, Cervigni M. Vaginal erbium laser: the second-generation thermotherapy for the genitourinary syndrome of menopause. Climacteric. 2015; 18: 757-763.
- Sokol ER, Karram MM. Use of a novel fractional CO2 laser for the treatment of genitourinary syndrome of menopause: 1-year outcomes. Menopause. 2017; 24: 810-814.
- Schachar J, Devakumar H, Martin L, Hurtado EA, Davila GW. Prospective study of fractional carbon dioxide laser therapy for symptoms of genitourinary syndrome of menopause: one-year follow-up. J Clin Gynecol Obstet. 2021; 10: s11-17.
- Tomczyk K, Chmaj-Wierzchowska K, Wszo?ek K, Wilczak M. New possibilities for hormonal vaginal treatment in menopausal women. J Clin Med. 2023; 12: 4740.
- Roloff KL. Vaginal estrogen: an option to be considered for postmenopausal women. Women’s Healthcare. 2022; 10: 30-35.
- Phillips NA, Bachmann GA. Genitourinary syndrome of menopause: common problem, effective treatments. Cleve Clin J Med. 2018; 85: 390-398.
- Pagano T, De Rosa P, Vallone R, Schettini F, Arpino G, De Placido S, et al. Fractional microablative CO2 laser for vulvovaginal atrophy in women treated with chemotherapy and/or hormonal therapy for breast cancer: a retrospective study. Menopause. 2016; 23: 1108-1113.
- Portman DJ, Gass ML; Vulvovaginal Atrophy Terminology Consensus Conference Panel. Genitourinary syndrome of menopause: new terminology for vulvovaginal atrophy from the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. Menopause. 2014; 21: 1063-1068.