Treatment of Buried Penis Using Cosmetic Penile Enhancement Implant, Himplant™
- 1. Emeritus, Department of Urology, Cedars-Sinai Medical Center, USA
- 2. Institute for Urologic Excellence, La Quinta, USA
- 3. Department of Urology, University of Minnesota, USA
Abstract
Buried penis is a condition in which the penile shaft is concealed by surrounding tissues, leading to physical, functional, and psychological challenges for affected individuals. While obesity and excessive suprapubic fat are the primary risk factors in adult-acquired cases, additional factors such as post circumcision complications and connective tissue disorders also contribute. Conservative measures, including weight loss and psychological support, often fall short in addressing the anatomical barriers, necessitating surgical intervention. This study evaluates the efficacy of Himplant™, a medical-grade silicone penile prosthesis, as a novel corrective option for buried penis, without concurrent suprapubic fat removal. Twelve patients underwent the procedure, reporting statistically significant improvements in penile visibility, girth, and length, alongside enhanced self-confidence and sexual satisfaction. Postoperative complications were minimal and managed conservatively, with no cases of implant infection or removal. These findings suggest that Himplant™ offers a promising surgical alternative for the long-term management of buried penis, with potential to improve patient quality of life both physically and psychologically
Citation
Elist J, Wilson SK, Tajkarimmi K, De Fazio A, Amirazodi K (2025) Treatment of Buried Penis Using Cosmetic Penile Enhancement Implant, Himplant™. JSM Sexual Med 9(2): 1152.
INTRODUCTION
Buried penis is a condition characterized by the partial or complete concealment of the penile shaft by the surrounding suprapubic abdominal tissue. The penile shaft is essentially retracted into the body and described in the medical literature as pubic recession of the penis or retractile penis [1]. Buried penis is distinct from the condition of micropenis, which is defined by a stretched penile length less than 2.5 standard deviations of the mean value for a given age group (9.3 cm or less in adult populations) [2]. Buried penis can result from both congenital and acquired etiologies [3, 4], with this article specifically focusing on the latter in adult male populations.
Obesity has been identified as the most significant risk factor for adult-acquired buried penis, with excess adipose tissue in the pubic region contributing to the concealment of the penis [5]. While obesity is not the sole predictor of the condition, nearly 87% of patients undergoing treatment for buried penis are classified as obese based on their body mass index (BMI) [6,7]. As obesity rates continue to increase in Western populations [8], the incidence of buried penis can be expected to rise correspondingly, presenting an escalating challenge for urologists and plastic surgeons.
Additional risk factors for acquiring the condition include excessive skin removal during circumcision, penoscrotal lymphedema, and dysgenic dartos fascia [6,9,10].
Men affected by buried penis experience a range of physical and psychological challenges. The most common reasons for seeking surgical consultation in buried penis patients are sexual dysfunction, issues with urination, difficulty with genital hygiene, and poor self-image [11,12]. Erectile dysfunction is common in individuals with buried penis, as the surrounding tissue can interfere with normal penile function and contribute to inability to achieve or maintain an erection and perform sexual activity [13]. With respect to urination, Amend et al. reported that 19 of 20 patients with buried penis experienced urinary complications such as incontinence, incomplete bladder emptying, dysuria, and urinary spray [14]. These complications, combined with restricted penile accessibility, hinders hygiene. Furthermore, individuals with buried penis may have psychological distress, poor self-image, and diminished self-esteem [12]. This can result in social withdrawal, decreased sexual confidence, and eventually depression.
Conservative treatment options for individuals with buried penis are limited. Physicians typically focus on weight loss, skin infection management, and psychological support [21]. However, prior weight gain in these patients often leads to significant fat accumulation in the Mons pubis (the pubic fat surrounding the penis), which is particularly resistant to reduction through weight loss alone [15,21]. Much of the pubic fat remains even after diligent weight loss [16,17]. Patients may choose to undergo other surgical interventions such as skin grafting, scrotoplasty, suprapubic lipectomy, escutcheonectomy, or abdominal panniculectomy based on the severity of the condition [9,11,13].
Himplant™ (International Medical Devices Inc., Beverly Hills, CA, USA), formerly known as Penuma™, is a penile prosthesis made of medical-grade silicone (Figure 1).
Figure 1 : Himplant
It has received four 510(k) clearances from the U.S. Food and Drug Administration (FDA) for the cosmetic correction of penile soft tissue deformities and cosmetic penile augmentation [18, 19]. The implant is usually used for young men who perceive they possess a smaller penile size in comparison to other men and wish to enhance visibility flaccid length, flaccid girth, and erect girth [20].
A previous study introduced the subcutaneous penile implant, Penuma™, as a safe and effective option for augmenting flaccid penile dimensions in individuals with retractile penis [1]. While this previous study demonstrated the potential of subcutaneous penile implants to correct buried penis, two of the three patients also underwent concurrent suprapubic lipectomy. Our study investigates the efficacy of Penuma™’s enhanced successor, Himplant™, as a standalone corrective measure for buried penis, without the use of additional surgical intervention reducing Mons pubis fat. Additionally, a significantly larger sample size is incorporated
SUBJECTS AND METHODS
Written and verbal consent was obtained from all patients, who were thoroughly informed of the potential benefits, risks, complications, and alternatives, including lifestyle changes to promote weight loss and/or opting not to undergo surgery. Institutional Review Board approval was obtained for the reporting of all outcomes related to Penuma™/Himplant™ procedures. Patients also signed informed consent forms authorizing the publication of this study and its associated images. All procedures were performed between January 2023 and May 2024.
This study presents twelve patients who underwent Himplant™ insertion as a surgical treatment for their buried penis condition. Each patient sought the Himplant™ to unbury his penis resulting in greater visibility and increased girth of the penile shaft. Collectively, all patients reported low self-confidence related to their penile appearance. Preoperative and postoperative physical measurements of midshaft penile length and dorsal penile girth using a paper ruler were performed.
Strict exclusion criteria were applied to ensure patient safety; men were excluded if they had an uncircumcised penis, a history of cosmetic penile injections, a need for non interruptible anticoagulant medications, or an inability to cease smoking for 30 days before and after the procedure. We believe these factors can increase complications during surgery and prolong the recovery period.
CLINICAL COURSE
Preoperative assessment of each patient’s height and weight was conducted, and BMI was calculated. All patients had attempted conservative measures to manage their condition, including lifestyle changes (diet and exercise) to reduce suprapubic fat and better expose the penis; these efforts were unsuccessful, leading them to opt for surgical intervention.
The Himplant™ is a penile prosthesis composed of medical-grade silicone, implanted subcutaneously underneath the penile skin through a high scrotal incision [20,]. The prosthesis features a wall thickness that varies longitudinally from 1.5 to 2.5 cm and is available in three lengths: 14, 16, and 18 cm. The appropriate implant size for each patient was determined intraoperatively based on penile measurements. All patients had a Jackson Pratt (JP) drain placed exiting from the left inguinal area to allow fluid drainage and avoidance of hematoma or seroma formation. The JP drain was assessed during each postoperative follow-up and removed once the drained fluid had significantly decreased. All patients had their drain removed within six days of their procedure date.
Postoperative monitoring included weekly evaluations for the first two months and periodic follow-ups through in-person appointments, virtual consultations, and email thereafter. During the initial two month period, patients were restricted from sexual activity; clearance for sexual activity was most frequently issued eight weeks postoperatively.
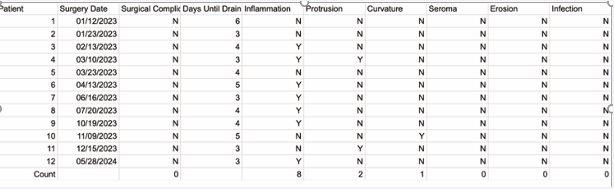
Complications during the postoperative period were monitored and recorded in Table 1.
Table 1 Clinical course
The most frequently observed complication was penile and scrotal swelling, occurring in eight out of twelve patients. All cases were effectively managed using conservative measures, including icing of the suprapubic region, application of a compression sleeve around the penile shaft, and elevation of the penis during sleep. Notably, there were no reports of persistent edema lasting longer than four weeks following these interventions.
Two patients experienced a midshaft protrusion of the implant, creating a palpable edge along the penile shaft. Although this was a cosmetic concern due to its potential impact on the aesthetic outcome, the protrusions were located along the midshaft and did not indicate compromised sutures at the distal end of the implant. Patients were advised to continue the use of the compression sleeve throughout the day to alleviate the protrusion. Over time, both cases showed significant improvement as the prosthesis encapsulated, minimizing the prominence of the protrusion.
There was one reported case of leftward penile deviation developing during the recovery period. The patient was instructed to dress their penis opposite the curve in briefs type underwear. While this did diminish the curvature, a mild degree did remain and was not completely resolved.
There were no instances of severe complications, such as prolonged seroma formation, implant erosion, or device infections, all of which usually require implant removal.
RESULTS
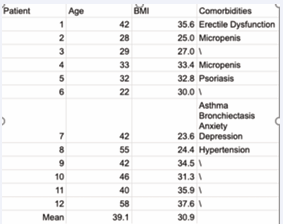
Twelve patients were included in the study, with an age range of 22–58 years and a mean age of 39.1 years. The cohort had a mean BMI of 30.9, with nine patients (75%) meeting criteria for obesity (BMI ≥ 30). Six patients (50%) presented with notable comorbid conditions, including erectile dysfunction, micropenis, and depression (Table 2).
Table 2 : Patient characteristics
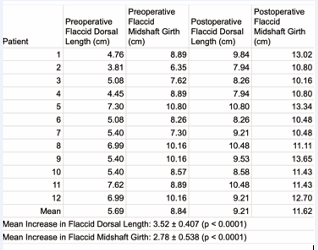
All participants experienced statistically significant increases in both flaccid dorsal length and flaccid midshaft girth following the intervention. Mean flaccid dorsal length increased by 3.52 ± 0.41 cm, while flaccid midshaft girth showed a mean increase of 2.78 ± 0.54 cm (p < 0.0001 for both parameters, Table 3).
Table 3: Pre and Post Operative penile measurements
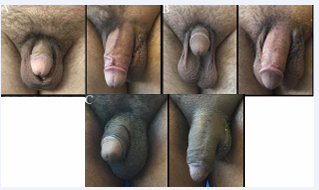
Measurements and photos were obtained preoperatively and on the day of drain removal (Figure 2).
Figure 2 : Pre-op and 4 day post-op front view of flaccid penis. Figure 2A: Patient 3. Figure 2B: Patient 5. Figure 2C: Patient 8.
Physical examination at the time of drain removal confirmed appropriate implant positioning along the penile shaft and full preservation of penile mobility in all cases.
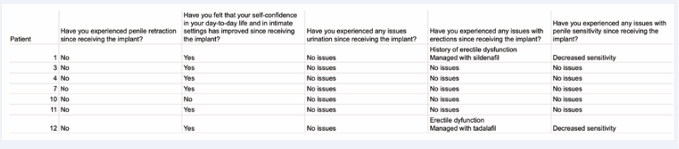
Patient-reported outcomes were assessed via follow up questionnaires, with a response rate of 58% (7/12). The median follow-up period among respondents was 16.5 months. Patients were asked about recurrence of penile retraction, changes in self-confidence, and any functional complications related to urination, erection, or sensitivity. Detailed outcomes from the questionnaire are presented in Table 4.
Table 4 : Questionnaire data
DISCUSSION
Reducing abdominal and suprapubic fat through lifestyle modifications alone is generally insufficient to adequately expose the buried penis. Although weight loss can lead to overall fat reduction, the suprapubic fat pad remains notably resistant to these changes, largely due to hormonal influences [15]. Weight gain in the Mons pubis and chronic obesity can compromise the dartos fascia which connects penile skin to the deep fascia surrounding the suspensory ligament resulting in retraction of the penis [9,10,17]. While counseling may help improve self-confidence and conservative measures can be taken to reduce body fat, these methods are ineffective in addressing the underlying anatomical concealment. Given these limitations, surgical interventions tend to be the only viable option that can directly address the anatomical barriers to penile exposure.
Surgical interventions for buried penis, including penile shaft reconstruction using skin grafting, suprapubic fat pad excision, and abdominal panniculectomy, are among the most commonly employed techniques [11,13]. However, prior studies have reported recurrence rates ranging from 21.7% to 25% within the first 12 months postoperatively, alongside complication rates necessitating surgical revision in 7.1% to 13.3% of cases [11,21]. These outcomes highlight a need for a safer, more effective surgical technique.
This study evaluated the outcomes of Himplant™ placement in twelve men suffering from adult-acquired buried penis. Until our original study of correcting buried penis with Himplant™ [1], the primary indication for the device was to cosmetically enhance the penis by increasing flaccid length and overall girth [20]. Two of the three patients in the initial study from 2020 also had liposuction of the Mons Pubis. None of the patients in this study had liposuction and achieved satisfactory improvement in the length of the visible penis without additional manipulation of infrapubic fat. Our results suggest Himplant™ placement may serve as a viable surgical solution for achieving anatomical correction in cases of buried penis without the need for adjunctive liposuction of infrapubic fat. One deficiency of this study is the lack of longer follow-up to assess the durability of the correction of buried penis by the subcutaneous penile implant.
Among the twelve patients included in this study, there were no instances of complications such as seroma, erosion, or infection that required additional surgery. Comparatively, a previously published study evaluating the use of Penuma™ for cosmetic augmentation of the flaccid penis in a cohort of 400 patients reported acceptable complication rates. The most common postoperative complications in that study included seroma (4.8%), scar tissue formation (4.5%), and infection (3.3%), with infection being the only adverse event necessitating device removal [20]. The absence of complications in the present study, combined with the low rates of severe events reported in similar research, underscores the early safety of the implanted patient from revision surgery.
Of the seven respondents to the follow-up questionnaire, six (85.7%) reported improved self-confidence in both daily activities and sexual encounters. No issues with urination were reported by participants who responded to the follow-up questionnaire. Instances of negative changes in erection maintenance were rare and, in these cases, were effectively managed using phosphodiesterase-5 inhibitors. Notably, no cases of buried penis recurrence were observed within the follow-up period of up to 18 months. These findings suggest that the Himplant™ insertion is effective in mitigating both the psychological and physical challenges associated with buried penis, thereby enhancing overall quality of life.
The most significant concern reported was changes in penile sensitivity. The insertion of Himplant™ and eventual encapsulation of the implant may lead to stretching of the penile skin or nerves, similar to the effects observed with breast implants [22,23]. This can result in transient or, in rare cases, persistent hyposensitivity. While sensitivity often improves as post-operative swelling and inflammation subside and the body adapts to the implant, it is essential for physicians to counsel patients on the potential for long-term changes in sensitivity. Additionally, management strategies should be discussed as part of the preoperative consultation to ensure informed consent and decision-making.
The subcutaneous soft silicone Himplant™ provides therapeutic benefits for patients with buried penis by offering structural support that enhances penile girth and flaccid length while stabilizing the shaft against retractile forces from surrounding tissue. The implant extends the penile shaft beyond the mons pubis, resulting in immediate postoperative improvements in both appearance and functional positioning. These benefits typically become more pronounced over 12 to 18 months postoperatively as natural tissue encapsulation around the device and the implant’s weight contribute to loosening of the suspensory ligament, further externalizing the penile shaft (Figure 3).
Figure 3 : Front view of flaccid penis of patient 7. Figure 3A: 1 day pre-op. Figure 3B: 3 days post-op. Figure 3C: 23 weeks post-op.
Patients should continue to be encouraged to adopt healthy lifestyle choices, including weight loss strategies, during this period to optimize outcomes.
A standardized classification system for assessing the severity of buried penis has yet to gain widespread acceptance, despite efforts such as the Pariser-Santucci classification system [24], and the framework proposed by Tausch et al. [25]. The spectrum of buried penis severity complicates treatment standardization, and prior studies, including those by Falcone et al., have evaluated various surgical techniques (excluding Himplant™ insertion) for its correction [11, 21]. While these studies demonstrated symptomatic improvements, the high variability in outcomes and significant complication rates underscore the need for more effective surgical methods. The absence of severe complications and recurrence in the current study suggests that Himplant™ insertion may be a promising, long-term corrective option for treating buried penis.
A limitation of our study is that it is a retrospective, single-center design with one surgeon. While our early results are promising, there is a need for a prospective, multi-centric approach to validate the efficacy of Himplant™ placement in this patient population. Additionally, comparative studies examining Himplant™ insertion against traditional surgical options would provide further insights into its effectiveness in managing buried penis.
CONCLUSION
The findings of this study demonstrate that Himplant™ is a safe and effective surgical solution for the treatment of adult-acquired buried penis. Patients achieved notable improvements in penile dimensions and psychological well-being without the need for adjunctive liposuction. Minimal postoperative complications and an absence of recurrence within the follow-up period underscore the procedure’s durability. Future studies should focus on multicenter trials and direct comparisons with other surgical approaches to further validate these promising results.
REFERENCES
- Elist JJ, Baniqued M, Steven KW, Hosseini A. Correction of retractile penis with subcutaneous soft silicone penile implant. Int J Impot Res. 2020; 32: 317-322.
- Lee PA, Mazur T, Danish R, Amrhein J, Blizzard RM, Money J, et al. Micropenis. I. Criteria, etiologies and classification. Johns Hopkins Med J. 1980; 146: 156-163.
- Redman JF. Buried penis: congenital syndrome of a short penile shaftand a paucity of penile shaft skin. J Urol. 2005; 173: 1714-1717.
- Pestana IA, Greenfield JM, Walsh M, Donatucci CF, Erdmann D. Management of “buried” penis in adulthood: an overview. Plast Reconstr Surg. 2009; 124: 1186-1195.
- Cohen PR. Adult Acquired Buried Penis: A Hidden Problem in Obese Men. Cureus. 2021; 13: 13067.
- Higuchi TT, Yagamuchi Y, Wood HM, Angermeier KW. Evaluation and treatment of adult concealed penis. Curr Urol Rep. 2012; 13: 277-284.
- Tang SH, Kamat D, Santucci RA. Modern management of adult- acquired buried penis. Urology. 2008; 72: 124-127.
- Boutari C, Mantzoros CS. A 2022 update on the epidemiology of obesity and a call to action: as its twin COVID-19 pandemic appears to be receding, the obesity and dysmetabolism pandemic continues to rage on. Metabolism. 2022; 133: 155217.
- Anandan L, Mohammed A. Surgical management of buried penis in adults. Cent Eur J Urol. 2018; 71: 346-352.
- Alter GJ, Ehrlich RM. A new technique for correction of the hidden penis in children and adults. J Urol. 1999; 161: 455-459.
- Falcone M, Plamadeala N, Cirigliano L, Preto M, Peretti F, Ferro I, et al. The Outcomes of Adult Acquired Buried Penis Surgical Reconstruction. Life. 2024; 14: 1321.
- Voznesensky MA, Lawrence WT, Keith JN, Erickson BA. Patient- Reported Social, Psychological, and Urologic Outcomes After Adult Buried Penis Repair. Urology. 2017; 103: 240-244.
- James R, Stephen L, Michelle Y, Laurence AL. Single Center Outcomes after Reconstructive Surgical Correction of Adult Acquired Buried Penis: Measurements of Erectile Function, Depression, and Quality of Life. J Sex Med. 2014; 11: 1086-1091.
- Amend GM, Holler JT, Sadighian MJ, Rios N, Hakam N, Nabavizadeh B, et al. The Lived Experience of Patients with Adult Acquired Buried Penis. J Urol. 2022; 208: 396-405.
- Sumithran P, Prendergast LA, Delbridge E, Purcell K, Shulkes A, Kriketos A, et al. Long-term persistence of hormonal adaptations to weight loss. N Engl J Med. 2011; 365: 1597-1604.
- Alter GJ. Pubic contouring after massive weight loss in men and women: correction of hidden penis, mons ptosis, and labia majora enlargement. Plast Reconstr Surg. 2012; 130: 936-947.
- Jun MS, Gallegos MA, Santucci RA. Contemporary management of adult-acquired buried penis. BJU Int. 2018; 122: 713-715.
- Food and Drug Administration. Premarket Notification: Silicone Block.
- Food and Drug Administration. Premarket Notification: Pre-formed Penile Silicone Block.
- Elist JJ, Valenzuela R, Hillelsohn J, Feng T, Hosseini A. A Single- Surgeon Retrospective and Preliminary Evaluation of the Safety and Effectiveness of the Penuma Silicone Sleeve Implant for Elective Cosmetic Correction of the Flaccid Penis. J Sex Med. 2018; 15: 1216- 1223.
- Falcone M, Preto M, Timpano M, Oderda M, Plamadeala N, Cirigliano L, et al. The outcomes of surgical management options for adult acquired buried penis. Int J Impot Res. 2023; 35: 712-719.
- Iwahira Y, Nakagami G, Sanada H. Risk factors for capsular contracture after breast reconstruction with tissue expanders and silicone implants in nonirradiated patients: A retrospective observational cohort study. Medicine (Baltimore). 2022; 101: 31837.
- Brown T. Objective Sensory Changes Following Subfascial Breast Augmentation. Aesthet Surg J. 2016; 36: 784-789.
- Pariser JJ, Soto-Aviles OE, Miller B, Husainat M, Santucci RA. A Simplified Adult Acquired Buried Penis Repair Classification System With an Analysis of Perioperative Complications and Urethral Stricture Disease. Urology. 2018; 120: 248-252.
- Tausch TJ, Tachibana I, Siegel JA, Hoxworth R, Scott JM, Morey AF. Classification System for Individualized Treatment of Adult Buried Penis Syndrome. Plast Reconstr Surg. 2016; 138: 703-711.